137 Chemical and Nuclear Agents
• Decontamination should take place immediately, before initial treatment and evacuation of exposed patients.
• For patients exposed to nerve agents, atropine and pralidoxime chloride should be administered rapidly.
• Treatment of blast injuries and emergency medical conditions should precede specific treatment of radiation exposure.
Epidemiology
Tens of thousands of chemicals are manufactured, transported, and used every day. The 1984 Bhopal, India, disaster revealed the dangers posed by chemical agents. A 2008 U.S. Department of Health and Human Services database of 14 states reported more than 15,000 chemical-related events and over 4500 casualties.1 Since World War I, chemical agents have also been used intentionally on civilian and military personnel, most recently in Japan in 1994-1995, in Russia in 2002, and in Iraq in 2007. Of the 13 categories of chemical agents recognized by the U.S. Centers for Disease Control and Prevention, the four principal categories are nerve, vesicant, blood, and pulmonary agents2 (Box 137.1).
Perspective
Casualties involving chemical and radiologic or nuclear agents have traditionally been associated with military armed conflicts. However, over the past 25 years, with the increased production and distribution of industrial chemicals, as well as the escalating threat of terrorist use of weapons of mass destruction, management of casualties from chemical, biologic, radiologic, nuclear, and high-yield explosive events has increasingly become the responsibility of the EP.3
Initially approved in 1999 and revised in 2006, the American College of Emergency Physicians (ACEP) issued a clinical policy statement that recognized the risk posed by accidental or intentional release of chemical and nuclear hazardous material (HAZMAT).4 In another clinical policy statement, the ACEP also encouraged EPs to assume a primary role in the medical aspects of planning, management, and patient care during disasters, including those involving chemical, radiologic, and nuclear agents.5
Basic Principles of Managing Contaminated Patients
Communication and Mobilization
Most events involving chemical or radioactive agents are rapidly identified by emergency services. Notification of health care facilities of a HAZMAT incident and casualties must also take place rapidly because 50% to 80% of the acute casualties will arrive at the closest health care facilities within 90 minutes following an event.6 Some casualties may leave the scene under their own power and go to a nearby health care facility, even before other patients arrive via emergency medical services.7,8
Decontamination
Decontamination should take place immediately, before initial treatment and evacuation of exposed patients. Although decontamination is usually completed at the scene before transportation, exposed and potentially contaminated patients may go on their own to nearby health care facilities.9 In addition to requiring primary decontamination and triage, these patients may secondarily contaminate existing patients and medical personnel and thus create additional casualties and diminish the response by the affected facility.7,9,10
Removal of contaminated clothing can eliminate 70% to 90% of HAZMAT.11,12 Once completed, patients should shower—or be showered if incapacitated—with copious amounts of tepid water. Several adjuncts, such as hypoallergenic liquid soap, may be helpful. Other adjuncts, including hard brushes and dilute additives such as bleach, are unlikely to provide additional benefit and, in some scenarios, could be harmful. Contaminated clothing and special items such as valuables and firearms should be labeled and securely contained to prevent accidental or continued secondary contamination, as well as for possible forensic analysis during a HAZMAT or criminal investigation.12–16
Security
Security personnel at health care facilities should be engaged promptly because their primary responsibility is to protect existing patients, staff, and the health care facility from contamination and distraction from avoidable crowds by controlling all access points to the facility. This responsibility may entail limiting visits from arriving friends, family, and other third parties, as well as sequestering contaminated patients.17
Security personnel should control traffic flow to and within the facility. Incoming patients should be directed to designated triage and decontamination sites, and the arrival of hospital personnel should be expedited. Patients awaiting further evaluation and disposition may be directed to secondary triage, holding, and treatment areas. Security personnel should coordinate with law enforcement and government agencies, safeguard valuables, and maintain the chain of custody of firearms and forensic evidence.9,10,17
Chemical Agents
Nerve Agents
Pathophysiology
Absorbed through inhalation and skin contact, nerve agents irreversibly bind and inactivate acetylcholinesterase (AChE) receptors, thereby leading to excessive accumulation of acetylcholine and overstimulation of nicotinic and muscarinic receptors. Though dose dependent, the effects from inhalation begin within seconds and peak within minutes, whereas the effects from skin exposure may take minutes to hours to become evident.18–20
Treatment
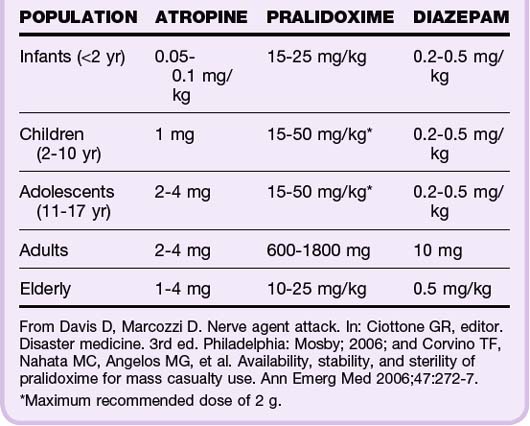
Atropine and pralidoxime chloride (2-PAM chloride) should be administered rapidly. When intubating patients, use of succinylcholine should be avoided. Atropine, a competitive cholinergic blocking agent, can mitigate muscarinic symptoms and should be administered every 5 to 10 minutes until airway resistance is minimized and respiratory secretions have dried. Pediatric patients may receive 0.05 to 0.1 mg/kg, with a maximum dose of 1 mg. Adults can receive 2-mg doses, with total doses of 2 g having been reported anecdotally.2-PAM chloride reactivates AChE. Pediatric patients may receive 15 mg/kg, whereas adults can receive 600-mg doses.With severe exposure, diazepam should be administered to reduce seizure activity and its sequelae20–23 (Table 137.1).
Vesicant Agents
Pathophysiology
Vesicating agents are highly penetrative oily substances that induce blister formation and include mustard agents and organic arsenicals. Mustard has a wide range of effects on the eyes, skin, lungs, nervous system, and bone marrow.20 It has been produced and stockpiled by multiple countries.24 Lewisite is an arsenical often combined with mustard, smells like geraniums, and is associated with renal failure and hepatic necrosis.
Presenting Signs and Symptoms
For mustard agents, the earliest symptoms are irritation and burning of exposed areas, such as the eyes and upper airway. Subsequent symptoms include pruritus and erythema of the skin, especially warm, moist locations such as the axillae and groin. With higher doses or prolonged exposure, shortness of breath, bulla formation, and corneal damage develop. Vomiting, diarrhea, bone marrow suppression, and seizures are associated with severe exposure and imply a poor prognosis.20,25,26
Treatment
Unless completed within minutes of exposure, decontamination will not prevent tissue and DNA damage. It can, however, reduce or prevent ongoing exposure and secondary contamination. Only lewisite has a specific antidote, the chelating agent British antilewisite (BAL). BAL can be toxic itself, may contain peanut oil, and thus should not be given to patients with peanut allergy.20,27
Blood Agents
Pathophysiology
Blood agents include cyanide and arsenic-based chemicals. Absorbed through inhalation, ingestion, and topical exposure, blood agents disrupt the mitochondrial cytochrome oxidase complex, thereby inhibiting intracellular oxygen use and aerobic metabolism. Cyanide is the most well-known blood agent and is often associated with a pungent odor described as bitter almond. Cyanide is widely used in many industries, such as mining and plastic manufacturing, and can be released during the combustion of numerous natural and synthetic material. It has also been identified as a likely agent for use by terrorists.20,28
Treatment
Treatment should be initiated immediately and presumptively based on prehospital information and clinical suspicion because diagnostic tests are not readily available. Traditionally, definitive treatment has been administration of the three components of the cyanide antidote kit: amyl nitrite, sodium nitrite, and sodium thiosulfate. Hydroxocobalamin, a precursor of vitamin B12, has gained acceptance as another antidote because it can be used for prehospital management and has better safety and side effect profiles.28–30
Pulmonary Agents
Pathophysiology
Pulmonary agents include phosgene and chlorine. Absorbed through inhalation and topical contact, pulmonary agents irritate and cause an inflammatory reaction of the peripheral and central airways. Phosgene is widely used in many industries, released during the combustion of foam plastics, and associated with the smell of newly cut grass. Chlorine is used widely in manufacturing and for purifying water and has its own distinctive odor. It was the first chemical warfare agent and has recently been involved in several large-scale disasters and terrorist attacks.20,31
Presenting Signs and Symptoms
Symptoms begin within minutes and may start with eye irritation, rhinorrhea, coughing, and dyspnea. With greater exposure, skin irritation, vomiting, and shortness of breath may be observed, and with severe exposure, blistering and pulmonary edema may develop.32
Treatment
Treatment is primarily supportive. Eye injuries should be managed with ophthalmologic antibiotics and follow-up. Skin injuries should be treated similar to thermal burns, including wound care, tetanus prophylaxis, and analgesia. Respiratory injuries may require oxygen, bronchodilators, and endotracheal intubation and ventilatory support. Corticosteroids are recommended, and nebulized lidocaine and sodium bicarbonate may be beneficial.31
Radiologic and Nuclear Agents
Pathophysiology
Irradiation and external contamination by a radiologic agent may occur as a result of the surreptitious placement of a radiation emission device or detonation of a dirty bomb.33,34 A dirty bomb involves the use of conventional explosives to disperse radioactive material, such as iodine 131. After decontamination, treatment of blast injuries should precede treatment of radiologic injuries because immediate death from the radiation is unlikely35,36 (Table 137.2). If free of particulate matter and shrapnel, patients are unlikely to pose a significant threat to other patients and medical personnel.
| TYPE | MECHANISM | EXAMPLES/EFFECTS |
|---|---|---|
| Primary | Direct pressurization | Rupture of tympanic membranes, lungs, viscera |
| Secondary | Projectiles | Penetrating trauma from fragments |
| Tertiary | Secondary trauma | Structural collapse, being thrown by the blast wind |
| Quaternary | Other | Burns, radiation, hazardous materials |
From DePalma RG, Burris DG, Champion HR, et al. Blast injuries. N Engl J Med 2005;352:1335–42; and U.S. Department of Health and Human Services radiation emergency medical management. Available at http://www.remm.nlm.gov/nuclearexplosion.htm.
Presenting Signs and Symptoms
Within a few hours of exposure to greater than 1 Gy, three acute radiation syndromes may develop. Hematopoietic syndrome results in pancytopenia and a predisposition to infection, bleeding, and poor wound healing. Gastrointestinal syndrome results in abdominal cramping, vomiting, and diarrhea. Early intractable vomiting and bloody diarrhea imply a poor prognosis. Cerebrovascular syndrome results in confusion, ataxia, and seizures.37
Treatment
After blast injuries and emergency medical conditions are treated, several radiation exposure–specific treatments should be discussed and initiated under the guidance of radiation safety, nuclear medicine, and hematology consultants. Any necessary surgeries should be performed within the first 24 to 36 hours before patients become immunologically incompetent. Cytokine therapy and the administration of chelating or blocking agents, such as potassium iodide and Prussian blue, should be considered.37
Disaster Medical Services Clinical and Practice Management Policy Statement. American College of Emergency Physicians. October 2006. Available at http://www.acep.org/content.aspx?id=29176
Koenig KL, Boatright CJ, Hancock JA, et al. Health care facility–based decontamination of victims exposed to chemical, biological, and radiological materials. Am J Emerg Med. 2008;26:71–80.
Lawrence DG, Kirk MA. Chemical terrorism attacks: update on antidotes. Emerg Med Clin North Am. 2007;25:567–595.
Wolbarst AB, Wiley AL, Jr., Nemhauser JB, et al. Medical response to a major radiologic emergency: a primer for medical and public health practitioners. Radiology. 2010;254:660–677.
1 U.S. Department of Health and Human Services. Agency for Toxic Substances & Disease Registry biennial report 2007-2008. Available at http://www.atsdr.cdc.gov/hs/hsees/annual2008.html
2 U.S. Centers for Disease Control and Prevention. Emergency preparedness and response chemical categories. Available at http://www.bt.cdc.gov/agent/agentlistchem-category.asp
3 Waeckerle JF, Seamans S, Whiteside M, et al. Executive summary: developing objectives, content, and competencies for the training of emergency medical technicians, emergency physicians, and emergency nurses to care for casualties resulting from nuclear, biological, or chemical (NBC) incidents. Ann Emerg Med. 2001;37:587–601.
4 Handling of Hazardous Materials Clinical and Practice Management Policy Statement. American College of Emergency Physicians. October 2006. Available at http://www.acep.org/content.aspx?id=29496
5 Disaster Medical Services Clinical and Practice Management Policy Statement. American College of Emergency Physicians. October 2006. Available at http://www.acep.org/content.aspx?id=29176
6 U.S. Centers for Disease Control and Prevention. Emergency preparedness and response mass casualties predictor. Available at http://www.bt.cdc.gov/masscasualties/predictor.asp
7 Okumura T, Takasu N, Ishimatsu S, et al. Report on 640 victims of the Tokyo subway sarin attack. Ann Emerg Med. 1996;28:129–135.
8 Gutierrez de Ceballos JP, Turegano-Fuentes F, Perez-Diaz D, et al. 11 March 2004: the terrorist bomb explosions in Madrid, Spain—an analysis of the logistics, injuries sustained, and clinical management of casualties treated at the closest hospital. Crit Care. 2005;9:104–111.
9 Macintyre AG, Christopher GW, Eitzen E, Jr., et al. Weapons of mass destruction events with contaminated casualties: effective planning for health care facilities. JAMA. 2000;283:242–249.
10 Koenig KL, Boatright CJ, Hancock JA, et al. Health care facility–based decontamination of victims exposed to chemical, biological, and radiological materials. Am J Emerg Med. 2008;26:71–80.
11 Kales SN, Christiani DC. Acute chemical emergencies. N Engl J Med. 2004;350:800–808.
12 Koenig KL. Strip and shower: the duck and cover for the 21st century. Ann Emerg Med. 2003;42:391–394.
13 Best practices and guidelines for mass personnel decontamination. 1st ed. Maryland: Aberdeen Proving Grounds, Chemical and Biological Defense Information Analysis Center; 2003.
14 Marcozzi D. Introduction to chemical disasters. Ciottone GR, ed. Disaster medicine, 3rd ed, Philadelphia: Mosby, 2006.
15 Moffett PM, Baker BL, Kang CS, et al. Evaluation of time required for water-only decontamination of an oil-based agent. Mil Med. 2010;175:185–187.
16 Feldman RJ. Chemical agent stimulant release from clothing following vapour exposure. Acad Emerg Med. 2010;17:221–224.
17 Schultz CH, Mothershead JL, Field M. Bioterrorism preparedness I: the emergency department and hospital. Emerg Med Clin North Am. 2002;20:437–455.
18 Sidell FR, Borak J. Chemical warfare agents: II. Nerve agents. Ann Emerg Med. 1992;21:865–871.
19 Lee EC. Clinical manifestations of sarin nerve gas exposure. JAMA. 2003;290:659–662.
20 U.S. Army Medical Research Institute of Chemical Defense Chemical Casualty Care Division. Medical management of chemical casualties handbook, 4th ed. Maryland: Aberdeen Proving Grounds; 2007.
21 Leikin JB, Thomas RG, Walter FG, et al. A review of nerve agent exposure for the critical care physician. Crit Care Med. 2002;30:2346–2354.
22 Corvino TF, Nahata MC, Angelos MG, et al. Availability, stability, and sterility of pralidoxime for mass casualty use. Ann Emerg Med. 2006;47:272–277.
23 Lawrence DG, Kirk MA. Chemical terrorism attacks: update on antidotes. Emerg Med Clin North Am. 2007;25:567–595.
24 Central Intelligence Agency Unclassified Semi-Annual Report to Congress on the acquisition of technology to weapons of mass destruction and advanced conventional weapons. 1 January-30 June 2001. Washington, DC: Government Printing Office; 2001.
25 Borak J, Sidell FR. Agents of chemical warfare: sulfur mustard. Ann Emerg Med. 1992;21:303–308.
26 Goffman TE. Toxic chemical effects that might present in the ED. Am J Emerg Med. 2009;27:1149–1154.
27 Kulchycki LK. Vesicant agent attack. Ciottone GR, ed. Disaster medicine, 3rd ed, Philadelphia: Mosby, 2006.
28 Eckstein M. Enhancing public health preparedness for a terrorist attack involving cyanide. J Emerg Med. 2007;35:59–65.
29 Borron SW, Baud FJ, Barriot P, et al. Prospective study of hydroxocobalamin for acute cyanide poisoning in smoke inhalation. Ann Emerg Med. 2007;49:794–801. e1–e2
30 Shepherd G, Velez LI. Role of hydroxocobalamin in acute cyanide poisoning. Ann Pharmacother. 2008;42:661–669.
31 Jones R, Wills BK, Kang CS. Chlorine gas: an evolving hazardous material threat and unconventional weapon. West J Emerg Med. 2010;11:151–156.
32 Van Sickle D, Wenck MA, Belflower A, et al. Acute health effects after exposure to chlorine gas released after a train derailment. Am J Emerg Med. 2009;27:1–7.
33 Coleman CN, Hrdina C, Bader JL, et al. Medical response to a radiologic/nuclear event: integrated plan from the Office of the Assistant Secretary for Preparedness and Response. Ann Emerg Med. 2009;53:213–222.
34 Wolbarst AB, Wiley AL, Jr., Nemhauser JB, et al. Medical response to a major radiologic emergency: a primer for medical and public health practitioners. Radiology. 2010;254:660–677.
35 Wightman JM, Gladish SL. Explosions and blast injuries. Ann Emerg Med. 2001;37:664–678.
36 DePalma RG, Burris DG, Champion HR, et al. Blast injuries. N Engl J Med. 2005;352:1335–1342.
37 Waselenko JK, MacVittie TJ, Blakely WF, et al. Medical management of the acute radiation syndrome: recommendations of the Strategic National Stockpile Radiation Working Group. Ann Intern Med. 2004;140:1037–1051.