Clinical examination of the cervical spine
History
Pain
Onset
Next, the following questions are asked about the onset of the pain.
 Pain of cervical origin very often starts at the cervical spine but frequently spreads or shifts to another region quite quickly, so that the cervical source may pass unnoticed.
Pain of cervical origin very often starts at the cervical spine but frequently spreads or shifts to another region quite quickly, so that the cervical source may pass unnoticed.
 Interscapular onset of pain is typical of a lower cervical disc lesion that compresses the dura. In contrast, it is very unusual for pain to begin in the arm. Should this occur, the possibility of a neurofibroma, compressing a nerve root, has to be considered in young people. In the elderly, an osteophyte or even a malignant process is more probable.
Interscapular onset of pain is typical of a lower cervical disc lesion that compresses the dura. In contrast, it is very unusual for pain to begin in the arm. Should this occur, the possibility of a neurofibroma, compressing a nerve root, has to be considered in young people. In the elderly, an osteophyte or even a malignant process is more probable.
Evolution
The localization may change, either because the pain shifts to another place or because it spreads. Pain that spreads and gradually expands over a larger area is typical of an expanding lesion and should always arouse suspicion. On the other hand, pain that shifts from the scapular area to the upper limb is highly indicative of a shifting lesion (or disc lesion). The fragment of disc substance first displaces posterocentrally and compresses the dura mater, which results in central, bilateral or unilateral scapular pain; it then moves laterally and impinges on the dural investment of a nerve root. The scapular pain disappears and is replaced by a radicular pain down the upper limb. In order to interpret the distribution and evolution of the pain correctly, the mechanism of dural pain should be understood. Because the anterior aspect of the dura mater is innervated by a dense network of branches of sinuvertebral nerves originating at several levels, extrinsic compression and subsequent irritation of the dura may give rise to pain felt in several dermatomes. This phenomenon is called ‘multisegmental pain’ and is described in Chapter 1. Because the dural investment of the nerve root is only innervated from its own recurrent nerve, irritation here results in pain strictly felt in the corresponding dermatome, thus strict segmental pain.
Also the duration of the pain is informative. Most benign cervical disorders are intermittent. If pain progressively worsens, then the presence of an irreversible lesion such as metastases must be borne in mind, particularly in the elderly. Root pain as the result of a disc protrusion lasts for a variable but limited period and then ceases as spontaneous remission takes place (see Ch. 8). Hence, root pain that lasts longer than 6 months should arouse suspicion of another, possibly progressive cause.
Current pain
Localization
Headache
Some types of headache can be recognized by paying attention to the history.
Early morning headache in elderly patients is a typical example. The patient wakes every morning with headache and/or occipital pain. After some hours the symptoms ease and have completely disappeared by midday. Symptoms do not recur until the next morning. The sequence is repeated daily without fail and, as the years go by, pain tends to last longer into the day. This type of headache responds spectacularly to manipulative treatment (see p. 201).
Pain in the trapezioscapular area
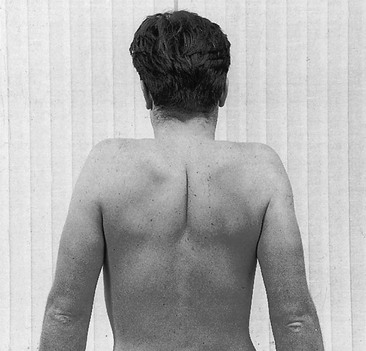
This is the most common pain reference for cervical lesions. The majority of pain in the trapezius or scapular area has a cervical origin, and must usually be considered as the multisegmental reference of a discodural conflict (Fig. 6.1). The pain may be unilateral, bilateral or interscapular. Depending on the patient’s age, it may be intermittent or constant; the older the patient, the more likely the pain will last over longer periods. Upper scapular pain or pain in the trapezius area may also have a C4 segmental origin. Other sources of trapezioscapular pain are a thoracic lesion, a local scapular lesion or a shoulder girdle problem.
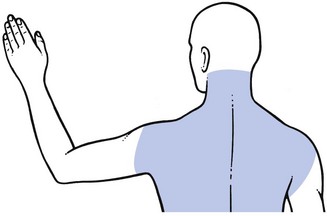
Fig 6.1 Multisegmental scapular pain.
Paraesthesia
Paraesthesia is a very common symptom which may originate from any nerve fibre in the cervicoscapular area or in the arm (Table 6.1). Paraesthesia is often experienced as a ‘pins and needles’ sensation. In other instances, the patient may describe the feeling as ‘numbness’. The moment the patient mentions the presence of such symptoms, the examiner should carefully determine how proximal they are because, as has been explained in Chapter 2, the point of compression always lies proximal to that of the paraesthesia. The lesion may lie at any one of a number of different levels but the vaguer the distribution of the pins and needles, the more proximally the lesion needs to be sought.
Table 6.1
| Level | Cause/site of cause | Symptoms |
| Cervical | Myelopathy: | No pain |
| Intrinsic | Multisegmental paraesthesia on neck flexion | |
| Extrinsic | Lhermitte’s sign | |
| Nerve root | Pain | |
| Segmental paraesthesia | ||
| Compression phenomenon | ||
| Shoulder girdle | Brachial plexus | Vague paraesthesia |
| Release phenomenon | ||
| Arm | Nerve trunk | Defined area of paraesthesia |
| Specific tests | ||
| Nerve ending | Cutaneous analgesia | |
| (Paraesthesia) |
At the shoulder girdle
Lesions of the brachial plexus at the thoracic outlet give rise to paraesthesia in one or both hands and affect all digits. When there is external pressure and because of the release phenomenon, pins and needles are only felt after the compression has ceased (see Ch. 2). They are often nocturnal, waking the patient after some hours’ sleep.
Vertigo or symptoms related to the vertebral artery
It is well known that vertigo may be the consequence of vertebrobasilar vascular insufficiency. However, cervical disorders without any impairment of the vertebral artery can also give rise to vertigo. The explanation is that the cervical spine, together with the eyes and the labyrinths of the ear, is an important source of proprioceptive information that influences the sense of balance. When vertigo is a dominant symptom, the examiner must carefully look for its origin, especially if a manipulative treatment is considered (see Ch. 11).
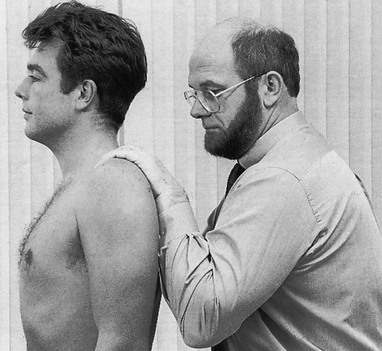
Inspection
Inspection and examination are performed on the standing patient. The examiner stands behind the patient and looks at the neck and scapular region. First the posture of neck and head is observed. The head should be in the midline, with the chin above the manubrium. A normal neck shows a slight lordotic curve. Loss of the lordotic curve, with the head fixed in flexion, suggests a block at the back of an intervertebral joint and is most common after whiplash injuries. Next, neck length is ascertained. A short neck is present in Klippel–Feil syndrome (due to fusion of several vertebrae)1 and a webbed neck in a girl is typical of Turner’s syndrome.2 Then the examiner notices if the head is tilted or rotated in one direction, which indicates torticollis. A careful analysis of the torticollis is then made. The neck may be held in lateral deviation or in a combined position of lateral deviation and rotation. The lateral tilt as well as the rotation can be towards or away from the painful side. In acute discodural torticollis, the head is usually deviated in lateral flexion away from the painful side. There is usually no fixation in rotation. Shortening of the sternocleidomastoid muscle (congenital or acquired) leads to a deviation of the head in lateral flexion towards the pain combined with rotation to the other side (see Ch. 8).
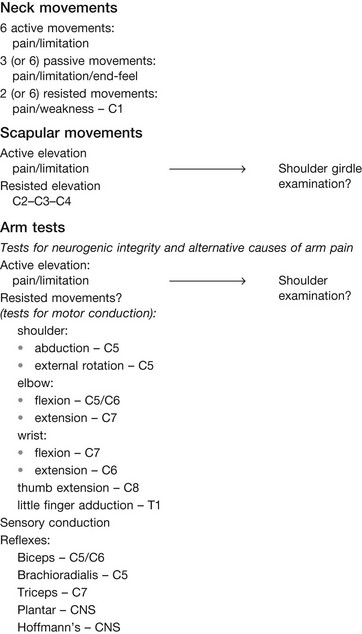
Functional examination 
Neck movements
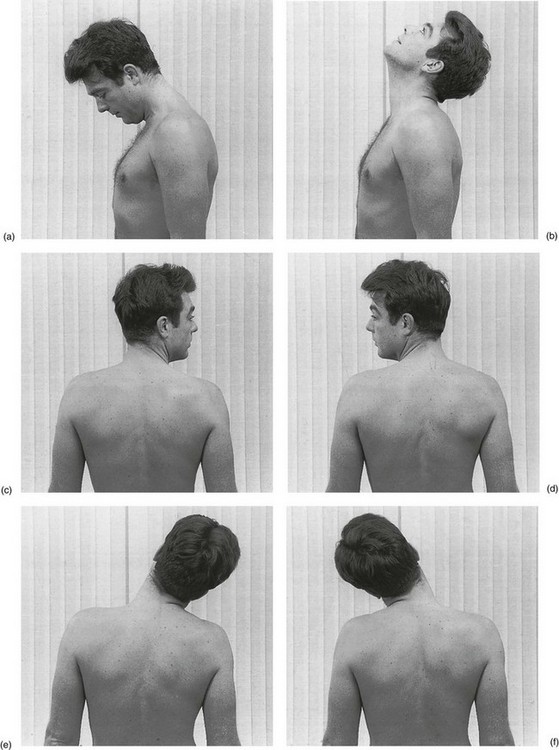
Active movements
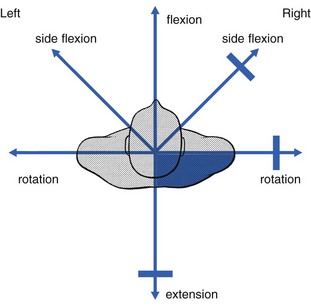
The patient is asked to flex and extend the head and to rotate and tilt it in both directions (Fig. 6.2). The amplitude of each movement is noted and the patient indicates whether it is painful and, if so, where. Neck flexion must be considered not only as an articular test for the cervical spine but also as a dural test for the thoracic spine in that it stretches both the cervical and the thoracic dura. Hence, if pain is elicited in the upper thoracic region, it may be the consequence of a dural impingement at either a cervical or a thoracic level. The relation of the movements shows either a symmetrical (full articular) pattern (Fig. 6.3) or an asymmetrical (partial articular) pattern (Fig. 6.4). The full articular pattern of the cervical spine is: some or great limitation of extension, equal degree of limitation of both rotations and both lateral flexions and no limitation of flexion. All other combinations of pain (and limitation) are classified as partial articular patterns.
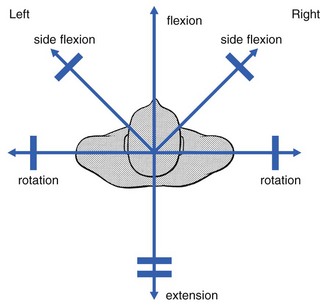
Fig 6.3 The full articular pattern.
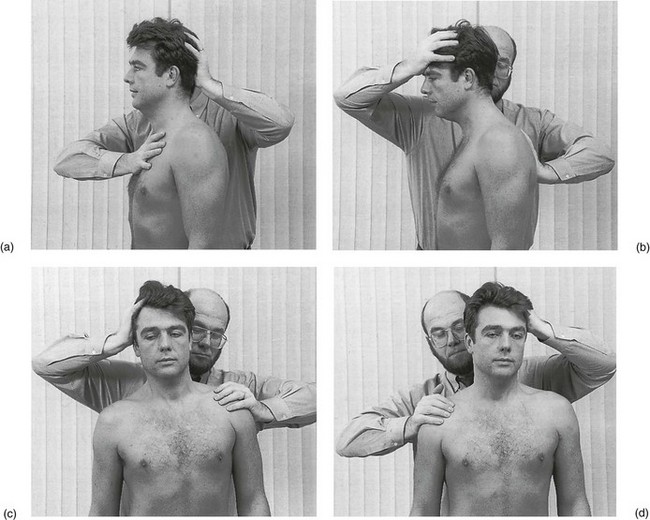
Passive movements
Next, the same movements are performed passively. However, it is not always necessary to carry these out. Flexion and both lateral flexions are done in doubtful cases only, but passive extension and both passive rotations are always executed with great care. Pain, limitation and the end-feel are assessed. The normal end-feel is capsular. Abnormal end-feels are muscle spasm, bone-to-bone, crisp, empty, soggy and elastic rebound. They point towards particular pathological entities (see Ch. 4).
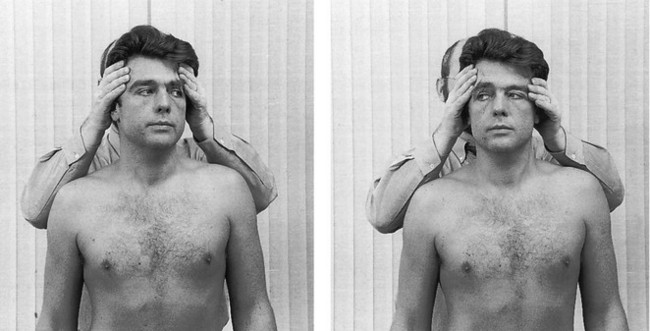
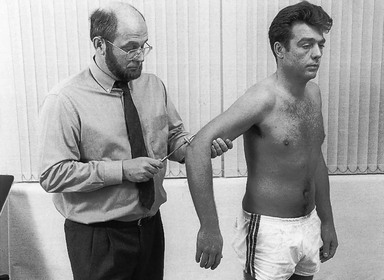
Resisted movements
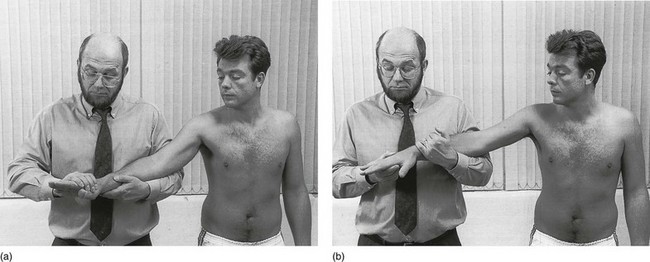
Primary test: rotation
The patient holds the head in the neutral position. The examiner places the forearms against both scapulae with the fingers just above the patient’s ears and the fingertips pointing forwards so that they lie on the temples (Fig. 6.5). The patient is asked to rotate the head and the movement is resisted with the fingertips.
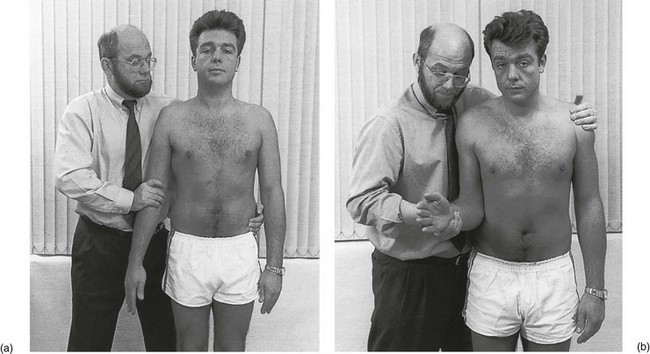
Scapular movements
Active movement
The patient is asked to elevate the shoulders (Fig. 6.7). Pain and/or limitation are checked.
The mobility of the scapula on the thoracic cage, together with the integrity of the acromioclavicular joints, the sternoclavicular joints and the joints between the first ribs and the vertebral column, is assessed. Any pain and/or limitation suggest the need for a full shoulder girdle examination (see p. 210).
Arm tests
Arm movements test the integrity of the muscular system.
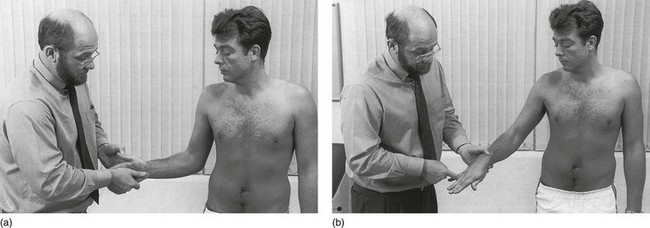
Active elevation
The patient is asked to elevate both arms sideways, as high as possible (Fig. 6.9). This is a swift scan for shoulder and shoulder girdle problems. If there is pain and/or limitation, a complete shoulder examination should follow (see Ch. 12).
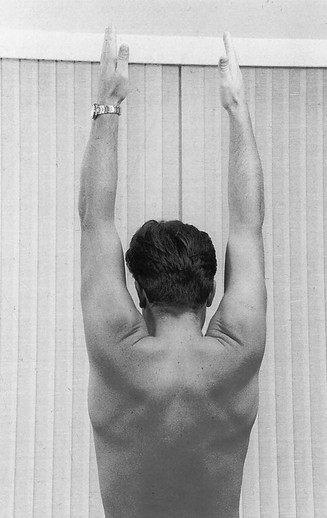
Fig 6.9 Active elevation of the arms.
Resisted movements
The tests are illustrated in Figures 6.10–6.13. Detailed execution of the different tests is discussed in the relevant chapters on the shoulders, elbow and wrist.
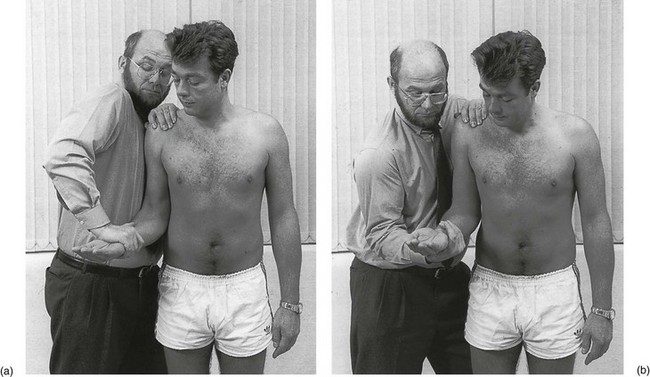
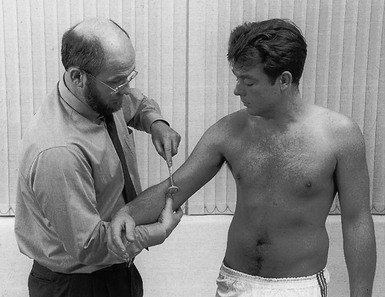
Sensory conduction
The examiner passes his fingers over the patient’s skin in the different dermatomes (Fig. 6.14). The patient is asked if the sensation is the same over all areas.
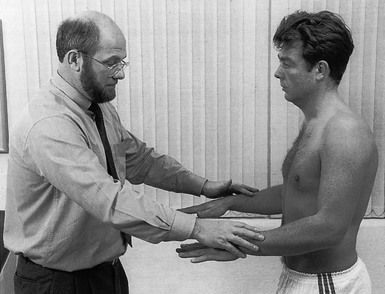
Fig 6.14 Testing sensory conduction.
One arm is compared with the other, and each dermatome is compared with the others in the same limb.
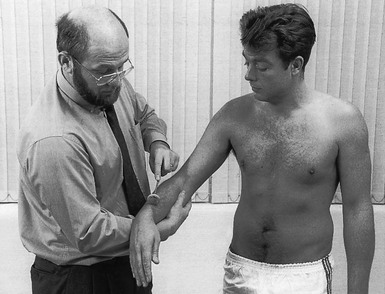
Testing reflexes
Biceps reflex
The patient’s elbow is held at a right angle and is well relaxed. The tendon is stretched by the pressure of the examiner’s thumb on which the hammer is tapped. The C5 and C6 nerve roots are tested. The reaction is elbow flexion (Fig. 6.15).
Brachioradialis reflex
The patient’s elbow is held at a right angle and is well relaxed. The hammer taps on the distal end of the radius. This tests the C5 nerve root. The reaction is elbow flexion (Fig. 6.16).
Triceps reflex
The patient’s elbow is 90° flexed and well relaxed. The hammer strikes the triceps tendon, just proximal to the olecranon. The C7 nerve root is tested. The reaction is elbow extension (Fig. 6.17).
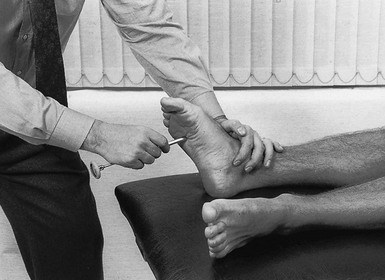
Plantar reflex
To test the plantar reflex, the examiner uses the sharp end of the reflex hammer to stroke the sole of the patient’s foot, starting at the lateral aspect of the heel and moving along the lateral border of the foot to the base of the fifth metatarsal bone and then onwards to the base of the big toe at the medial aspect of the foot. The normal reaction, as described by Strümpell, is flexion of the toes and withdrawal of the foot (Fig. 6.18). The pathological reflex – Babinski’s sign – is a slow extension of the big toe, combined with spreading of the other toes and flexion of knee and hip. The presence of Babinski’s sign indicates a (severe) central disorder.
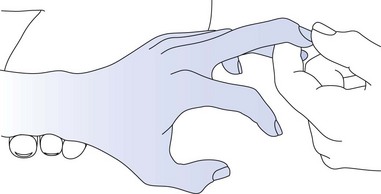
Hoffmann’s sign
The hand is supported and pronated so that wrist and fingers fall into slight flexion. The middle finger is firmly grasped and partially extended. The nail is then flicked by the examiner’s thumbnail. This flicking should be done with considerable force. The sign is considered to be positive when quick flexion of both the thumb and the index finger results.3 A positive sign is indicative of possible pyramidal tract pathology (Fig. 6.19).4
A summary of the neurological deficit at each level is given in Table 6.2.
Table 6.2
Neurological deficit at each level
| Level | Deficit |
| C1–C2 | Tingling in the occipitoparietal region. Muscular weakness is rare |
| C3 | Paraesthesia or numbness at the lower pinna, the posterior part of the cheek, the temporal area and the lateral aspect of the neck. Weakness is clinically not detectable. Cutaneous analgesia is uncommon (the lateral aspect of the neck) |
| C4 | A horizontal band of cutaneous analgesia along the spine of the scapula, the mid-deltoid area and the clavicle. Slight weakness of the trapezii. Paraesthesia does not occur |
| C5 | Weakness of the supraspinatus, infraspinatus, deltoid and brachial biceps muscles. The biceps and brachioradialis jerks are sluggish or absent. Paraesthesia and sensory deficit do not occur |
| C6 | Paraesthesia in thumb and index fingers. Analgesia at the tips of thumb and index fingers. Weakness of the biceps, brachialis, supinator brevis and the extensores carpi radiales muscles. The biceps jerk is sluggish or absent |
| C7 | Paraesthesia in index, middle and ring fingers. Cutaneous analgesia at the dorsal aspect of the index and middle fingers. The weak muscles are the triceps and the flexor carpi radialis. The triceps jerk may be affected |
| C8 | Paraesthesia in the middle, ring and little fingers. Cutaneous analgesia at the little finger. The weak muscles are both extensors of the thumb, the extensor and flexor carpi ulnaris, the adductor pollicis, the common extensor of the fingers and the abductor indicis |
| T1 | Paraesthesia and cutaneous analgesia at the ulnar aspect of the hand, and weakness of the intrinsic muscles of the hand |
| T2 | Paraesthesia and motor and sensory deficit are very uncommon |
A summary of the functional examination is given in Box 6.2.
Technical investigations
During recent decades there has been a tendency to reduce the time spent on history taking and clinical examination and to proceed immediately with technical investigations in order to detect the anatomical changes that are held to be responsible for a patient’s condition. This trend not only has serious financial consequences but also leads to diagnostic errors. It is important to realize that imaging, whether it is X-ray, computed tomography (CT) or magnetic resonance imaging (MRI), does not reveal the source of the pain but only shows anatomical changes that may or may not be consistent with the patient’s description of the pain. Most of these anatomical alterations reflect painless degenerative changes that are normal at certain ages and which may also be present in asymptomatic individuals. The examiner should constantly keep in mind the fact that the presence of anatomical and morphological changes does not automatically imply causality. For example: CT and MRI are widely used to demonstrate the existence of discal disorders, which also exist in a large number of asymptomatic people. Boden5 cites a figure between 14 and 28% and Teresi6 a figure of 23%. According to Matsumoto et al, degeneration is present in 86% of the discs of asymptomatic individuals of over 60 years of age. Posterior disc protrusion is observed in 7.6% of asymptomatic subjects.7
Radiography may show congenital anomalies but quite often these are not clinically significant. Another reason for obtaining plain films is to exclude fractures and luxations.8 Plain radiography has a specificity of 100% in low-risk patients.9,10 However, in high-risk patients, helical CT scan seems to be the preferred initial screening test for detection of cervical spine fractures.11,12 The most important consideration with cervical X-rays is perhaps the risk of missing tumours and infections. It is important to remember, however, that bony disorders are not always visible on plain X-rays in their initial stages, and a negative examination may give a false feeling of security.
Computed tomography is a good diagnostic tool for bony disorders, such as fractures and luxations, where it is often more effective than plain radiography and MRI.13 It is useful to demonstrate osseous neural foraminal stenosis, bone destruction or bone proliferation and ossification of the posterior longitudinal ligament. It is also effective for detecting cranial migration of the odontoid process in rheumatoid arthritis patients.14
Magnetic resonance imaging – because of its superior depiction of soft tissue anatomy – is a preferred tool for the diagnosis of soft tissue disorders such as pre- or paravertebral haemorrhage or oedema, ligamentous lesions and disc herniations.15 It is also excellent for demonstrating cord compression and nerve root injuries.16 It appears to be the most reliable imaging study for diagnosing spinal infections17 and tumours.18 Dynamic functional MRI may provide additional information in patients with rheumatoid arthritis.19
Conclusions
• Technical investigation should not replace clinical examination.
• It may be used to clarify the clinical picture or to exclude a serious disorder.
• The results must be evaluated with great care and only in the light of the clinical picture.
• In doubtful cases, clinical evaluation will be more important than technical investigations.
• Treatment decisions should never be taken on the outcome of imaging studies alone.
References
1. Samartzis, DD, Herman, J, Lubicky, JP, Classification of congenitally fused cervical patterns in Klippel–Feil patients: epidemiology and role in the development of cervical spine-related symptoms. Spine. 2006;31(21):E798–E804. ![]()
2. McCarthy, K, Bondy, CA, Turner syndrome in childhood and adolescence. Expert Rev Endocrinol Metab. 2008;3(6):771–775. ![]()
3. Bendheim, OL. On the history of Hoffmann’s sign. Bull Inst Hist Med. 1937; 5:684–685.
4. Glaser, JA, Curie, JK, Bauley, KL, et al, Cervical spinal cord compression and the Hoffman sign. Iowa Orthop J 2001; 21:49–52. ![]()
5. Boden, SD, McCowin, PR, Davis, DO, et al, Abnormal magnetic resonance scans of the cervical spine in asymptomatic subjects. J Bone Joint Surg (Am) 1990; 72:1178–1184. ![]()
6. Teresi, LM, Lufkin, RB, Reicher, MA, Asymptomatic degenerative disc disease and spondylosis of the cervical spine: MR imaging. Radiology 1987; 164:83–88. ![]()
7. Matsumoto, M, Fujimura, Y, Suzuki, N, et al, MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80(1):19–24. ![]()
8. American College of Surgeons Committee on Trauma. Advanced Trauma Life Support Course for Physicians. Chicago: American College of Surgeons; 1984.
9. Nguyen, GK, Clark, R, Adequacy of plain radiography in the diagnosis of cervical spine injuries. Emerg Radiol. 2005;11(3):158–161. ![]()
10. Holmes, JF, Akkinepalli, R, Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma. 2005;58(5):902–905. ![]()
11. Blackmore, CC, Ramsey, SD, Mann, FA, Deyo, RA, Cervical spine screening with CT in trauma patients: a cost-effectiveness analysis. Radiology. 1999;212(1):117–125. ![]()
12. Grogan, EL, Morris, JA, Jr., Dittus, RS, et al, Cervical spine evaluation in urban trauma centers: lowering institutional costs and complications through helical CT scan. J Am Coll Surg. 2005;200(2):160–165. ![]()
13. Katz, MA, Beredjiklian, PK, Vresilovic, EJ, et al, Computed tomographic scanning of cervical spine fractures: does it influence treatment? J Orthop Trauma. 1999;13(5):338–343. ![]()
14. Ostensen, H, Gudmundsen, TE, Haakonsen, M, et al, Three dimensional CT evaluation of occipito-atlanto-axial dislocation in rheumatoid arthritis. Scand J Rheumatol. 1998;27(5):352–356. ![]()
15. Dai, L, Disc degeneration and cervical instability. Correlation of magnetic resonance imaging with radiography. Spine. 1998;23(16):1734–1738. ![]()
16. Song, KJ, Choi, BW, Kim, GH, Kim, JR, Clinical usefulness of CT-myelogram comparing with the MRI in degenerative cervical spinal disorders: is CTM still useful for primary diagnostic tool? J Spinal Disord Tech. 2009;22(5):353–357. ![]()
17. Rothman, SLG, The diagnosis of infections of the spine by modern imaging techniques. Orthop Clin North Am 1996; 27:15–31. ![]()
18. Chiewvit, P, Danchaivijitr, N, Sirivitmaitrie, K, et al, Does magnetic resonance imaging give value-added than bone scintigraphy in the detection of vertebral metastasis? J Med Assoc Thai. 2009;92(6):818–829. ![]()
19. Allmann, KH, Uhl, M, Uhrmeister, P, et al, Functional MR imaging of the cervical spine in patients with rheumatoid arthritis. Acta Radiol. 1998;39(5):543–546. ![]()