Closed-circuit anesthesia
Closed-circuit anesthesia refers to a technique in which, during the delivery of an inhalation anesthetic agent using an anesthesia work station (machine) with a circle system, the adjustable pressure relief valve is closed and the fresh gas inflow is adjusted such that it is just sufficient to match the amount of inhaled anesthetic gas and O2 that is taken up by the patient and the amount of gas removed by any side-stream monitors (for measurement of anesthetic gas concentration, CO2, and O2) (Box 13-1). To prevent hypercapnia, a CO2 absorber must be used; all exhaled gases except CO2 are rebreathed when this technique is used. One must ensure that the circuit is free of any leaks (more than 20 potential sites exist for gases to leak from the circuit/system) (Box 13-2).
During the use of a closed-circuit anesthetic, it is important that flowmeters and vaporizers have been calibrated to be accurate at low flows and varying circuit pressures. It may be difficult to deliver the required amount of inhalation anesthetic using this technique with certain vaporizers that are inaccurate at low flow rates (see Box 13-2). If this is the case, one can inject the inhalation anesthetic directly into the expiratory limb of the circle system, but this is rarely done.
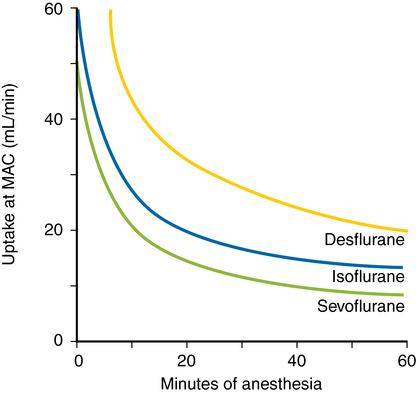
Some major obstacles must be overcome if anesthesia is induced using a closed-circuit anesthesia system (see Box 13-2). Before tissue uptake of the anesthetic can occur, an adequate amount of the inhalation anesthetic must be in the breathing circuit, the patient’s alveoli, and the arterial circulation. During conventional inhalation anesthetic induction, uptake of the inhalation anesthetic agent is greatest during the initial phases of induction; uptake decreases as venous concentration approaches alveolar concentration of the inhalation anesthetic. During induction with a closed-circuit anesthetic, it is difficult to denitrogenate the patient; the N2 that the patient exhales dilutes the breathing circuit, thereby slowing induction and increasing the risk for awareness and, possibly, resulting in delivery of a hypoxic gas mixture.
During closed-circuit anesthesia, O2 is the preferred carrier gas because its uptake is relatively constant. The administration of N2O makes induction more complicated because its uptake follows a power function and requires constant titration during induction and further increases the risk of delivery of a hypoxic gas mixture. To avoid these difficulties, most clinicians use high flows on induction to denitrogenate the breathing circuit and the patient’s functional residual capacity and to establish adequate anesthetic concentrations prior to switching to a closed system (Figure 13-1).