CHAPTER 39 Chronic Volar-Flexed Intercalated Segment Instability
The definition of instability of the wrist has been described by the International Wrist Investigators’ Workshop as “the inability of the carpus to maintain its normal anatomical relationships under physiological loading.” Dobyns and colleagues,1 and more recently the International Wrist Investigators’ Workshop, have suggested a number of terms that describe the patterns of instability:
It is now accepted that the stability of the carpus is wholly dependent on the integrity of the interosseous and capsular ligaments of the wrist joint and not on any inherent stability conferred by bone shape or position.2
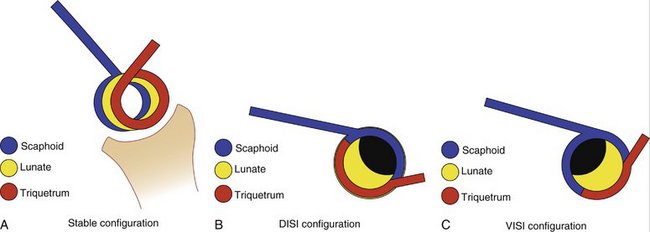
One might look at the effects of failure of these ligaments by using an analogy of the coiled spring. This concept, proposed by Garcia-Elias, identifies that the scaphoid, the lunate, and the triquetrum are intimately connected and, as Kapandji has described,3 there is a variable geometry of the proximal row of the carpus as the loaded wrist is moved. Thus, the scaphoid flexes, extends, pronates, supinates, and translates. The lunate flexes, extends, and translates but does not pronate or supinate. Finally, the triquetrum flexes and extends much less than the lunate but does not pronate or supinate and although it does translate, it does not articulate with the distal radius and barely articulates with the triangular fibrocartilage complex (TFCC). The scaphoid has a long lever arm by comparison to the lunate and triquetrum and therefore has a profound effect on the biomechanics of the wrist. Using the coiled spring analogy, axial loading of the intact wrist requires the rotational moment of the scaphoid to be balanced by the opposite rotational moment of the triquetrum, with the lunate acting as the torque converter in its position as the intercalated segment of the proximal row. Failure of the scapholunate ligament gives rise to the potential for the scaphoid to flex under the axial loading but, of course, the triquetral/lunate complex rotational moment is unopposed and the lunate and triquetrum extend, giving rise to the radiographic appearance of dorsiflexed intercalated segment instability (DISI). If, however, the lunate is separated from the triquetrum, the rotational moment of the scaphoid takes the lunate into flexion, thus creating the radiographic appearances of volar-flexed intercalated segment instability (VISI) (Fig. 39-1).4–7
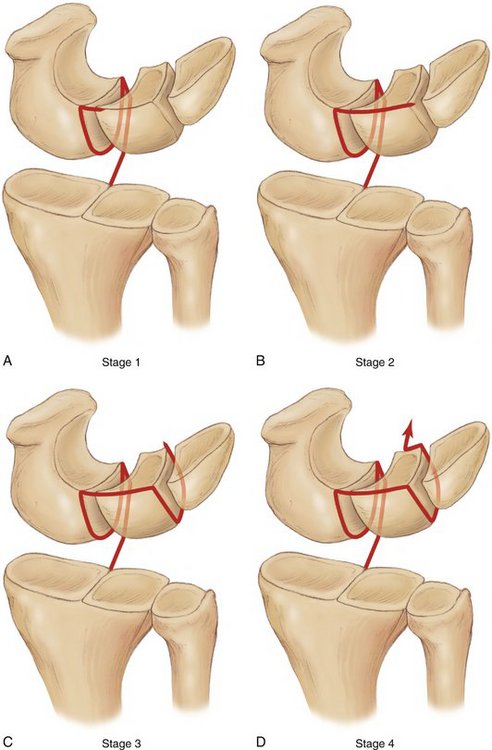
The work of Mayfield and Johnson8 has shown us that there are patterns of ligamentous injury, through a radial-sided applied force, in which, with the wrist loaded in extension and ulnar deviation, axial loading resulted in sequential ligament disruption. In effect, these injuries occurred as a result of applying what might be described as a proximal row supination force to the cadaver specimens. This is translated into the in vivo injury when, as a result of falling on the outstretched hand, the thenar eminence (Fig. 39-2) contacts the ground first and thereafter the protective pronation reflex of the forearm forces the hand, and therefore the carpus, into supination, resulting in either a pronator quadratus fracture in the child, a Colles’ type fracture in the elderly, a scaphoid fracture in the young male, and a scapholunate, perilunate lesser arc, type of soft tissue injury in most adults. The sequence of ligament failure in this pattern of injury is well recognized and described elsewhere.
The so-called reverse Mayfield sequence, or the proximal row pronation injury, occurs as a result of the forces acting on the hand as the hypothenar eminence strikes the ground first (Fig. 39-3). The patterns of injury are complex in that there are many more ligament attachments to the triquetrum than to the scaphoid. The act of falling on the outstretched hand when the heel of the hand strikes the ground concentrates the forces that now act on the ulnar side of the carpus and therefore through the pisiform to the triquetrum. The position of the pisiform on the volar aspect of the triquetrum results in this pair of bones decelerating rapidly, but the momentum of the individual suffering the injury drives the ulna toward the ground, which results in the forces being transmitted to the structures on the ulnar side of the wrist. There is a tendency to thus force the hand into a pronation attitude with reference to the distal radius and ulna. The ulnar head continues to approach the ground, which leads to a dorsal shearing force that may detach the posterior aspect of the TFCC from the dorsal ulnar carpal ligaments, giving rise to a separation of these two structures. This does not involve a true tear of the TFCC.
Any disruption of connections between the scaphoid and the lunate or the lunate and triquetrum can prevent the wrist from supporting physiological loading without collapsing.5 The proximal row variable geometry system becomes dyskinetic, that is, it is not in the appropriate configuration in most positions of the loaded wrist. It is accepted from anatomical studies that the most important part of the scapholunate interosseous ligament lies dorsally and the most important part of the triquetrolunate interosseous ligament lies anteriorly.7 This allows each of the bones to have its own axis or rotation different from the others and also for each bone to move within its limits set down by these two ligaments.
Ulnar midcarpal instability is traumatic, degenerative, or idiopathic.9–12 The traumatic version is acute or chronic; the degenerative version is chronic and usually defined as part of the ulnar abutment syndrome; and the idiopathic version is related to hyperlaxity and pathological hyperlaxity, as exhibited in Ehlers-Danlos syndrome.
The clinical features of ulnar midcarpal instability are ulnar-sided pain and a sagging carpus. The posterior sag is a very characteristic one and is related to the detachment of the posterior part of the posterior TFCC from the ulnar carpal ligaments, a greater feel of the dorsal tubercle of the triquetrum as this bone flexes, the clunking wrist, tenderness over the lunotriquetral interval, a positive Regan shuck test, and, often, a positive Lichtman pivot shift test.13
The arthroscopic features can be defined as a significant step-off between the lunate and the triquetrum when viewed on midcarpal arthroscopy (Fig. 39-4).
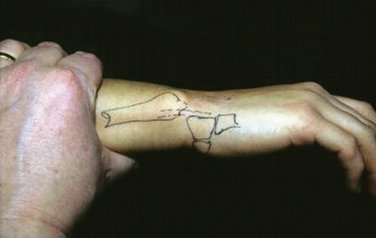
A possible sequence of events is proposed arbitrarily divided into discrete steps based on the known patterns of injury seen (Fig. 39-5):
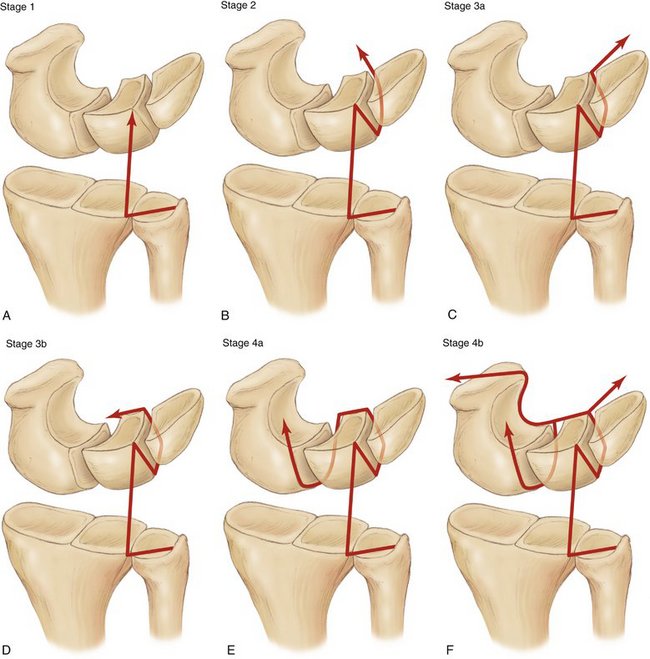
FIGURE 39-5 Proposed mechanism of ulnar midcarpal instability. A, Stage 1: Detachment of ulnar carpal ligaments from the posterior aspect of the TFCC. B, Stage 2: Lunotriquetral ligament disruption. C, Stage 3a: Peritriquetral instability. D, Stage 3b: Disruption of the volar ulnar carpal ligaments. E, Stage 4a: Progressive damage to the scapholunate ligaments (the reverse Mayfield). F, Stage 4b: The complete disruption of the proximal and midcarpal joint system.
Treatment Options for Specific Patterns of Instability
Ulnar Midcarpal Instability (Carpal Instability Dissociative)
The treatment options for the management of chronic lunotriquetral instability are limited.14 An alternative to ligament reconstruction or augmentation is intercarpal fusion, which can give rise to a significant loss of wrist motion.9 At all levels of the problem the treating physician should respond to the patient’s symptoms and, as in any other nonprogressive musculoskeletal problem, the starting point is reassurance and lifestyle modification supported by orthoses and physical therapy in the acute phase or in the acute exacerbation of a chronic injury. Posterior ligament surgery in the form of an extensor carpi ulnaris reconstruction; anterior ligament surgery, which has been described both by Lichtman and by Garcia-Elias; and intercarpal fusions can be performed in cases unresponsive to conservative management. Limited wrist arthrodeses can significantly distort carpal motion, and the results can be disappointing.
Triquetrohamate fusion is ideal for patients with a peritriquetral instability, but this affects a very small number of patients.15
Extensor Carpi Ulnaris Tenodesis for Lunotriquetral Instability
We have described a technique for a ligament augmentation of the dorsal aspects of the ulnar carpal ligament complex, the ECU tenodesis.16 The operation is shown in Figure 39-6.
We have reviewed 46 of these procedures. In the review group there was no gender bias, the average age was 30, the dominant wrist was treated in 33% of patients, and significant trauma was recalled by the patients in 43 cases.16
Lunotriquetral instability as a result of proximal row pronation injuries can be effectively treated with soft tissue reconstruction. Stage 2, 3a, and 3b pronation injuries are suitable for this procedure. This grading is done at the time of arthroscopy. The procedure is less effective in injuries to the triquetrolunate joint as a result of a supination pattern of injury of the carpus. Tensioning of the repair must be performed with the wrist in neutral, not in ulnar, deviation; the surgery is simple, the operating room time is short, and, more importantly, the procedure is reversible. The cosmetic appearance of the scar is very acceptable.
There is an alternative method of repairing the lunotriquetral interval, using a complex reconstruction described from the Mayo Clinic. Garcia-Elias and others have recommended the volar and dorsal approach, repairing both the anterior part of the lunotriquetral internal and the triquetrohamate ligament. This basically is the pisohamate ligament, which runs deep from the pisotriquetral joint to the hook of the hamate at its base. The triquetrocapitate ligament also is reconstructed. Future developments in arthroscopic-assisted surgery may allow earlier diagnosis and intervention, and the techniques of arthroscopic capsular shrinkage may be sufficient to reduce the symptom level to acceptable levels in the milder cases.17
True Midcarpal Instability Nondissociative
True midcarpal instability does not involve any injury to the intrinsic scapholunate or triquetrolunate interosseous ligaments; and because there is no such injury there is no dissociation between the individual bones of either the proximal or the distal rows of the carpus. The instability arises between the proximal and distal rows, and therefore the term “carpal instability nondissociative” is applied. This is related to problems where the extrinsic capsular ligament system fails to adequately maintain the relationship of the proximal row to the distal row and thus allows the distal row to fall into its default position, which forces the proximal row into flexion. This gives rise to the so-called tilting teacup or VISI pattern (Fig. 39-7). Ligament reconstruction (or more accurately augmentation or substitution) is unreliable in these circumstances, and one of the limited fusions may be required.

FIGURE 39-7 Lateral radiograph of wrist demonstrates the volar tilt of the lunate that occurs in midcarpal instability.
Limited wrist arthrodesis can be in the form of lunotriquetral fusion,18 triquetrohamate fusion, capitolunate fusion, lunotriquetral-capitohamate fusion (LTCH or so-called four-corner fusion), and radiolunate fusion (the Chamay fusion).
1. Linscheid RL, Dobyns JH, Beckenbaugh RD, et al. Instability patterns of the wrist. J Hand Surg [Am].. 1983;8:682-686.
2. Viegas SF, Patterson RM, Ward K. Extrinsic wrist ligaments in the pathomechanics of ulnar translation instability. J Hand Surg [Am].. 1995;20:312-318.
3. Kapandji A. [Biomechanics of the carpus and the wrist]. Ann Chir Main.. 1987;6:147-169.
4. Moritomo H, Murase T, Goto A, et al. In vivo three-dimensional kinematics of the midcarpal joint of the wrist. J Bone Joint Surg Am.. 2006;88:611-621.
5. Tang JB, Xie RG, Yu XW, Chen F. Wrist kinetics after lunotriquetral dissociation: the changes in moment arms of the flexor carpi ulnaris tendon. J Orthop Res.. 2002;20:1327-1332.
6. Trumble TE, Bour CJ, Smith RJ, Glisson RR. Kinematics of the ulnar carpus related to the volar intercalated segment instability pattern. J Hand Surg [Am].. 1990;15:384-392.
7. Wiesner L, Rumelhart C, Pham E, Comtet JJ. Experimentally induced ulnocarpal instability: a study on 13 cadaver wrists. J Hand Surg [Br].. 1996;21:24-29.
8. Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg [Am].. 1980;5:226-241.
9. Ambrose L, Posner MA. Lunate-triquetral and midcarpal joint instability. Hand Clin.. 1992;8:653-668.
10. Shin AY, Battaglia MJ, Bishop AT. Lunotriquetral instability: diagnosis and treatment. J Am Acad Orthop Surg.. 2000;8:170-179.
11. Trail IA, Stanley JK, Hayton MJ. Twenty questions on carpal instability. J Hand Surg [Br].. 2007;32:240-255.
12. Weiss LE, Taras JS, Sweet S, Osterman AL. Lunotriquetral injuries in the athlete. Hand Clin.. 2000;16:433-438.
13. Alexander CE, Lichtman DM. Ulnar carpal instabilities. Orthop Clin North Am.. 1984;15:307-320.
14. Lichtman DM, Bruckner JD, Culp RW, Alexander CE. Palmar midcarpal instability: results of surgical reconstruction. J Hand Surg [Am].. 1993;18:307-315.
15. Rao SB, Culver JE. Triquetrohamate arthrodesis for midcarpal instability. J Hand Surg [Am].. 1995;20:583-589.
16. Shahane SA, Trail IA, Takwale VJ, et al. Tenodesis of the extensor carpi ulnaris for chronic, post-traumatic luno-triquetral instability. J Bone Joint Surg Br.. 2005;87:1512-1515.
17. Moskal MJ, Savoie FH3rd, Field LD. Arthroscopic capsulodesis of the lunotriquetral joint. Clin Sports Med.. 2001;20:141-153.
18. Goldfarb CA, Stern PJ, Kiefhaber TR. Palmar midcarpal instability: the results of treatment with 4-corner arthrodesis. J Hand Surg [Am].. 2004;29:258-263.