23 Clinical Informatics
Pearls
• Clinical information technology (IT) involves a dynamic set of interactions that all have to be managed effectively. The categories of people, process, and technology each introduce different challenges and factors that must be addressed for successful IT implementation and adoption.
• To achieve maximal beneficial effects, clinical IT must provide clinicians with the right amount of data in the appropriate context to help them make good clinical decisions.
• The use of IT to enforce compliance and adherence to policies and regulations must be balanced with clinical utility and minimal distractions.
• Effective use of clinical IT tools can markedly improve patient safety and clinical workflow.
• Clinical, administrative, and IT leaders need to develop a shared vision and governance model to deploy and maintain clinical IT systems.
Introduction
In the past decade, many examples of error, waste, and inefficiency in healthcare have been identified. In 1999, the Institute of Medicine (IOM) estimated that nearly 100,000 hospitalized patients die each year from medical errors.12 The IOM report led to increased scrutiny of the safety and efficiency of the healthcare system. In 2003, the analysis by McGlynn and others9 documented a significant gap between the care that patients need and the care that is provided. In a sample of more than 6700 adult patients in 12 metropolitan cities, only 54.9% of patients received the recommended care.9
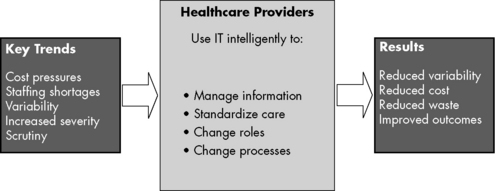
IT is a potential tool to reduce errors. A reduction in errors can result from the role of IT in managing information, its utility in standardizing care, and through its role as a vehicle to change roles and processes in an effort to reduce cost, variability, and waste. These efforts can result in improved outcomes (Fig. 23-1)
Implemention of clinical information systems
In another case, in the first 5 months following implementation of a commercially purchased CPOE system in a pediatric critical care unit at a leading children’s hospital in the northeast, mortality during interfacility patient transfer more than doubled (from 2.8% to 6.6%) when compared with the mortality in the 13 months preceding CPOE implementation.3 Several factors may have contributed to this rise. First, the system was rapidly deployed. Second, the clinical care team was not allowed to enter orders until the patient physically entered the hospital. Third, order sets were not developed to help clinicians rapidly enter common orders. Fourth, simultaneous with the CPOE implementation, the hospital dispensing process for medications was changed. All of these factors directly affected patient care.
A second children’s hospital in the northwest installed the same commercial CPOE system. When the effects of the implementation system on the northwest children’s hospital was studied by Del Beccaro and others,2 they found no difference in mortality in the preimplementation and postimplementation periods.
The Agency for Healthcare Research and Quality (AHRQ) calls for careful and thoughtful implementation of CPOE systems. Koppel’s study of CPOE systems, funded by the AHRQ,7 found two key problem areas in implementation:
• Fragmentation of data among each hospital’s various information systems
• Interface problems between people and machines, particularly when the computer forced people to work in a way that differed from clinical work routines
People, Process, and Technology
Different units in the same hospital will have drastically different acceptance of the same technology as the result of differences in staff perceptions regarding the ease of technology use and also the result of differences in staff attitudes about changes in their practice. Gender and age play important roles in determining these perceptions and attitudes. Karsh4 found that male users valued the usefulness of a tool, whereas female users felt that ease of use was more valuable. Older users focused more on social and process issues, whereas younger users focused more on the effects of the tool on task performance. Therefore before implementing any new technology, planners should evaluate characteristics of potential users and of the potential technology itself.
Best Practices
Feedback
Several signs can predict potential failure of a technology implementation project. These “red flags” were adapted from a study by Upperman and others13 and are summarized in Box 23-1.
Box 23-1 Red Flags for Potential Implementation Failure
• Ignoring anxiety from change
• Not considering the consequences of each process step
• Lack of extensive training in the preimplementation and postimplementation periods
• Inadequate access to computers
• Not understanding the system limitations
• Neglecting to communicate the possible negative effects of information technology as well as the benefits
• Communicating through outside technical consultants rather than in-house leadership
From Upperman JS, et al: The introduction of computerized physician order entry and change management in a tertiary pediatric hospital. Pediatrics 116:e634-e642, 2005
Clinical information systems
The focus on medical safety stimulated by the 1999 Institute of Medicine12 report led to the formation of the Leapfrog Group for Patient Safety. This group consists of many large companies and organizations that pay for healthcare coverage for their employees. The group initially named three key practices that could significantly improve healthcare quality and safety. These three practices are:
2. Evidence-based hospital referral (choice of hospitals and referrals should be based on a hospital’s experience and outcomes, particularly for complex procedures), and
3. Staffing of pediatric critical care units with physicians experienced in critical care medicine
Computerized Provider Order Entry
There are many reasons why CPOE is expected to improve healthcare quality and safety (Box 23-2). CPOE systems can aggregate data for clinical use. Unlike the paper ordering process, a clinician can interact with the system away from the bedside without relying on verbal or telephone orders, which can lead to potential errors. Because communication is electronic, CPOE systems immediately route orders and requisitions to ancillary departments.
Order Sets
Many institutions have already developed treatment protocols in the paper ordering process. These protocols are the best place to begin designing CPOE order sets. Facilities with significant experience with CPOE have found that the energy and resources available during the implementation phase of CPOE wanes over time. During the maintenance phase of the CPOE system, it important to establish a process for periodic review and update of order sets with continued incorporation of the latest evidence from the healthcare literature to guide clinical care (Fig. 23-2)
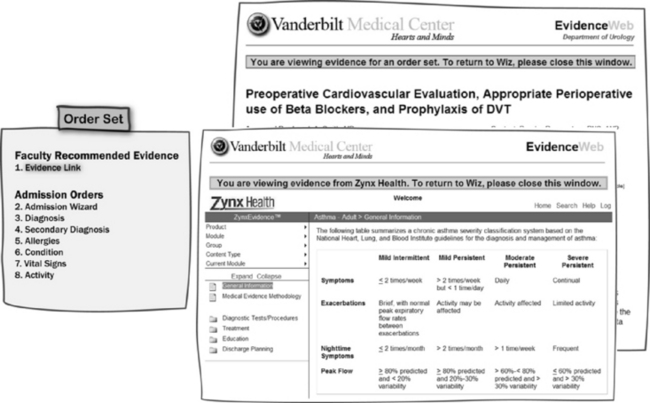
Fig. 23-2 Order sets with links. This diagram shows the relationship among traditional order sets with links to the reference material for evidence-based medicine developed by the Evidence-Based Medicine Team at the Vanderbilt University Medical Center.11a
(Courtesy Zynx Health Incorporated, Los Angeles, CA; and Vanderbilt University Medical Center, Nashville, Tenn.)
The project team can often leverage existing hospital process improvement infrastructure to help establish a systematic process for developing order sets (Box 23-3). The first step in building the infrastructure is to identify the core team that will serve as the resource for the institution. Because order sets can exist for each of the clinical disciplines, it is important for the core team to work with key representatives of the patient care team so that the clinicians have confidence in the process and a sense of ownership of the order set content. Minimizing the time commitment by the clinicians will help retain their engagement. The core team should be responsible for coordinating meetings, collating the necessary documents, and filtering the literature. This process frees the clinicians to focus on important clinical content.
Box 23-3 Sample Evidence-Based Practice Process for Development of Order Sets11a
Input Phase
Development Phase
CPOE, Computerized provider order entry.
Alerts and Cross-Checks
A DDI is any situation in which one drug has the potential to increase or decrease the effect of another drug to an extent that is clinically significant. Ideally, a prescribing clinician is alerted to this possible situation during the order entry process and will be guided toward a better clinical decision. In a study by Ko and others6 of providers and pharmacists who used the U.S. Department of Veterans Affairs CPOE system, most felt that DDI alerts increased the safety of prescribing practice. The caveat from this study was that fewer than one third of the prescribers found that the system gave the essential information necessary to make good decisions. Both the prescribers and pharmacists felt that for DDI alerts to be effective, the system should give more detailed information and should suggest appropriate alternatives.
Pediatric medication safety
There are four steps in medication delivery: prescribing, transcribing, dispensing, and administering. Errors can occur at each step, but approximately 80% of medication errors occur at the prescribing and administering steps1:
Pediatric Medication Dosing
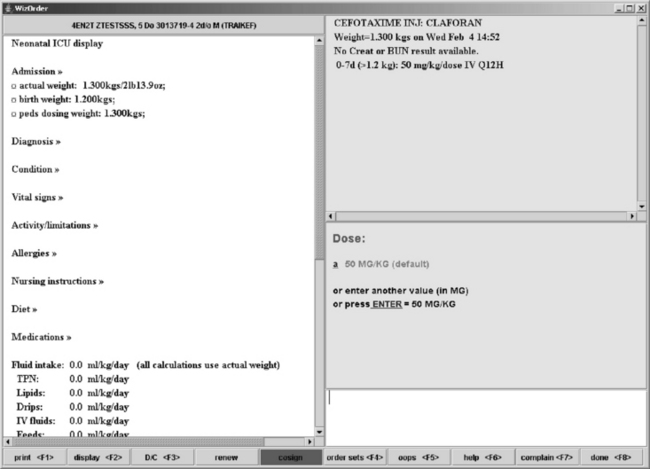
The use of CPOE in the pediatric population requires a special focus on dosing algorithms (Box 23-4). The process of dosing medications for the pediatric patient is distinctly different from the process used in adult patients. Pediatric medication dosing is based primarily on patient weight. In certain subpopulations, dosing differs based on the age of the patient in both chronologic and gestational terms. In neonatal patients, rapid weight changes that are significant as a percent of weight must also be considered. If weight-based dosing is used, some school-aged patients can surpass adult dosing recommendations on a milligram per kilogram basis. A CPOE system must be able to integrate these factors into appropriate decision support (Fig. 23-3).
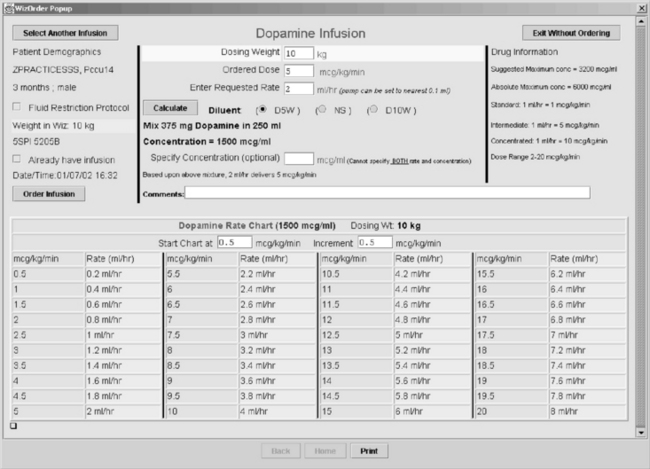
The calculations for both standard and weight-based concentrations, such as the rule of sixes, can lead to confusion and errors. In the paper-based ordering process, prescribers often did not provide the complete information necessary for pharmacists and nurses to cross-check the calculations. A CPOE system with effective clinical decision support can significantly improve the prescribing process for continuous infusions by performing the complex calculations, ensuring completeness of the orders, and producing a titration table against which intravenous pump settings can be compared by nurses administering the drug (Fig. 23-4). This final check by the nurse at the point of care is crucial.
Pediatric Patient Specific Decision Support
When a critical care environment transitions to an electronic ordering system, the project team should evaluate several system features and develop a standardized approach to address common pediatric dosing issues (Box 23-5).
Box 23-5 Key Features of Patient Specific Decision Support
• Provides weight- and age-specific dosing information at the time of ordering
• Menu dose options provided in mg/kg or mg depending on weight of patient
• Calculations performed by the computer
• Only intervals and doses appropriate for the specific patient are presented to the prescriber
Overall, the use of CPOE can be highly effective in reducing medication errors. The presence of advanced decision support markedly improves the utility of CPOE, especially in the care of pediatric patients.11
The Five Rights of Medication Administration
The core checks for appropriate medication administration are the well publicized “five rights” (Box 23-6), which are right patient, drug, dose, route, and time.
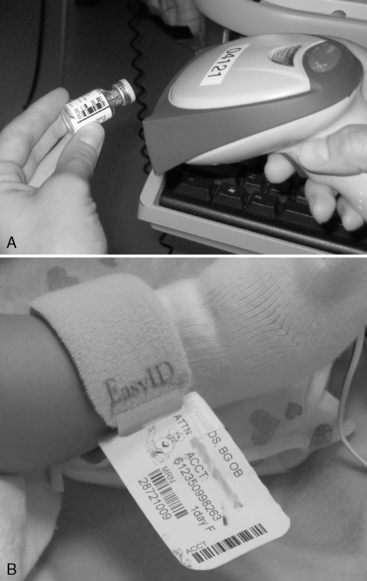
Bar-Coded Medication Administration
The standard process for administering medications requires mental checks of the labeling on the syringe, the medication administration record, and the patient arm band, even after the checks for propriety of drug and dose. Many medications have similar packaging and labeling that can contribute to medication errors.5 There are tragic examples of overdose of drugs such as heparin resulting from such similarities.
The bar-coded medication administration (BCMA) system uses bar code technology to cross-check the patient’s arm band bar code and the drug bar code against a system containing the medication orders for the patient to confirm that the patient should receive that drug in that dose at that time (Fig. 23-5). Alerts should be raised if the orders do not indicate a match of the drug dose, the patient, and the time. The BCMA system requires that all steps be followed and that the provider acknowledge the alerts.
In an evaluation of BCMA use and the types of workarounds that users create, Koppel and others8 were able to group the workarounds into three general categories:
Technology-related causes: issues related to the BCMA application or hardware itself. For example, if the nurse must pass the scanner over the patient or medication bar code several times before scanning is successful, or if there are frequent equipment failures, the system may be perceived as delaying or complicating medication delivery rather than enhancing it.
Task-related causes: issues related to the users workflow. For example, if the nurses are accustomed to routinely discarding drug packaging before bringing the medication to the bedside, and the bar code is located on the packaging, the nurses will have to change practice to avoid delays and rework (e.g., to retrieve the discarded package).
Organizational causes: issues related to inadequate policies, training, staffing or other areas that are governed at an organization level. For example, if the unit dose provided is consistently too large for every pediatric patient, and the nurse must always draw up a tiny fraction of that unit dose, then each time the drug is used there is an opportunity for imprecision in drug dosing or overdose.
Patient-related causes: issues related to patient level logistics. For example, if the patient’s barcode is not accessible (e.g., patient is draped for a sterile procedure), providers will perform overrides or workarounds.
Environmental causes: issues related to the logistics of space, positioning, and location of key items necessary to use BCMA technology. For example, if there are insufficient bar code scanners available for the pediatric critical care unit, or if the medication cabinet and the scanners are stored in different places so that the nurse spends a great deal of time getting the medication and finding a bar code scanner, then these issues will delay medication delivery and complicate the nursing workflow.
Electronic clinical documentation
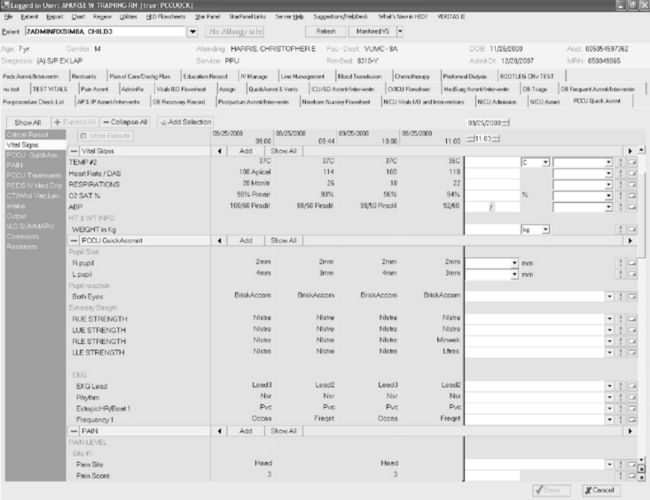
Just as in the use of CPOE for providers, electronic documentation can prompt completeness in charting by nurses (Fig. 23-6). In both the CPOE and electronic documentation, prompts must be used judiciously to minimize disruptions and support effective clinical communication, documentation, and workflow. Effective use of forcing functions requires titrating disruptions to their level of importance for clinical care. Forcing functions should be reserved to prompt entry of data that is essential either for the safety of the patient or to fulfill a regulatory requirement that all agree is a priority.
1 Bates D.W., et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. J Am Med Assoc. 1995;274:29-34.
2 Del Beccaro M.A., et al. Computerized provider order entry implementation: no association with increased mortality rates in an intensive care unit. Pediatrics. 2006;118(1):290-295.
3 Han Y.Y., et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;116(6):1506-1512. Erratum in: Pediatrics 117(2):594, 2005 Feb
4 Karsh B.T. Beyond usability: designing effective technology implementation systems to promote patient safety. Qual Saf Health Care. 2004;13(5):388-394.
5 Kaushal R., et al. Medication errors and adverse drug events in pediatric inpatients. J Am Med Assoc. 2001;285(16):2114-2120.
6 Ko Y., et al. Practitioners’ views on computerized drug-drug interaction alerts in the VA system. J Am Med Inform Assoc. 2007;14(1):56-64.
7 Koppel R., et al. Role of computerized physician order entry systems in facilitating medication errors. J Am Med Assoc. 2005;293(10):1197-1203.
8 Koppel R., et al. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc. 2008;15(4):408-423.
9 McGlynn E.A., et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635-2645.
10 Miller R.A., et al. The anatomy of decision support during inpatient care provider order entry (CPOE): empirical observations from a decade of CPOE experience at Vanderbilt. J Biomed Inform. 2005;38(6):469-485.
11 Potts A.L., et al. Computerized physician order entry and medication errors in a pediatric critical care unit. Pediatrics. 2004;113(1 Pt 1):59-63.
11a Starmer J.M., Pinson C.W., Lorenzi N.M. Informatics and evidence-based medicine: prescriptions for success. In: Safran C., Retl S., Marin H., editors. MedInfo 2010: partnerships for effective health solutions, 13th world congress on medical and health informatics. Amsterdam: IOS Press, 2010.
12 The Institute of Medicine. To err is human: building a safer health system. Washington, DC: National Academy Press; 1999.
13 Upperman J.S., et al. The introduction of computerized physician order entry and change management in a tertiary pediatric hospital. Pediatrics. 2005;116(5):e634-e642.
American Nursing Infomatics Association. http://www.ania.org
The Healthcare Information and Management Systems Society. http://www.himss.org
The Leapfrog Group. http://www.leapfroggroup.org
U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. http://www.healthit.ahrq.gov
U.S. Department of Health and Human Services, Health Information Technology. http://www.healthit.hhs.gov