Chapter 69 Chest injuries
CHEST INJURIES
The majority of chest injuries in Australasia result from blunt trauma due to motor vehicle crashes. Less frequent causes include falls and penetrating injuries from stab or gunshot wounds. Associated extrathoracic injuries are common. Chest injuries account for a quarter of all trauma deaths. Immediate death from blunt chest trauma is usually due to blunt rupture of the thoracic aorta, heart or major vessel. Patients who survive the immediate posttrauma period may still have life-threatening injuries that require timely intervention. Most patients can be managed with simple measures, including intercostal tube drainage, analgesia, oxygen therapy and mechanical ventilation. Thoracotomy is infrequently required.1,2
IMMEDIATE MANAGEMENT
During the primary survey a rapid assessment of the respiratory, circulatory and neurological status of the patient is made (Table 69.1). Airway patency is ensured, oxygen administered by facemask and ventilation assessed. Obvious external bleeding is controlled. Two large bore intravenous cannulae are sited, blood samples taken for crossmatch, haematology and biochemistry tests, and intravenous fluids commenced. Intravenous opioid analgesia is given as repeated small boluses, titrated to effect. There are four critical chest injuries that should be sought during the primary survey for which immediate intervention may be life saving:
In addition, the clinical features of flail chest should be sought as these will no longer be apparent if positive-pressure ventilation is instituted (see below). A chest radiograph is integral to the initial assessment and should be performed promptly. Subcostal ultrasonography of the heart as part of the focused assessment with sonography for trauma (FAST) should be performed with penetrating chest trauma, or if there is haemodynamic instability.3 An ECG is important in the assessment for blunt cardiac injury (see below).4
Endotracheal intubation and mechanical ventilation are indicated for the patient with a compromised airway, severe head injury, or gross hypoventilation and/or hypoxaemia not attributable to pneumothorax. Haemodynamic instability should be anticipated (Table 69.2). Emergency cricothyroidotomy or tracheostomy is only rarely required when an airway obstruction cannot be bypassed by translaryngeal intubation. A nasogastric tube (or orogastric, if facial injuries are suspected) should be inserted to decompress the stomach after endotracheal intubation.
Table 69.2 Causes of cardiovascular collapse on induction of anaesthesia and positive-pressure ventilation in chest-injured patients
PNEUMOTHORAX
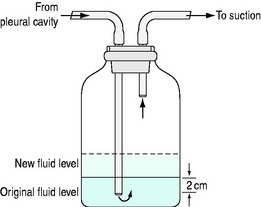
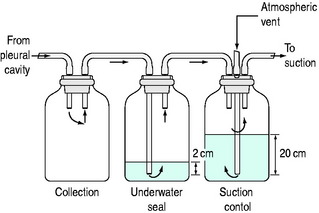
Pneumothorax visible on the initial chest radiograph should be treated with insertion of an intercostal tube connected to an underwater seal drainage system (Figure 69.1). A single-bottle drainage system without suction is usually adequate. Low-pressure suction (20 cmH2O) is applied if the pneumothorax fails to fully resolve, or if there is associated haemothorax (Figure 69.2). A three-bottle system (or commercially available three-in-one system) allows more accurate control of suction (Figure 69.3). Presumptive antibiotics are not indicated.5
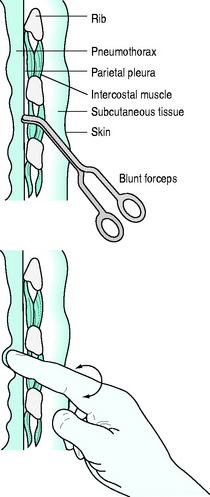
Figure 69.1 Intercostal tube insertion. After sterile preparation and drape, 1% lidocaine is infiltrated in the mid-axillary line at the level of the nipple. A 2–3 cm transverse skin incision is made. Dissection is performed by blunt forceps down to the pleura, passing just superior to the rib surface to avoid injury to neurovascular structures. A gloved finger is used to confirm separation of lung from chest wall. A large bore (32 French) intercostal tube is inserted without a trocar and directed anteriorly for pneumothorax or posteriorly for haemothorax. Curved forceps clamped to the tip of the tube can be used to guide the tube through the chest wall. The tube is immediately connected to an underwater seal drainage system (Figures 69.2 and 69.3) and checked for satisfactory drainage and tidal rise and fall in fluid level with respiration. Non-absorbable sutures are used to seal the skin incision around the tube and secure the tube. The intrathoracic position of the tube is checked with a chest radiograph.
If tension pneumothorax is suspected clinically an intercostal tube should be inserted immediately, prior to the chest radiograph. Needle thoracostomy with a large bore cannula inserted into the second intercostal space in themidclavicular line may be used to drain air more rapidly for patients in extremis. However, this is rarely necessary and may puncture the lung, fail to reach the pleural space, or kink when the needle is removed from within the cannula. Whether successful or not, needle thoracostomy must be followed by formal intercostal tube drainage.
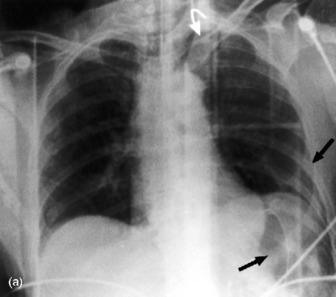
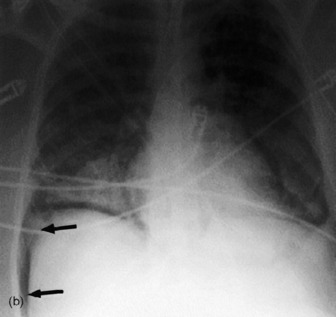
Simple pneumothorax may develop tension at any stage, especially with positive-pressure ventilation (Table 69.2). A small pneumothorax may be missed on the initial chest radiograph. In the supine position pleural air collects anteroinferiorly and is demonstrated radiologically by a deep sulcus sign or increased radiolucency of one side of the chest compared to the other (Figure 69.4).6
Occult pneumothorax is defined as visible on chest CT (or upper slices of an abdominal CT) but not plain radiograph.7 Drainage is not mandatory, but should be considered if prolonged surgery is anticipated, there is significant cardiorespiratory compromise or interhospital transport is necessary. With a conservative approach the patient should be carefully monitored for deterioration from expansion of the pneumothorax.7
Subcutaneous emphysema over the chest wall in a patient with blunt chest trauma is almost always associated with pneumothorax, but should raise suspicion of other injuries (Table 69.3). The pneumothorax may not be visible on the plain chest radiograph, either because it is obscured by the emphysema or because it has largely decompressed into subcutaneous tissues. An intercostal tube should be inserted.
Table 69.3 Causes of pneumothorax, subcutaneous emphysema and/or pneumomediastinum
If there is no associated fluid collection the chest tube can be removed once the pneumothorax is no longer visible on chest radiograph and there has been no air drained for at least 24 hours. Persistent air leak and incomplete drainage of a pneumothorax after intercostal tube insertion should prompt investigation for tracheobronchial injury. However, the depth of the tube within the pleural space and tubing connections should be checked to ensure that extraneous air is not being inadvertently entrained. Incomplete drainage with no air leak is usually due to tube malplacement.
HAEMOTHORAX
Haemothorax visible on chest radiography should be drained as completely as possible (Figure 69.1). The tube can be removed once radiographic clearance is achieved, with < 100 ml/24 hours drainage. A small haemothorax (< 300 ml) (visible on ultrasound or CT) may initially be managed conservatively, but should be drained if it enlarges.
Massive haemothorax, defined as > 1500 ml, causes life-threatening circulatory compromise fromhypovolaemia and vena caval compression as well as hypoxaemia. This requires immediate tube drainage. If the amount of ongoing bleeding following initial drainage is low, the patient remains haemodynamically stable after initial resuscitation, and the blood is venous in appearance, the patient can be managed with close observation. Ongoing bleeding of > 200 ml/h, or > 600 ml over 6 hours (massive haemothorax equivalent), is an indication to proceed to thoracotomy.
PERICARDIAL TAMPONADE
Pericardial tamponade should be suspected in any patient with a gunshot wound to the chest or stab wound to the precordium. It occurs rarely with blunt trauma, but should be suspected if there is hypotension out of proportion to blood loss, and distended neck veins. Pulsus paradoxus may be detected in the spontaneously breathing patient. The differential diagnosis includes tension pneumothorax (most likely) and cardiogenic shock from severe blunt cardiac injury or delayed and inadequate resuscitation. Pericardial fluid can be detected with ultrasound (FAST scan).3 Cardiac structures are imaged via a subcostal view using a low-frequency transducer (3.5 MHz) to provide good tissue depth penetration. Echocardiography, or operative subxiphoid window, can be used if diagnostic uncertainty remains.
Haemodynamically unstable patients should undergo thoracotomy.8 Subxiphoid pericardiotomy can be performed in selected stable patients, but may require conversion to open thoracotomy. Needle pericardiocentesis is rarely effective in the acute setting, but may have a role in the drainage of delayed pericardial effusions following stab wounds.8
CARDIAC ARREST AND EMERGENCY THORACOTOMY
External cardiac massage is invariably unsuccessful in the trauma setting. Indeed, cardiac compression may cause further injury to intrathoracic structures and obstruct access to the patient for more potentially useful interventions such as (bilateral) intercostal tube insertion. For patients with witnessed loss of vital signs after penetrating chest trauma, emergency thoracotomy should be considered if suitably experienced medical personnel are available.8 This is rarely successful for blunt trauma. The standard approach is a left-sided anterolateral thoracotomy. This allows access to the thoracic cavity for specific interventions:8
These temporising (damage control) measures are followed by transfer to the operating room for completion of surgery:9
SPECIFIC INJURIES
Specific chest injuries should be systematically excluded. Imaging techniques play an important role. Choice of investigation is influenced by clinical findings. The degree of haemodynamic and respiratory instability will determine whether the patient can be moved to an imaging facility. Local availability of equipment and clinician expertise may limit the options available. Extrathoracic injuries will often determine investigation and management priorities. With the advent of rapid high-resolution CT scanners, routine chest CT has become increasing popular, particularly in patients who require abdominal or head CT.10 Endotracheal intubation and mechanical ventilation may be required to facilitate investigations (e.g. the combative trauma patient with ethanol intoxication).
BLUNT AORTIC INJURY
Blunt aortic injury usually occurs at the junction between the mobile arch and fixed descending aorta, just distal to the origin of the left subclavian artery, as a result of severe deceleration injury. Less frequently, the ascending aorta or arch vessels are injured by direct trauma. Blunt aortic injuries may be divided into:11
Most patients with blunt aortic injury die at the scene from complete aortic wall transection or associatedinjuries. Of those that reach hospital, 90% will have a significant injury.11 Clinical signs include unequal upper limb pulses, pseudocoarctation or interscapular murmur, but these are rarely detected.12 Aortic injury should be suspected if the mechanism of injury is suggestive of rapid deceleration, such as high speed (greater than 90 km/h) motor vehicle or motorcycle crashes, or a pedestrian hit by a vehicle.13
Historically, chest radiography has been the screening test (to detect mediastinal haematoma) and aortic angiography the diagnostic test for blunt aortic injury.12,14 More recently, CT and echocardiography have been introduced for screening and diagnostic purposes:15
| Signs of periaortic haematoma | Indirect signs |
|---|---|
| Widened mediastinum (> 8 cm) | Left haemothorax |
| Obscured aortic knuckle | Left pleural cap |
| Opacification of aortopulmonary window | Fractured first or second ribs |
| Deviation of trachea, left main bronchus or nasogastric tube | |
| Thickened paratracheal stripe |
Table 69.5 Signs of aortic branch vessel injury
Significant aortic injury requires prompt surgical or endoluminal stent repair.21 However, this should not take priority over other life-saving operations (e.g. craniotomy or laparotomy).12 Surgical options include direct repair (clamp and sew) or techniques that maintain distal aortic perfusion.14 The latter reduce the risk of postoperative paraplegia from spinal cord ischaemia, but often require systemic heparinisation, which may exacerbate bleeding from other injuries.15 Surgery should be deferred, sometimes indefinitely, if severe associated injuries or comorbidities make the operative risk unacceptably high.12,22 In such cases endoluminal stent repair may still be feasible.21 Conservative management includes antihypertensive therapy (β-blockers ± vasodilators) and serial imaging to assess for expanding pseudoaneurysm that will require intervention. Minimal aortic injury may also be managed expectantly.11,15,20
BLUNT CARDIAC INJURY
Blunt cardiac injury results from compression of the heart between the sternum and the spine, abrupt pressure changes within cardiac chambers or deceleration shear injury. A wide spectrum of injuries has been described, but may be classified according to the clinical sequelae and need for intervention:4
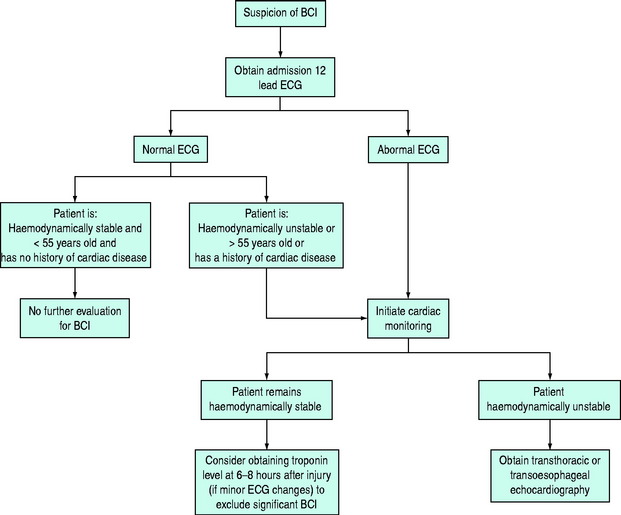
All patients should have an ECG on admission (Figure 69.5). If this is normal and the patient is young, haemodynamically stable, and has no history of cardiac disease, the risk of significant injury is very low and no further cardiac evaluation is required. Other patients should be monitored for late sequelae of significant cardiac injury (arrhythmia or heart failure).4 Patients who remain haemodynamically stable, with only minor ECG changes, and who have a normal troponin level at 6–8 hours post injury, have a low risk of cardiac complications.4,23 Echocardiography is indicated for patients with hypotension unexplained by other injuries, heart failure, or persistent arrhythmias.4 Undisplaced sternal fracture does not of itself warrant cardiac evaluation.24
TRACHEOBRONCHIAL INJURY
Blunt rupture of the trachea or bronchi results from crush injury or rapid deceleration with shearing of the airway between a fixed trachea and mobile lungs. The proximal right main bronchus is the most common site of injury.25 Large injuries present with respiratory distress, subcutaneous emphysema and haemoptysis (Table 69.3).26 The chest radiograph demonstrates pneumothorax and mediastinal emphysema. Dramatic deterioration may follow the institution of positive-pressure ventilation (Table 69.2). With smaller injuries, initial findings are often overshadowed by associated injuries with delay in diagnosis. Persistent pneumothorax with a large air leak, or recurrentpneumothoraces and pulmonary collapse, should prompt further investigation. Flexible bronchoscopy confirms the diagnosis and identifies the level of injury. Treatment is usually primary repair, although non-operative management has been described.27 Late complications of either approach include postobstructive pneumonia, empyema or bronchiectasis.25
DIAPHRAGMATIC RUPTURE AND DIAPHRAGMATIC PARESIS
The usual mechanism of diaphragmatic rupture is gross abdominal compression from direct vehicular intrusion. The risk of rupture is higher with lateral impact collisions, but not seat belt use.28 Associated injuries are very common.28 Rupture of the left hemidiaphragm is more common, because the right hemidiaphragm is congenitally stronger and protected by the liver.
Symptoms (dyspnoea and chest pain) are non-specific. Rarely bowel sounds are audible on chest auscultation. Diagnostic chest radiograph findings are herniation of bowel into the thoracic cavity and nasogastric tube above the left hemidiaphragm. Indirect signs include an elevated or distorted diaphragmatic outline, or pleural effusion, but these may be obscured by adjacent pulmonary pathology, phrenic nerve injury or with positive-pressure ventilation.29 The low diagnostic accuracy of chest radiography often results in delayed diagnosis unless further imaging is performed. Multidetector CT has high diagnostic accuracy, but magnetic resonance imaging or video thorascopy may be required if uncertainty persists.29–31 Prompt operative repair is important to prevent bowel incarceration or perforation. The choice of surgical approach (laparotomy or thoracotomy) is dictated by associated injuries.
OESOPHAGEAL INJURY
Rupture of the oesophagus from blunt trauma is rare. Penetrating trauma usually causes injury to the cervical portion of the oesophagus. Oesophageal injury may also result from attempted endotracheal intubation or gastric tube insertion during resuscitation of the trauma patient.32 Clinical features include chest pain, dysphagia, pain on swallowing and subcutaneous emphysema (Table 69.3). Chest radiograph findings include pneumothorax and/or hydrothorax, mediastinal emphysema or widened mediastinum.26 Prompt diagnosis by oesophagoscopy or gastrograffin swallow is important. Treatment is immediate surgical repair.32 Delayed recognition or repair (more than 12 hours post injury) leads to septic shock from mediastinal contamination. Extensive irrigation and drainage are then required, but postoperative complications are common.32
PULMONARY INJURY
Pulmonary contusion is characterised by interstitial haemorrhage and oedema, with a secondary inflammatory reaction. Clinically, there is increased work of breathing, impaired gas exchange and sometimes haemoptysis. The chest radiograph demonstrates patchy interstitial infiltrates or consolidation not confined to anatomical segments. Gas exchange and radiographic findings may initially be unremarkable, with deterioration over the first 24–48 hours.2,6 CT is more sensitive at detecting contusion, and quantification of lung volume affected predicts risk of acute respiratory distress syndrome (ARDS).33 In the absence of complications (ARDS, pneumonia or aspiration), clinical and radiological recovery can be expected within 3–5 days.6,33
Treatment is supportive with humidified oxygen therapy, and encouragement of deep breathing and coughing in the spontaneously breathing patient. Non-invasive ventilation can be used in selected patients if gas exchange is poor. Intubation and mechanical ventilation are indicated for refractory hypoxaemia, or if intubation is required for non-pulmonary reasons. Routine corticosteroids are not indicated. Antibiotics should be reserved for superimposed pneumonia.2
Pulmonary laceration occurs when disruption of lung architecture, with formation of an air- or blood-filled cavity, occurs after blunt or penetrating trauma.6 On chest radiography lacerations are often initially obscured by adjacent contusion, but typically take many weeks to resolve, and may be complicated by abscess formation or bronchopleural fistula.6
BONY INJURIES
Half of all rib fractures are missed on plain chest radiography, but should be suspected if there is localised tenderness over the chest wall. Good analgesia to prevent pulmonary complications from sputum retention is essential.34 This risk may not be clinically apparent initially, but deterioration in respiratory status over the next few days should be anticipated, especially in the elderly, smokers or patients with pre-existing pulmonary disease. First and second rib fractures, scapula fracture and sternoclavicular dislocation are markers of high-energy trauma.6
Most sternal fractures occur in restrained occupants involved in frontal impact vehicular crashes. Associatedthoracolumbar spine fractures are common.24 Blunt cardiac injury should be suspected with displaced sternal fractures.24
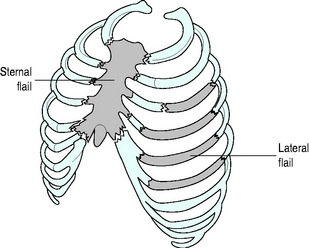
FLAIL CHEST
Fracture of at least four consecutive ribs in two or more places results in a flail segment with paradoxical movement of the chest wall during tidal breathing (Figure 69.6).2 Associated pulmonary contusion is often present. Younger patients with no other major injuries, no pulmonary comorbidities, and good analgesia can often be managed with non-invasive ventilation or oxygen therapy alone.35 Deteriorating gas exchange and sputum retention are indications for intubation and mechanical ventilation. Prolonged ventilatory support is often not necessary in patients whose associated injuries and comorbidities are not severe. Surgical stabilisation has been advocated for severe flail to reduce the duration of ventilation.36
EXTRAPLEURAL HAEMATOMA
Traumatic extrapleural haemorrhage arises when chest wall bleeding does not enter the pleural space.37 Chest radiography shows a parietal shadow that does not cause blunting of the costophrenic angle or shift with gravity. A large haematoma should be evacuated with a chest tube or by thoracotomy.
SYSTEMIC AIR EMBOLISM
This is more frequent with penetrating injuries and is immediately life threatening. The typical presentation is circulatory collapse after institution of positive-pressure ventilation, when the pulmonary airspace pressure exceeds pulmonary venous pressure (Table 69.2). Focal neurological changes in the absence of head injury also suggest the diagnosis. Characteristic head CT findings have been described.38
When suspected, maintenance of spontaneous ventilation is preferred. If positive-pressure ventilation is necessary, an FiO2 of 1.0 should be used, with ventilatory pressures and volumes reduced to a minimum. Selective lung ventilation, using a double lumen endotracheal tube or bronchial blocker, and/or high frequency ventilation, should be considered.8 However, urgent thoracotomy, with hilar clamping or lung isolation, is usually indicated.8 Hyperbaric oxygen therapy has been used to treat cerebral air embolism, but is often impractical.38
COMPLICATIONS AND ICU MANAGEMENT
On admission to ICU, rewarming, correction of coagulopathy and ongoing fluid resuscitation are often required. Pericardial tamponade and persistent air leak should be anticipated in post-thoracotomy patients.9 A restrictive approach to fluid therapy is indicated for patients who have undergone lung surgery. However, care should be taken to ensure adequate fluid resuscitation. A judicious transfusion policy should be employed with all patients.39
As with other critically ill or injured patients, prophylactic measures against thromboembolism40 and upper gastrointestinal stress ulceration should be used. Adequate nutrition is important to ameliorate the hypermetabolic and catabolic metabolic changes, reduce the incidence of sepsis, and improve outcome. Nutrition should be instituted early, preferably via the enteral route. Nasogastric feeding may be limited by gastric stasis, in which case nasojejunal feeding is usually successful.
ACUTE RESPIRATORY FAILURE AND MECHANICAL VENTILATION
ANALGESIA
Adequate analgesia is essential for deep breathing and effective coughing, which, if achieved, will reduce the likelihood that endotracheal intubation is needed for less severely injured patients. Analgesia also facilitates chest physiotherapy and early mobilisation, reducing pulmonary morbidity. The choice of analgesia depends on the severity of illness and may vary over time. Options include:34
PNEUMONIA
Sepsis is the principal cause of late death after major trauma. Breach of the skin surface barrier, devitalised tissues, and the presence of invasive drains and catheters make the trauma patient especially prone to bacterial invasion. In the chest-injured patient, pulmonary contusion, emergency intubation, shock, blood transfusion and the presence of extrathoracic injuries increase the risk of nosocomial pneumonia.42
The diagnosis of pneumonia is suspected if there are new or progressive infiltrates on the chest radiograph and deterioration in respiratory status. However, new infiltrates may also be caused by pulmonary contusion, pleural fluid collections, atelectasis, aspiration and pulmonary oedema. Infection is supported by the presence of purulent sputum, new fever and leukocytosis. Confirmation depends on culture of tracheal aspirate or bronchoscopic samples.43 Antibiotic therapy should be targeted at causative organisms. Prompt empiric antibiotics should be started in unstable patients, with re-evaluation at 48–72 hours.
Preventative measures include careful hand cleansing, reduced duration of intubation and ventilation, semirecumbent position, enteral nutrition, avoidance of excessive sedation or hyperglycaemia, and avoidance of prolonged prophylactic antibiotics.43 The role of selective decontamination of the digestive tract remains controversial.
RETAINED HAEMOTHORAX AND EMPYEMA
If the initial chest tube is poorly positioned or blocked, a second tube may be placed through a different skin incision, preferably under ultrasound or CT guidance. In the absence of a bleeding diathesis or empyema formation, early evacuation of retained haemothorax (within a few days of the initial haemothorax) can be attempted with intrapleural administration of a thrombolytic agent. Streptokinase 250 000 units, or urokinase 100 000 units, in 100 ml saline is instilled into the intercostal tube for 4 hours each day until resolution of haemothorax with minimal further drain losses.44 Alternatively, video-assisted thoracoscopic surgery (VATS) may be used in haemodynamically stable patients who can tolerate single lung ventilation.30,31 Failure of these techniques, or empyema formation, requires formal thoracotomy ± decortication.
FAT EMBOLISM SYNDROME
Fat embolism invariably occurs in patients with long bone fractures.45 Although fat embolism syndrome (with pulmonary, neurological and cutaneous sequelae) is uncommon, oxygen desaturation occurs frequently, and may be more severe and prolonged in patients with parenchymal lung injury.46 Treatment is supportive, but early resuscitation and fracture stabilisation are important preventative measures.45 Early (< 24 hours) intramedullary nailing is the fixation method of choice, resulting in fewer orthopaedic complications than other fixation methods, and fewer pulmonary complications than delayed surgery.47 However, internal fixation may provoke further fat embolism, require a longer operative time, and result in more blood loss than external fixation.47 Thus, in severely chest-injured patients, temporary stabilisation using external fixation, with intramedullary nailing several days later, is preferred.47
PROGNOSIS
Reported mortality rates for chest-injured patients vary greatly, reflecting the severity of chest injury and associated extrathoracic injuries. Initial physiological markers that predict adverse outcome are low Glasgow Coma Scale score, hypotension and high respiratory rate. In patients with severe blunt trauma, mortality is significantly higher with bilateral than unilateral chest injuries, and depends more on the extent of parenchymal lung injury than the extent of chest wall injury.48 Older age correlates strongly with worse outcome, even though the elderly are more likely to suffer rib fractures than parenchymal lung injury.48 In the elderly, the risk of death or pneumonia increases with each additional rib fractured. In younger patients, better physiological reserve means that outcome is only significantly worsened if four or more ribs are fractured.34,49 Obese patients (BMI > 30) are likely to suffer more complications during hospitalisation than non-obese patients.50
1 Kulshrestha P, Munshi I, Wait R. Profile of chest trauma in a level I trauma center. J Trauma. 2004;57:576-581.
2 Wanek S, Mayberry JC. Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20:71-81.
3 Scalea TM, Rodriguez A, Chiu WC, et al. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma. 1999;46:466-472.
4 Schultz JM, Trunkey DD. Blunt cardiac injury. Crit Care Clin. 2004;20:57-70.
5 Maxwell RA, Campbell DJ, Fabian TC, et al. Use of presumptive antibiotics following tube thoracostomy for traumatic hemopneumothorax in the prevention of empyema and pneumonia – a multi-center trial. J Trauma. 2004;57:742-748. discussion 748–9
6 Miller LA. Chest wall, lung, and pleural space trauma. Radiol Clin North Am. 2006;44:213-224. viii
7 Ball CG, Kirkpatrick AW, Laupland KB, et al. Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J Trauma. 2005;59:917-924. discussion 924–5
8 Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma – a review. Injury. 2006;37:1-19.
9 Rotondo MF, Bard MR. Damage control surgery for thoracic injuries. Injury. 2004;35:649-654.
10 Guerrero-Lopez F, Vazquez-Mata G, Alcazar-Romero PP, et al. Evaluation of the utility of computed tomography in the initial assessment of the critical care patient with chest trauma. Crit Care Med. 2000;28:1370-1375.
11 Malhotra AK, Fabian TC, Croce MA, et al. Minimal aortic injury: a lesion associated with advancing diagnostic techniques. J Trauma. 2001;51:1042-1048.
12 Nagy K, Fabian T, Rodman G, et al. Guidelines for the diagnosis and management of blunt aortic injury: an EAST Practice Management Guidelines Work Group. J Trauma. 2000;48:1128-1143.
13 Dyer DS, Moore EE, Ilke DN, et al. Thoracic aortic injury: how predictive is mechanism and is chest computed tomography a reliable screening tool? A prospective study of 1,561 patients. J Trauma. 2000;48:673-682. discussion 682–3
14 Fabian TC, Richardson JD, Croce MA, et al. Prospective study of blunt aortic injury: multicenter trial of the American Association for the Surgery of Trauma. J Trauma. 1997;42:374-380. discussion 380–3
15 Degiannis E, Boffard K. Critical decisions in trauma of the thoracic aorta. Injury. 2002;33:317-322.
16 Wong YC, Ng CJ, Wang LJ, et al. Left mediastinal width and mediastinal width ratio are better radiographic criteria than general mediastinal width for predicting blunt aortic injury. J Trauma. 2004;57:88-94.
17 Mirvis SE. Thoracic vascular injury. Radiol Clin North Am. 2006;44:181-197. vii
18 Holdgate A, Dunlop S. Review of branch aortic injuries in blunt chest trauma. Emerg Med Australas. 2005;17:49-56.
19 Cinnella G, Dambrosio M, Brienza N, et al. Transesophageal echocardiography for diagnosis of traumatic aortic injury: an appraisal of the evidence. J Trauma. 2004;57:1246-1255.
20 Vignon P, Martaille JF, Francois B, et al. Transesophageal echocardiography and therapeutic management of patients sustaining blunt aortic injuries. J Trauma. 2005;58:1150-1158.
21 Andrassy J, Weidenhagen R, Meimarakis G, et al. Stent versus open surgery for acute and chronic traumatic injury of the thoracic aorta: a single-center experience. J Trauma. 2006;60:765-771. discussion 771–2
22 Hirose H, Gill IS, Malangoni MA. Nonoperative management of traumatic aortic injury. J Trauma. 2006;60:597-601.
23 Rajan GP, Zellweger R. Cardiac troponin I as a predictor of arrhythmia and ventricular dysfunction in trauma patients with myocardial contusion. J Trauma. 2004;57:801-808. discussion 808
24 von Garrel T, Ince A, Junge A, et al. The sternal fracture: radiographic analysis of 200 fractures with special reference to concomitant injuries. J Trauma. 2004;57:837-844.
25 Kiser AC, O’Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg. 2001;71:2059-2065.
26 Euathrongchit J, Thoongsuwan N, Stern EJ. Nonvascular mediastinal trauma. Radiol Clin North Am. 2006;44:251-258. viii
27 Self ML, Mangram A, Berne JD, et al. Nonoperative management of severe tracheobronchial injuries with positive end-expiratory pressure and low tidal volume ventilation. J Trauma. 2005;59:1072-1075.
28 Reiff DA, McGwin GJr, Metzger J, et al. Identifying injuries and motor vehicle collision characteristics that together are suggestive of diaphragmatic rupture. J Trauma. 2002;53:1139-1145.
29 Iochum S, Ludig T, Walter F, et al. Imaging of diaphragmatic injury: a diagnostic challenge? Radiographics. 2002;22(Spec No):S103-S116. discussion S116–8
30 Carrillo EH, Richardson JD. Thoracoscopy for the acutely injured patient. Am J Surg. 2005;190:234-238.
31 Lowdermilk GA, Naunheim KS. Thoracoscopic evaluation and treatment of thoracic trauma. Surg Clin North Am. 2000;80:1535-1542.
32 Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma. 2001;50:289-296.
33 Miller PR, Croce MA, Bee TK, et al. ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma. 2001;51:223-228. discussion 229–30
34 Simon BJ, Cushman J, Barraco R, et al. Pain management guidelines for blunt thoracic trauma. J Trauma. 2005;59:1256-1267.
35 Gunduz M, Unlugenc H, Ozalevli M, et al. A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 2005;22:325-329.
36 Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002;52:727-732. discussion 732
37 Rashid MA, Wikstrom T, Ortenwall P. Nomenclature, classification, and significance of traumatic extrapleural hematoma. J Trauma. 2000;49:286-290.
38 Ho AM, Ling E. Systemic air embolism after lung trauma. Anesthesiology. 1999;90:564-575.
39 Croce MA, Tolley EA, Claridge JA, et al. Transfusions result in pulmonary morbidity and death after a moderate degree of injury. J Trauma. 2005;59:19-23. discussion 24
40 Knudson MM, Ikossi DG. Venous thromboembolism after trauma. Curr Opin Crit Care. 2004;10:539-548.
41 Fan E, Needham DM, Stewart TE. Ventilatory management of acute lung injury and acute respiratory distress syndrome. JAMA. 2005;294:2889-2896.
42 Croce MA, Tolley EA, Fabian TC. A formula for prediction of posttraumatic pneumonia based on early anatomic and physiologic parameters. J Trauma. 2003;54:724-729. discussion 729–30
43 Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388-416.
44 Inci I, Ozcelik C, Ulku R, et al. Intrapleural fibrinolytic treatment of traumatic clotted hemothorax. Chest. 1998;114:160-165.
45 White T, Petrisor BA, Bhandari M. Prevention of fat embolism syndrome. Injury. 2006;37(Suppl 4):S59-S67.
46 Wong MW, Tsui HF, Yung SH, et al. Continuous pulse oximeter monitoring for inapparent hypoxemia after long bone fractures. J Trauma. 2004;56:356-362.
47 Pape HC, Giannoudis P, Krettek C. The timing of fracture treatment in polytrauma patients: relevance of damage control orthopedic surgery. Am J Surg. 2002;183:622-629.
48 Pape HC, Remmers D, Rice J, et al. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496-504.
49 Brasel KJ, Guse CE, Layde P, et al. Rib fractures: relationship with pneumonia and mortality. Crit Care Med. 2006;34:1642-1646.
50 Brown CV, Neville AL, Rhee P, et al. The impact of obesity on the outcomes of 1,153 critically injured blunt trauma patients. J Trauma. 2005;59:1048-1051. discussion 1051