Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
• Classified into 5 types based on Todani classification
 Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall
Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall
 Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall
Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall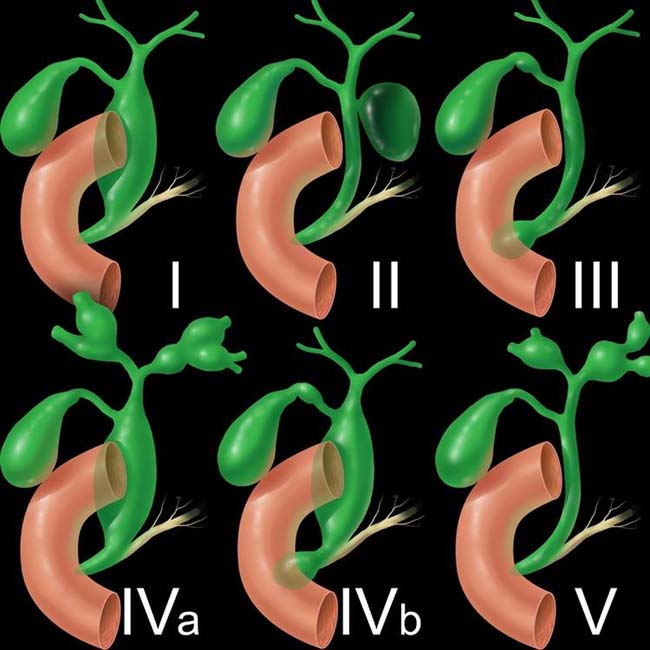
 . Type I lesions are the most common type of choledochal cyst.
. Type I lesions are the most common type of choledochal cyst.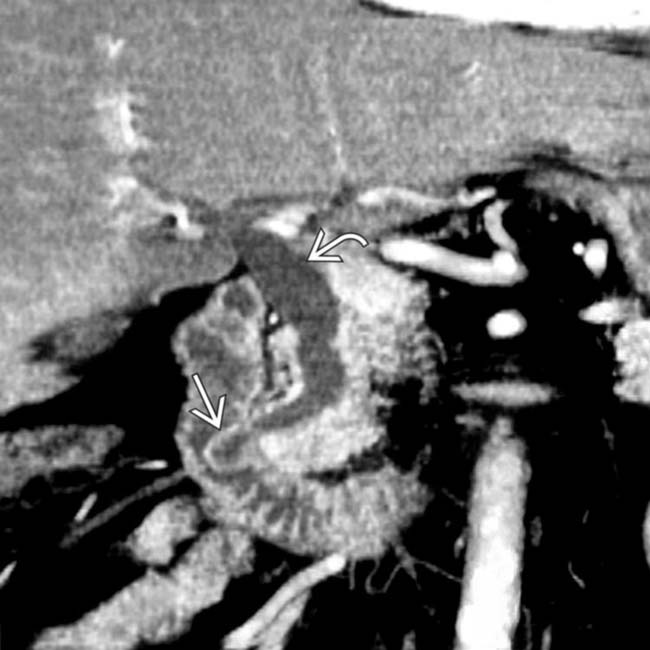
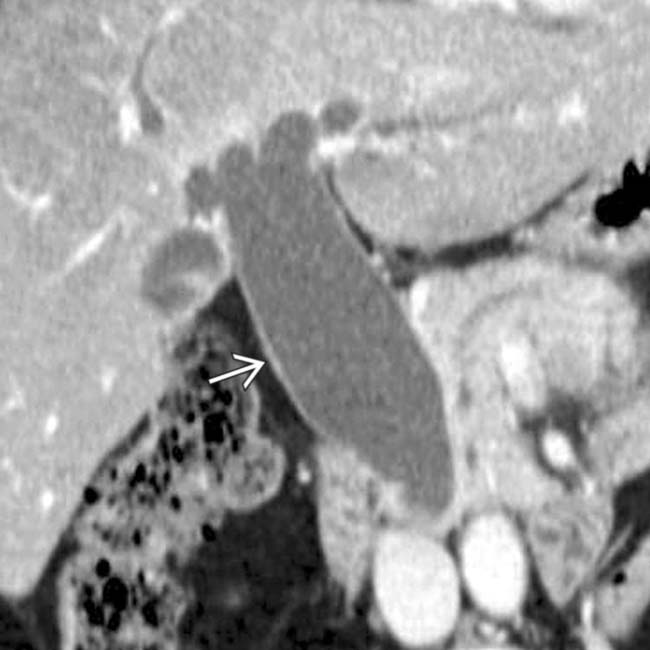
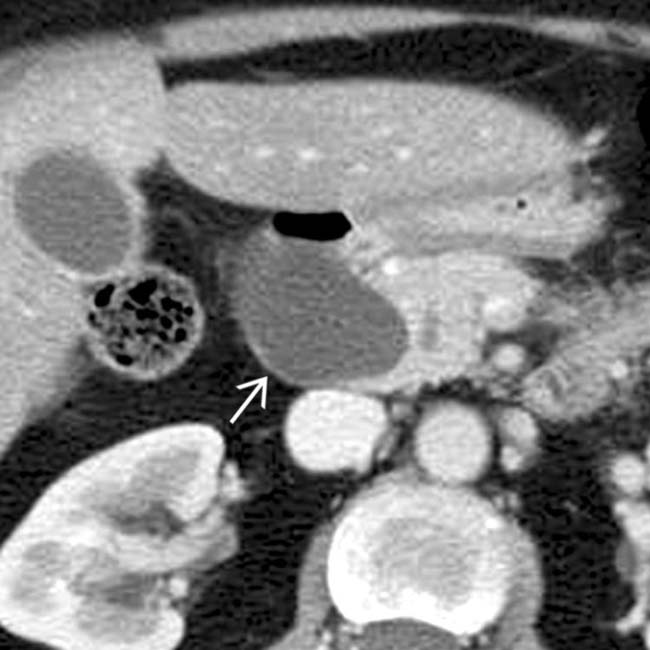
 protruding into the duodenal lumen and mild dilation of the common bile duct
protruding into the duodenal lumen and mild dilation of the common bile duct  . This is either a type III or IVb choledochal cyst, depending on whether the ED is considered to be involved.
. This is either a type III or IVb choledochal cyst, depending on whether the ED is considered to be involved.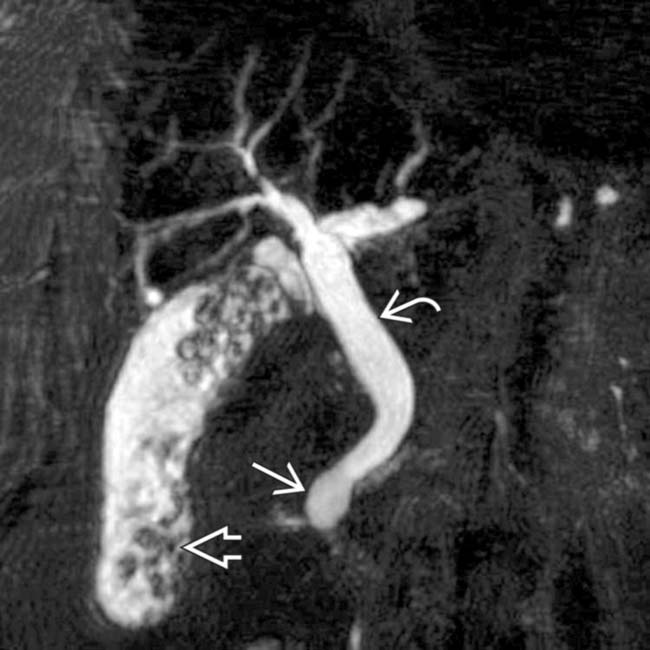
 protruding into the duodenal lumen and the mildly dilated extrahepatic duct
protruding into the duodenal lumen and the mildly dilated extrahepatic duct  , along with numerous stones in the gallbladder
, along with numerous stones in the gallbladder  .
.IMAGING
General Features
• Rare disorder usually diagnosed in infancy and childhood, but is most common congenital lesion of large bile ducts
• Segmental cystic dilatation of bile ducts with dilated segments maintaining communication with biliary tree
 Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
 Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis
Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis
 Most commonly classified into 5 different types based on Todani classification
Most commonly classified into 5 different types based on Todani classification
 Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis
Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis Most commonly classified into 5 different types based on Todani classification
Most commonly classified into 5 different types based on Todani classification
– 2003 modification of Todani classification incorporates presence of abnormal pancreaticobiliary junction (APBJ)
– Type I: Solitary fusiform or cystic dilation of extrahepatic bile duct (ED)
 Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)
Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)
 Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)
Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)– Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of ED located within duodenal wall
MR Findings
• Best noninvasive modality for assessing biliary tree, choledochal cysts, and anomalous pancreaticobiliary junction
• MRCP images nicely demonstrate cystic dilatation of biliary tree and relationship (and communication) of cysts with adjacent bile ducts
DIFFERENTIAL DIAGNOSIS
Malignant Common Bile Duct (CBD) Obstruction
• Often secondary to pancreatic adenocarcinoma, ampullary carcinoma, or distal CBD cholangiocarcinoma
Recurrent Pyogenic Cholangitis
• Formation of pigment stones throughout biliary tree (both intrahepatic and extrahepatic) with multiple biliary strictures, recurrent bouts of cholangitis, and dilatation of both intrahepatic and extrahepatic bile ducts
CLINICAL ISSUES
Presentation
Natural History & Prognosis
• Complications
 Stone formation most common complication (within cyst itself, gallbladder, intrahepatic ducts, or pancreatic duct)
Stone formation most common complication (within cyst itself, gallbladder, intrahepatic ducts, or pancreatic duct)
 Secondary biliary cirrhosis due to long-standing biliary obstruction or repeated bouts of cholangitis
Secondary biliary cirrhosis due to long-standing biliary obstruction or repeated bouts of cholangitis
 Stone formation most common complication (within cyst itself, gallbladder, intrahepatic ducts, or pancreatic duct)
Stone formation most common complication (within cyst itself, gallbladder, intrahepatic ducts, or pancreatic duct)
 Secondary biliary cirrhosis due to long-standing biliary obstruction or repeated bouts of cholangitis
Secondary biliary cirrhosis due to long-standing biliary obstruction or repeated bouts of cholangitisTreatment
• Treatment varies depending on type of choledochal cyst
 Type I and IV cysts: Surgical excision and reconstruction by Roux-en-Y hepaticojejunostomy due to risk of malignancy and complications (e.g., stones, cholangitis)
Type I and IV cysts: Surgical excision and reconstruction by Roux-en-Y hepaticojejunostomy due to risk of malignancy and complications (e.g., stones, cholangitis)
 Type I and IV cysts: Surgical excision and reconstruction by Roux-en-Y hepaticojejunostomy due to risk of malignancy and complications (e.g., stones, cholangitis)
Type I and IV cysts: Surgical excision and reconstruction by Roux-en-Y hepaticojejunostomy due to risk of malignancy and complications (e.g., stones, cholangitis)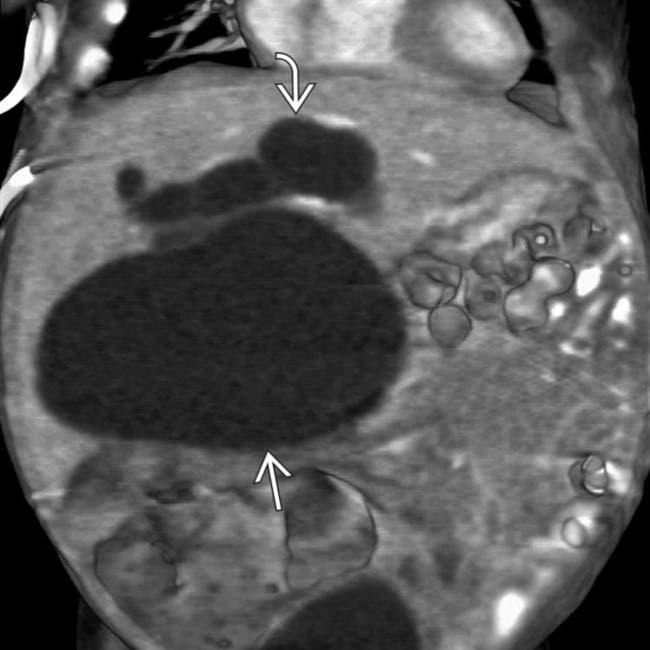
 , with a lesser degree of dilatation of the intrahepatic ducts
, with a lesser degree of dilatation of the intrahepatic ducts  , compatible with a type IVa choledochal cyst.
, compatible with a type IVa choledochal cyst.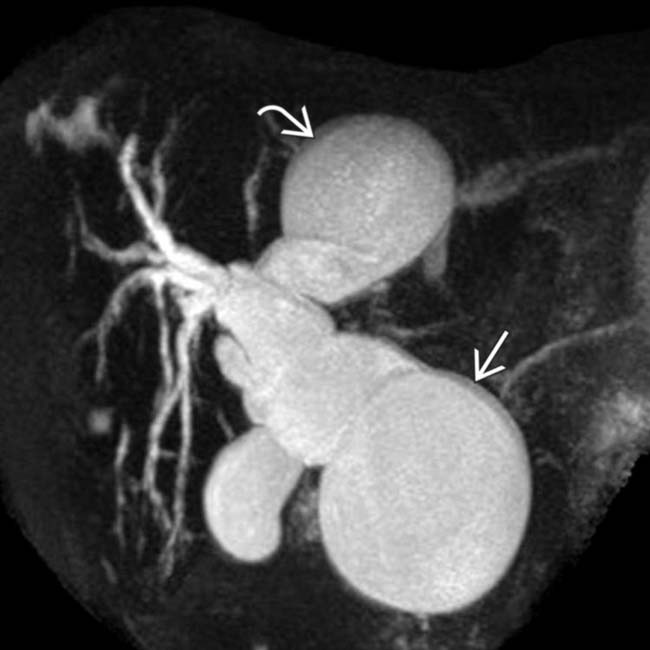
 , as well as focal cystic dilatation of the left hepatic duct
, as well as focal cystic dilatation of the left hepatic duct  , compatible with a type IVa choledochal cyst.
, compatible with a type IVa choledochal cyst.
 with a sudden transition to a normal distal bile duct
with a sudden transition to a normal distal bile duct  . This is a type IVa choledochal cyst.
. This is a type IVa choledochal cyst.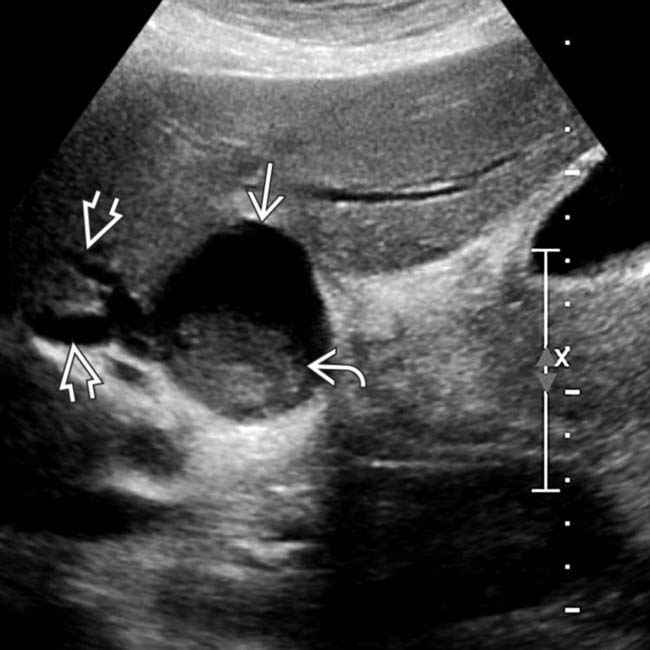
 with internal debris
with internal debris  arising in the porta hepatis. Note that the cyst communicates with mildly dilated intrahepatic ducts
arising in the porta hepatis. Note that the cyst communicates with mildly dilated intrahepatic ducts  , compatible with a choledochal cyst (probably type IVa).
, compatible with a choledochal cyst (probably type IVa).
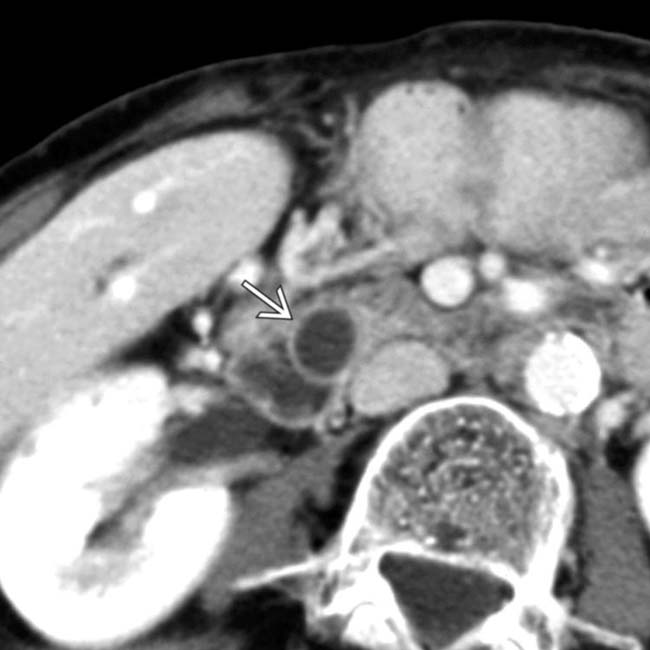
 within a type IV choledochal cyst, with marked dilation of the intrahepatic
within a type IV choledochal cyst, with marked dilation of the intrahepatic  and extrahepatic ducts (better seen on other sections).
and extrahepatic ducts (better seen on other sections).
 arising from the wall of the choledochal cyst. Both stones and cholangiocarcinoma are recognized complications of longstanding choledochal cysts.
arising from the wall of the choledochal cyst. Both stones and cholangiocarcinoma are recognized complications of longstanding choledochal cysts.
 .
.
 within the medial wall of the duodenum, while the rest of the biliary tree was normal in this type III choledochocele.
within the medial wall of the duodenum, while the rest of the biliary tree was normal in this type III choledochocele.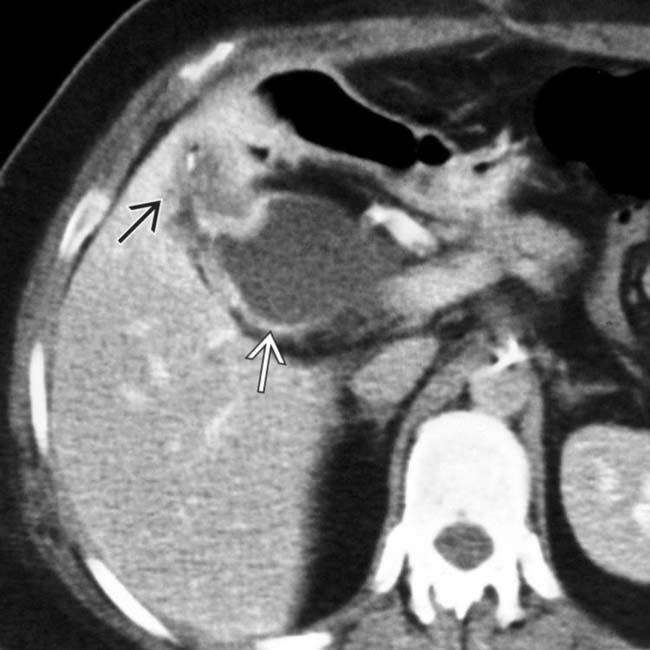
 with irregular wall thickening and a mass
with irregular wall thickening and a mass  invading the adjacent liver.
invading the adjacent liver.
 , as well as focal cystic dilatation of a segment of the left hepatic duct
, as well as focal cystic dilatation of a segment of the left hepatic duct  , in keeping with a type IV choledochal cyst.
, in keeping with a type IV choledochal cyst.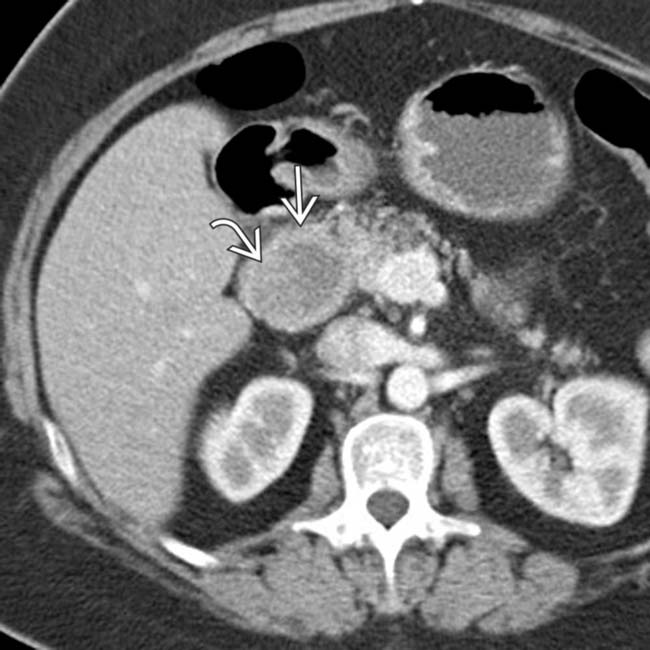
 of the extrahepatic bile duct, with subtle internal soft tissue
of the extrahepatic bile duct, with subtle internal soft tissue  within the duct at this site. This was found to be a cholangiocarcinoma arising within a type I choledochal cyst.
within the duct at this site. This was found to be a cholangiocarcinoma arising within a type I choledochal cyst.
 arising adjacent to the gallbladder and abutting the proximal CD. This cyst was resected and confirmed to be type II choledochal cyst, the most rare subtype.
arising adjacent to the gallbladder and abutting the proximal CD. This cyst was resected and confirmed to be type II choledochal cyst, the most rare subtype.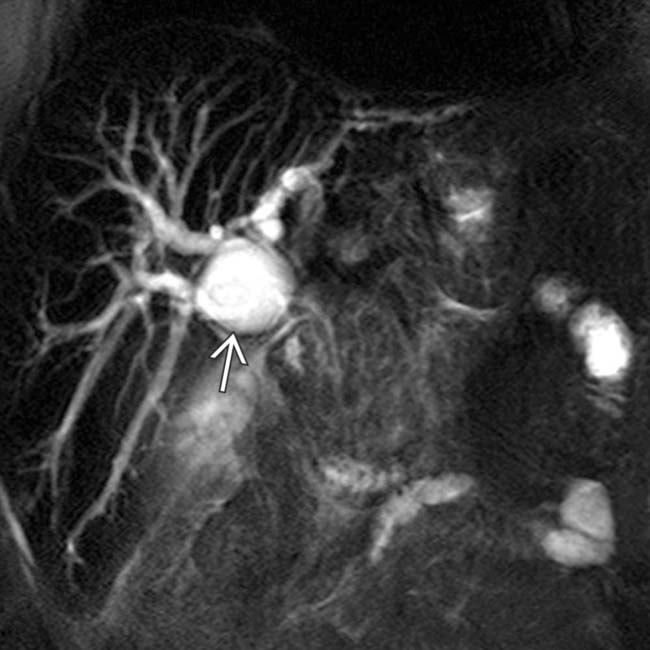
 of the proximal CBD, causing moderate dilatation of the upstream intrahepatic biliary tree, compatible with either a type I or IVa cyst.
of the proximal CBD, causing moderate dilatation of the upstream intrahepatic biliary tree, compatible with either a type I or IVa cyst.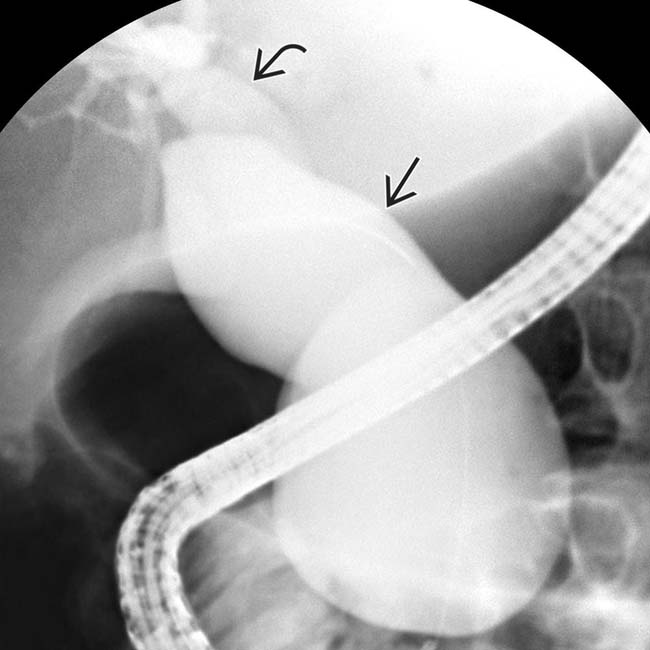
 . The intrahepatic ducts are moderately dilated
. The intrahepatic ducts are moderately dilated  . This constellation of findings is compatible with a type IVa choledochal cyst.
. This constellation of findings is compatible with a type IVa choledochal cyst.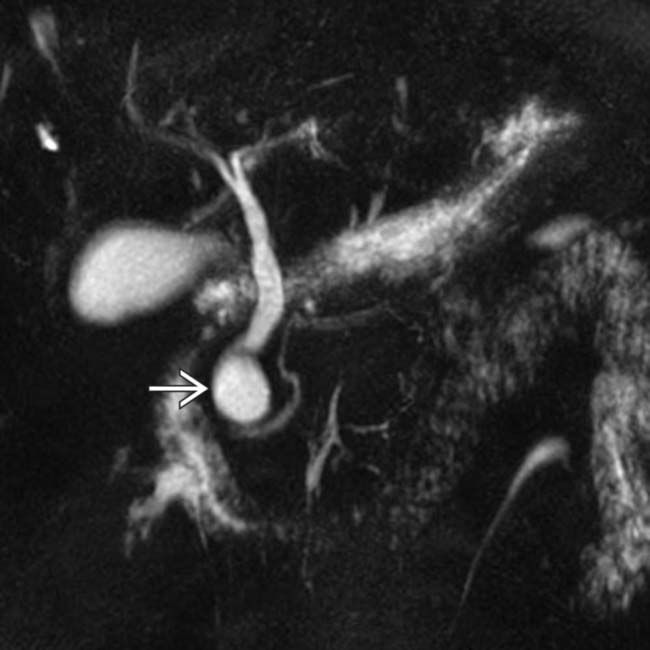
 of the distal CBD, in keeping with a type I choledochal cyst. Type I cysts can have either a fusiform or cystic morphology.
of the distal CBD, in keeping with a type I choledochal cyst. Type I cysts can have either a fusiform or cystic morphology.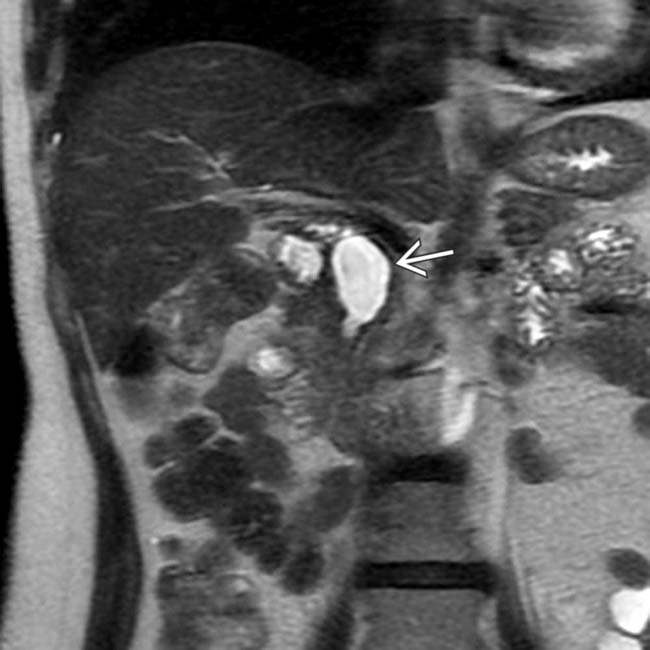
 of the extrahepatic bile duct, in keeping with a type I choledochal cyst. Type I cysts are the most common type, accounting for 50-85% of all choledochal cysts.
of the extrahepatic bile duct, in keeping with a type I choledochal cyst. Type I cysts are the most common type, accounting for 50-85% of all choledochal cysts.
 , a type I choledochal cyst in the Todani classification. This is the most common type of choledochal cyst.
, a type I choledochal cyst in the Todani classification. This is the most common type of choledochal cyst.




































































 .
.
 , plus moderate irregular dilation of the right and left main ducts, a type IVa choledochal cyst.
, plus moderate irregular dilation of the right and left main ducts, a type IVa choledochal cyst.
 , compatible with a type IVa choledochal cyst.
, compatible with a type IVa choledochal cyst.


