Chapter 62 Classification of Thoracolumbar Spine Fractures
Review of Thoracolumbar Classification Schemes
The biomechanical force vectors acting on the spine can be either rotational or linear. Among the rotational forces are flexion, extension, lateral bending, and torsional forces. Linear forces include compression, translational, and distraction forces. These forces can act alone or in combination, resulting in different and diverse fracture patterns.1 Although not always possible, categorizing a fracture based on a classification system is crucial to aid the clinician in selecting the appropriate management strategy. An effective classification system should be comprehensive, easy to apply, and directive of appropriate treatment.2
Current classification systems base their algorithms on the stability of different fracture patterns. The earliest attempt to classify thoracolumbar spine fractures was reported by Boehler in 1929.2 He grouped thoracolumbar fractures into five entities: compression, flexion-distraction, extension, shear, and rotational fractures. In 1938, Watson-Jones3 divided these fractures into simple wedge fractures, comminuted fractures, and fracture-dislocations. He introduced the concept of instability and was the first to associate the integrity of the posterior ligamentous complex (PLC) with spinal stability. In 1949, Nicoll4 categorized fractures into stable and unstable fractures. He ascribed four structures as contributing to spinal stability: the vertebral body, the disc, the facets, and the interspinous ligaments. In his view, the integrity of the latter was the major determinant of stability. He classified thoracolumbar spine fractures into anterior wedge, lateral wedge, fracture-dislocations, and neural arch fractures.
In his landmark 1963 paper, Holdsworth introduced the two-column theory of spinal stability.5 He recognized five mechanisms of injury: flexion, flexion-rotation, extension, compression, and shear forces. His classification scheme included anterior compressions; fracture-dislocations; rotational fracture-dislocations; and extension, shear, and burst fractures. He then categorized fractures as stable or unstable. According to his model, the spine was divided into anterior and posterior columns. The anterior column consisted of the vertebral body and the intervertebral disc, and the posterior column consisted of the neural arch, facet joints, and PLC (interspinal and supraspinal ligaments and ligamentum flavum). Fractures that included posterior column injury were unstable. His model thus defined burst-type fractures, which he was the first to describe, as stable.
In a sometimes controversial formulation, White and Panjabi in 1978 defined clinical instability as the inability of the spine under physiologic loads to maintain relationships between vertebrae such that there is neither acute nor subsequent neurologic injury, deformity, or pain.6 In addition to neurologic deficit, motion, and disruption of the anterior and posterior “elements,” their algorithm recognized the significance of pain and the anticipated loading of the spine. The latter, although significant, had not been identified in previous paradigms of fracture severity.
The three-column theory of the spine was introduced by Francis Denis in 1983.7 He added a third or middle column to Holdsworth’s two-column model. According to Denis, the anterior column of the spine comprised the anterior longitudinal ligament and the anterior half of the vertebral body, anulus, and disc. The middle column included the posterior half of the vertebral body, anulus, and disc, in addition to the posterior longitudinal ligament. The posterior column incorporated the neural arch, facets, and PLC, which consisted of the supraspinal and interspinal ligaments, ligamentum flavum, and facet capsules (Fig. 62-1). The middle column was important because for dislocation to occur, it was necessary to disrupt the middle column along with the anterior or posterior column, or both. Denis defined stability based on the integrity of two of the three columns. His classification included four groups: compression fractures resulting from failure of the anterior column under compression, burst fractures resulting from failure of the anterior and middle columns secondary to fractures of the vertebral body under axial loads, flexion-distraction injuries secondary to failure of the posterior and middle columns, and fracture-dislocations resulting from failure of all three columns. Under this scheme, flexion-distraction injuries or seat belt-type injuries were considered unstable in the first degree. Burst fractures with deficit were considered unstable in the second degree, and fracture-dislocations were unstable in the third degree. This classification system was later supported by in vitro biomechanical studies.8
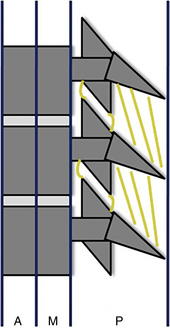
FIGURE 62-1 Denis’s three-column model of the spine: anterior column (A), middle column (M), posterior column (P).
As opposed to Denis, who subdivided basic injury patterns based on review of mostly radiographs of 412 fractures (53 were CT images), McAfee et al. in 1983 based their classification on an examination of CT scans with sagittal reconstruction from 100 patients.9 They recognized six fracture patterns: wedge compression, stable burst, unstable burst, Chance fracture, flexion-distraction, and translational. They linked the stability of burst fractures with the integrity of the PLC, emphasizing the PLC as the major factor in fracture stability. Shortly afterward, in 1984, Ferguson and Allen10 introduced the “mechanistic classification.” They classified fractures into seven categories: compressive flexion, distractive flexion, lateral flexion, torsional flexion, translation, vertical compression, and distractive flexion injuries.
In 1989, Magerl et al.11 introduced the AO (Arbeitsgemeinschaft für Osteosynthesefragen) classification system, based on a 10-year review of 1445 thoracolumbar fractures. They recognized three main fracture types: type A (compression), type B (distraction), and type C (fracture-dislocation). Subdivisions were created according to the severity of the fracture, resulting in 53 fracture patterns, with A1 being the least severe and C3 the most severe. This schema was generated based on review of radiographs, and as a result of their diligence, the schema was extensive and not always user friendly.
The load-sharing classification, introduced by McCormack et al. in 1994,12 was derived from analysis of failures of thoracolumbar spine fractures treated with transpedicular short-segment arthrodesis. Fractures were graded according to the degree of comminution of the body, apposition of the fracture fragments, and deformity. A point system from 1 to 3 was applied to each fracture, with a higher number indicating greater severity. Fractures with a score greater than 7 had a high risk of short-segment fixation failure. This algorithm was intended to aid in the surgical decision of whether to use short-segment arthrodesis or anterior column graft support. The classification was validated biomechanically in vitro.13
In 2005, the Spine Trauma Study Group introduced the Thoracolumbar Injury Severity Score (TLISS) as a new classification system.13–15 The system was based on three injury characteristics: mechanism of injury, neurologic status, and integrity of the PLC. Pertaining to the mechanism of injury, compression injuries are assigned one point; compression fractures with coronal plane deformity greater than 15 degrees and burst fractures are assigned two points. Translational or rotational injuries receive three points, and distraction injuries, being the most unstable, receive four points. The severity of neurologic injury is scored based on a five-category system. Patients with a negative neurologic examination receive zero points. In the presence of nerve root injury or complete spinal cord injury, the fracture is assigned two points. Patients with an incomplete spinal cord injury or cauda equina syndrome are assigned three points. The integrity of the PLC can be assessed clinically by the presence of a palpable interspinous gap, by separation of the spinous processes on plain radiographs, or by MRI. Patients with an intact PLC receive zero points. Those in whom the integrity of the PLC is indeterminate receive two points, and those with confirmed injury receive three points.
Based on a study that showed fair to moderate inter-rater agreement,16 the TLISS system, which emphasizes the mechanism of injury, was modified into the Thoracolumbar Injury Classification and Severity Score (TLICS), which emphasizes the morphology of fractures. In cases of multiple mechanisms involving one or more levels, the TLICS, as opposed to the TLISS, would consider only the most severe injury mechanism. Moreover, the one-point addition for coronal plane deformity was eliminated. Subsequent studies showed that both the TLISS and TLICS were comparable.17,18 Moreover, Lenarz et al.19 showed that the interobserver reliability of the TLISS system was comparable to that of the Denis and AO systems. The TLICS algorithm encompasses radiographic or mechanistic criteria, clinical criteria, and the integrity of the PLC assessed on MRI. No weight is given to the presence of pain, however.
Iowa Classification System and Algorithm
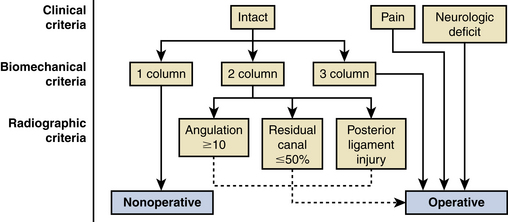
Recognizing the aforementioned schemes, and based on data collected prospectively on 300 thoracolumbar fractures, a simple classification system and algorithm for thoracolumbar spine fractures were developed (Fig. 62-2). This algorithm is based on three categories of criteria: clinical, biomechanical, and radiographic. The clinical criteria address the presence or absence of pain or neurologic deficit. Biomechanical criteria describe the involvement of one, two, or three columns, referring to Denis’s three-column theory. Radiographic criteria address the degree of kyphosis and canal compromise, and the integrity of the PLC.
This algorithm recognizes four major types of thoracolumbar spine fractures:
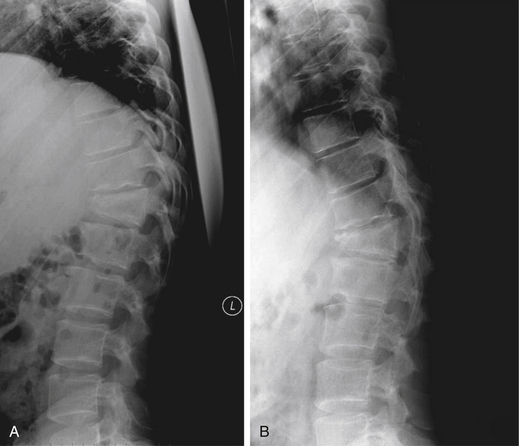
1. Wedge compression fractures: These are the most common type of fractures and occur secondary to axial load application in flexion.1 These fractures involve injury to the anterior Denis column only, sparing the middle and posterior columns (Fig. 62-3). Patients are typically neurologically intact and associated PLC disruption is rare. Conservative management with bracing and/or analgesia is the usual treatment. Patients with osteoporosis are at risk for these fractures, which can lead to severe kyphosis if multiple levels are involved.
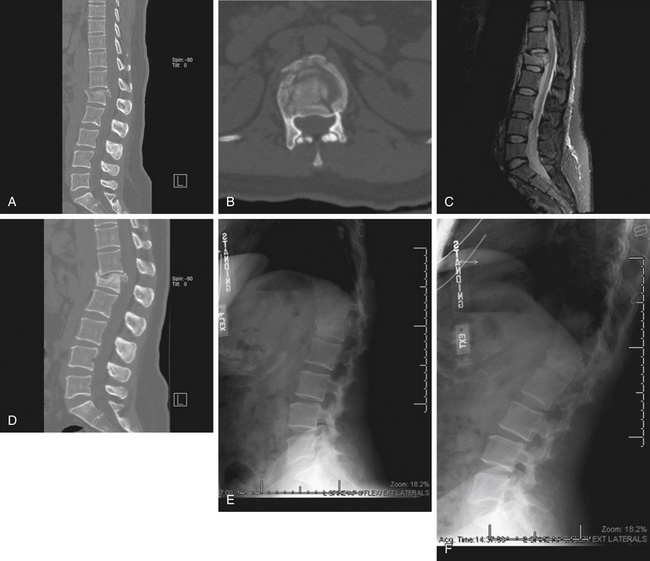
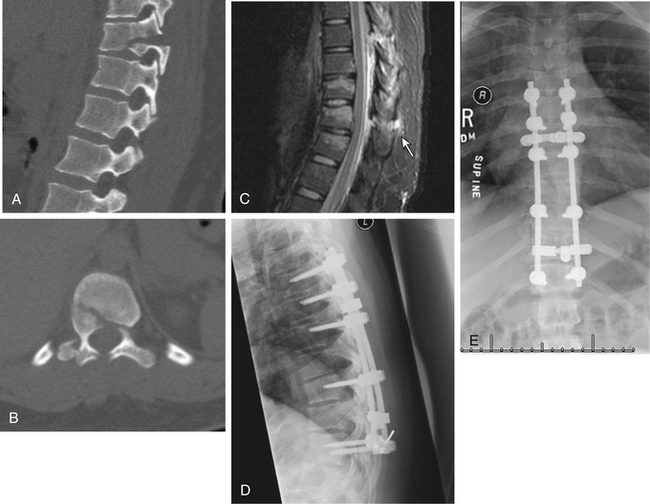
2. Burst fractures: These fractures occur as a result of axial load application. They involve injury to both the anterior and middle columns of Denis. Retropulsion of bony fragments into the canal occurs to varying degrees. The occurrence of associated neurologic injury is similarly variable, but when present demands decompression and stabilization. Correlation between the occurrence of neurologic deficit and the extent of canal compromise is controversial.20–22 Management of these injuries can be challenging, especially in patients who are neurologically intact.23,24 Disruption of the PLC as ascertained by MRI renders these fractures unstable. An unpublished, prospective review of 70 burst fractures treated at the University of Iowa since 1993 was conducted. Owing to absent or minimal neurologic deficit, this cohort was treated nonoperatively. Ultimately, 20 patients failed nonoperative treatment, mostly because of pain, and underwent surgery. The data suggest that in burst fractures, an angulation of more than 10 degrees and a residual canal of less than 50% were associated with failure of nonoperative treatment. On the other hand, patients with burst fractures who are neurologically intact without disruption of the PLC, in whom angulation is less than 10 degrees and the residual canal exceeds 50% of normal, will most likely succeed with nonoperative treatment (Figs. 62-4 and 62-5).
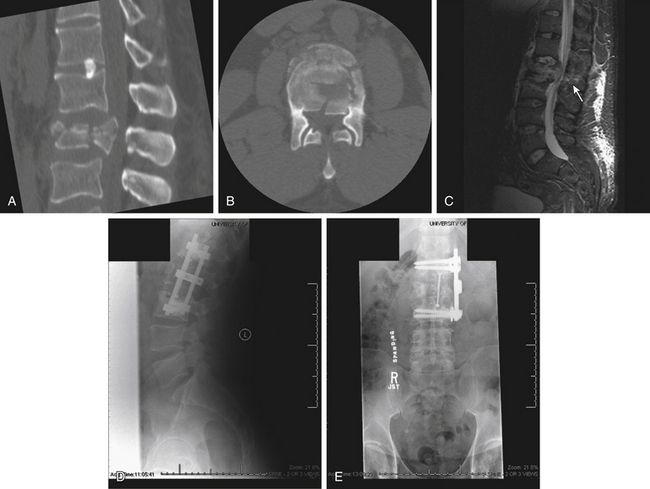
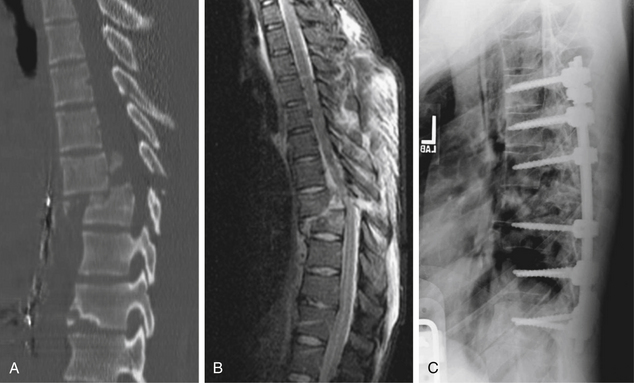
3. Flexion-distraction injuries: These fractures occur secondary to failure of Denis’s middle and posterior columns, with preservation of the anterior longitudinal ligament. The classic example is the Chance fracture, which involves failure of the middle and posterior bony columns, or can be limited to ligamentous injury traversing the PLC and disc-anulus complex, or a combination of both (Fig. 62-6). Surgical management is the rule because these fractures are inherently unstable.
4. Fracture-dislocations: These occur secondary to rotational shear forces, translational forces, or a combination of both. All three Denis columns are involved, rendering these fractures highly unstable (Fig. 62-7). Associated neurologic compromise is common. Surgical management is the rule.
Conclusion
In conclusion, there are many classifications for spinal fractures. The schemas differ in their complexity, completeness, and treatment guidance, but generally overlap to varying degrees. It is up to the spine surgeon to use the system with which he or she feels most comfortable to classify and manage patients with these fractures. In addition to criteria derived from plain radiographs, CT, and MRI, it is important to consider the patient’s clinical and neurologic condition before proceeding with management.
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8:817-831.
Magerl F., Aebi M., Gertzbein S.D., et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201.
McCormack T., Karaikovic E., Gaines R.W. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741-1744.
Panjabi M.M., Oxland T.R., Kifune M., et al. Validity of the three-column theory of thoracolumbar fractures: a biomechanic investigation. Spine (Phila Pa 1976). 1995;20:1122-1127.
Vaccaro A.R., Zeiller S.C., Hulbert R.J., et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209-215.
White A.A.III, Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: JB Lippincott; 1978. p 240
1. Vollmer D.G., Gegg C. Classification and acute management of thoracolumbar fractures. Neurosurg Clin North Am. 1997;8:499-507.
2. Sethi M.K., Schoenfeld A.J., Bono C.M., et al. The evolution of thoracolumbar injury classification systems. Spine J. 2009;9:780-788.
3. Watson-Jones R. The results of postural reduction of fractures of the spine. J Bone Joint Surg [Am]. 1938;20:567-586.
4. Nicoll E.A. Fractures of the dorso-lumbar spine. J Bone Joint Surg [Br]. 1949;31:376-394.
5. Holdsworth F.W. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg [Br]. 1963;45:6-20.
6. White A.A.III, Panjabi M.M. Clinical biomechanics of the spine. Philadelphia: JB Lippincott; 1978. p 240
7. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8:817-831.
8. Panjabi M.M., Oxland T.R., Kifune M., et al. Validity of the three-column theory of thoracolumbar fractures: a biomechanic investigation. Spine (Phila Pa 1976). 1995;20:1122-1127.
9. McAfee P.C., Yuan H.A., Fredrickson B.E., et al. The value of computed tomography in thoracolumbar fractures: an analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg [Am]. 1983;65:461-473.
10. Ferguson R.L., Allen B.L.Jr. A mechanistic classification of thoracolumbar spine fractures. Clin Orthop Relat Res. 1984;189:77-88.
11. Magerl F., Aebi M., Gertzbein S.D., et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201.
12. McCormack T., Karaikovic E., Gaines R.W. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741-1744.
13. Wang X.Y., Dai L.Y., Xu H.Z., et al. The load-sharing classification of thoracolumbar fractures: an in vitro biomechanical validation. Spine (Phila Pa 1976). 2007;32:1214-1219.
14. Vaccaro A.R., Lehman R.A.Jr., Hurlbert R.J., et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30:2325-2333.
15. Vaccaro A.R., Zeiller S.C., Hulbert R.J., et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209-215.
16. Harrop J.S., Vaccaro A.R., Hurlbert R.J., et al. Intrarater and interrater reliability and validity in the assessment of the mechanism of injury and integrity of the posterior ligamentous complex: a novel injury severity scoring system for thoracolumbar injuries. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2005. J Neurosurg Spine. 2006;4:118-122.
17. Bono C.M., Vaccaro A.R., Hurlbert R.J., et al. Validating a newly proposed classification system for thoracolumbar spine trauma: looking to the future of the thoracolumbar injury classification and severity score. J Orthop Trauma. 2006;20:567-572.
18. Whang P.G., Vaccaro A.R., Poelstra K.A., et al. The influence of fracture mechanism and morphology on the reliability and validity of two novel thoracolumbar injury classification systems. Spine (Phila Pa 1976). 2007;32:791-795.
19. Lenarz C.J., Place H.M., Lenke L.G., et al. Comparative reliability of 3 thoracolumbar fracture classification systems. J Spinal Disord Tech. 2009;22:422-427.
20. Meves R., Avanzi O. Correlation between neurological deficit and spinal canal compromise in 198 patients with thoracolumbar and lumbar fractures. Spine (Phila Pa 1976). 2005;30:787-791.
21. Mohanty S.P., Bhat N.S., Abraham R., et al. Neurological deficit and canal compromise in thoracolumbar and lumbar burst fractures. J Orthop Surg (Hong Kong). 2008;16:20-23.
22. Mohanty S.P., Venkatram N. Does neurological recovery in thoracolumbar and lumbar burst fractures depend on the extent of canal compromise? Spinal Cord. 2002;40:295-299.
23. Siebenga J., Leferink V.J., Segers M.J., et al. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976). 2006;31:2881-2890.
24. Wood K., Buttermann G., Mehbod A., et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective, randomized study. J Bone Joint Surg [Am]. 2003;85:773-781.