Chest Imaging
After reading this chapter, you will be able to:
1. Describe how the chest radiograph is produced.
2. Define the terms radiolucent and radiopaque.
3. Discuss how the appearance of a certain organ or tissue on a radiograph depends on its density.
4. Explain how the spatial relationship between the x-ray source, the patient, and the x-ray film affects the magnification of images on the radiograph. Identify the clinical indications for the use of a chest radiograph.
5. Discuss different types of radiograph orientations.
6. Recognize the proper technique for performing a systematic descriptive evaluation (interpretation) of the chest radiograph.
7. Explain the significance of the following special radiographic evaluation signs:
8. Discuss the limitations of the chest radiograph.
9. Appraise the typical clinical and chest radiographic findings for the following lung disorders:
10. Describe the correct position for endotracheal tube placement as seen on a chest radiograph.
11. Identify the value and limitations of using radiographs to determine a position of tubes and catheters
12. List situations that require obtaining a postprocedure chest radiograph.
13. Explain the technique, indications, and advantages and disadvantages for computed tomography scanning.
14. Discuss the relative use and indications for magnetic resonance imaging in lung disease.
15. Explain the technique and indications for performing nuclear medicine lung scans.
16. Explain the technique and indications for the use of pulmonary angiography.
17. Discuss the utility of ultrasound, fluoroscopy, and interventional radiology in diagnosis and treatment of lung diseases.
Production of the Radiograph
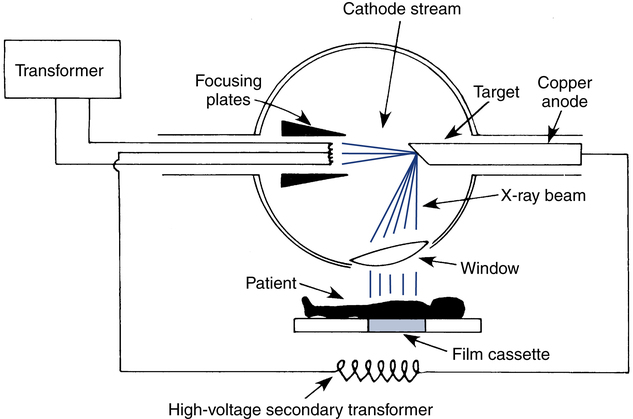
On striking the target, the electrons undergo physical changes that result in the emission of x-rays. The origins of the name x-rays are rather remarkable. Wilhelm Roentgen, a physicist from the 19th century, who is unanimously credited for the discovery of x-rays, was experimenting with various types of electromagnetic radiation. He called a particular type of radiation that he was studying x-rays, “x” for the unknown. Since then, the electromagnetic radiation in general and x-rays in particular have been extensively studied, but the name x-rays still persists, although in some countries they are referred to as Roentgen radiation. These x-rays are emitted in all directions, but because of the construction of the tube, only the few that escape through the window are actually used; the rest are absorbed harmlessly into the wall of the x-ray machine (Fig. 10-1). X-rays are not reflected like light rays but penetrate most matter. Their ability to penetrate matter depends on the density of the matter. Dense objects, such as bone, absorb more x-rays (allow less penetration) than air-filled objects, such as lung tissue.
Indications for the Chest Radiograph Examination
• Detecting alterations of the lung caused by pathologic processes
• Determining the appropriate therapy
• Evaluating the effectiveness of treatment
• Determining the position of tubes and catheters
Although only the physician can order a chest radiograph, the respiratory therapist (RT) may want to suggest to the attending physician that a chest image may be needed in certain circumstances. For example, an undiagnosed pneumothorax may suddenly cause deterioration of a mechanically ventilated patient. In the setting of a tension pneumothorax (discussed in detail later in this chapter), there may not be time even for an urgent radiograph, and treatment may have to be started solely on clinical grounds. However, in a less urgent situation, a portable chest film may be very helpful in confirming the suspected pneumothorax. The RT is often at the bedside of the mechanically ventilated patient and may be the first person to see the signs consistent with a pneumothorax, or another potentially serious complication, and would be the first to recognize the need for an urgent chest radiograph. For this reason, all RTs should be familiar with the clinical indications for a chest radiograph (Box 10-1).
Evaluation of the Chest Radiograph
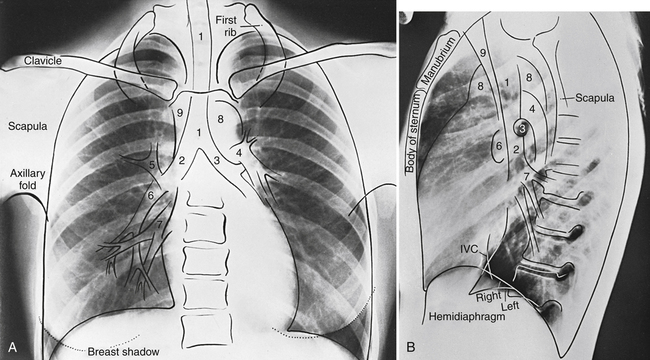
Familiarity with the anatomic landmarks seen on normal chest images is extremely helpful in learning to recognize abnormalities. Figure 10-2 identifies the important landmarks on a normal PA chest radiograph.
Systematic Approach to the Chest Radiograph
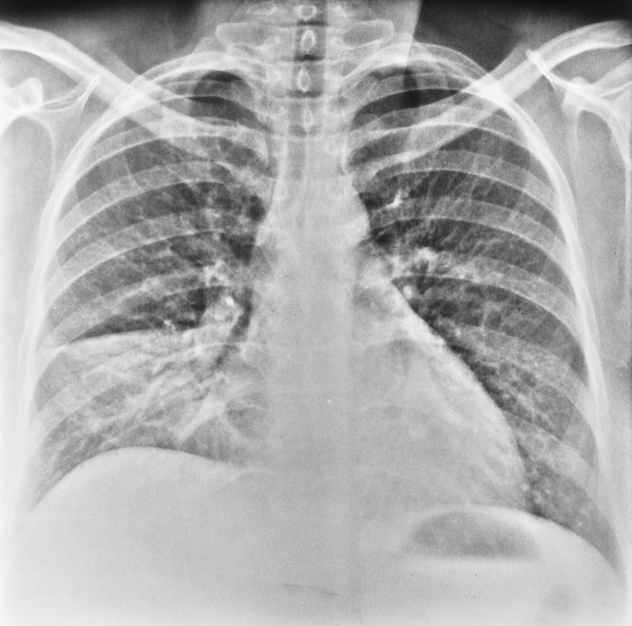
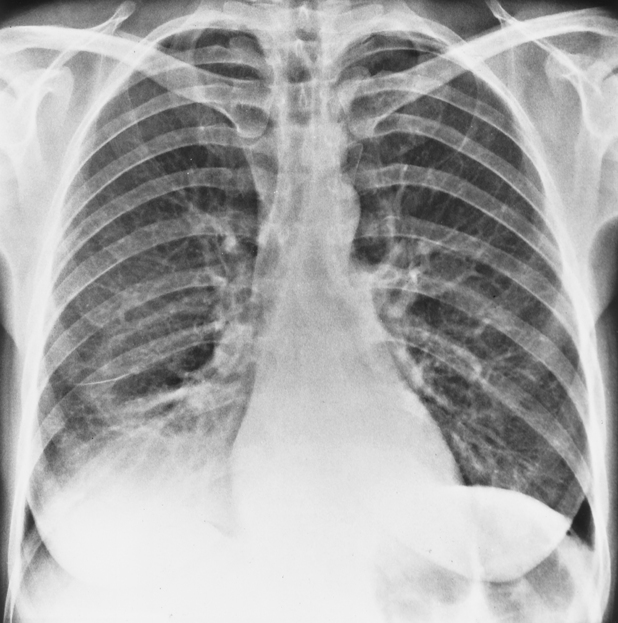
The chest radiograph should be evaluated to make sure that the patient was not rotated when the chest image was obtained. If the patient is rotated, uniform exposure of both lungs will not be obtained, and one side of the image will be darker than the other. The shadows of the heart and other mediastinal structures may also appear enlarged if the patient is rotated. Patient rotation is assessed by identifying the relationship of the spinous processes of the vertebral column to the medial ends of the clavicles (Fig. 10-3). The spinous processes should be centered between the ends of the clavicles and directly behind the tracheal air shadow. If the medial end of one clavicle appears closer to the spine, the patient probably was rotated.
Interpretation
Silhouette Sign
The silhouette sign is useful primarily in determining whether a pulmonary infiltrate is in anatomic contact with another thoracic structure. Normally, the significant difference in density between two adjoining structures will sharply delineate their borders. This allows a person viewing the chest radiograph to see the heart border, the aortic knob, and the diaphragm shadows on the background of radiolucent lung—a natural contrast between the thoracic tissues that makes the chest radiograph a great diagnostic tool (see comparison to thigh radiograph earlier in this chapter). If the lung tissue in contact with either heart border or sections of diaphragm becomes consolidated, the contrast in densities is lost, and the corresponding heart or diaphragm border is blurred (Fig. 10-4; see Fig. 10-3). This phenomenon is called the silhouette sign.