FIGURE 8.1 Practical approach to sensitive skin.
TABLE 8.1
Overview of Testing Methods for Sensitive Skin
|
Sensory Reactivity Tests |
Irritant Reactivity Tests |
Dermal Function Tests |
|
|
Goal |
To evaluate cutaneous neurosensory response to the application of different chemical substances, or physical stimuli |
To assess objective signs of skin irritation after the application of SLS or other known irritants |
To measure structural or physiological cutaneous changes after the application of topical irritants |
|
Tests |
• Self-assessment questionnaires • Stinging test: 10% lactic acid (or capsaicin, ethanol, menthol, benzoic acid) • Thermal sensation test (QST) • Evaluation of itching response • Washing and exaggerated immersion test |
Assessment of cutaneous irritation by the following: • Colorimetry (visual erythema) • Laser Doppler velocimetry (nicotinate test) • Electrical capacitance • Corneometry (skin hydration) • Reflectance |
Parameters evaluated: • TEWL (basal or dynamic desorption curves) • Cutaneous pH • Epidermal thickness (measured by US, OM, or CM) • Skin penetrability (measured by UV light) |
|
Advantages Disadvantages |
Fast and easy to perform Subjective, intraindividual variability, and lack of predictive value |
Objective and noninvasive Indirect measurement and specialized complex tools |
Quantitative and accurate Time consuming, specialized, and expensive |
Source: Primavera, G., and Beradesca, E., Int J Cosmet Sci, 27, 1–10, 2005; Piel, 28, Rodrigues-Barata, R., and Conde Salazar-Gómez, L., Sensitive skin, 520–530, Copyright (2013), with permission from Elsevier; Escalas-Taberner, J., González-Guerra, E., and Guerra-Tapia, A., Actas Dermosifiliogr, 102, 563–571, 2011.
Note: CM: confocal microscopy; OM: optical microscopy; QST: quantitative sensory test; US: ultrasonography.
Testing Methods
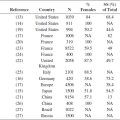
To evaluate and quantify the severity of sensitive skin objectively, reproducible and noninvasive tests are absolutely necessary. According to Farage et al. (22,23), testing methods can be divided into three main groups depending on the biophysical factor assessed: those that investigate neurosensory response (sensory reactivity tests), those that evaluate visible cutaneous signs of irritation (irritant reactivity tests), and those that measure structural and physiological parameters of the skin as a consequence of the irritant effect (dermal function tests) (24). Table 8.1 represents an overview of the currently available testing methods.
Sensory Reactivity Tests
Because almost half of patients with sensitive skin report uncomfortable symptoms without accompanying visible signs of inflammation, new tools of sensory testing have been increasingly utilized to provide definite information (13).
These methods evaluate cutaneous neurosensory response to the application of different chemical substances or other physical stimuli (7). Of them, the stinging test of Frosch and Kligman (25), which consists of the application of 0.5 mL of 10% lactic acid to the nasolabial fold with subsequent assessment of the severity of the subjective symptoms, has traditionally been considered to be the most suitable, fast, and easy to perform (26). However, nasolabial stinging seems to be a poor predictor of general skin sensitivity (27). Marriott et al. (27) tested four chemicals commonly used to induce different sensory effects (lactic acid, stinging; capsaicin, burning; menthol, cooling; and ethanol, a mixture of burning and stinging), reporting a high number of variations in reactivity to the tested substances and a lack of predictive value of increased reactivity among the different materials (27). In addition, an important intraindividual variability has been demonstrated comparing the responses to only two chemicals (28).
Irritant Reactivity Tests
Irritant reactivity tests measure objective signs of skin irritation after the application of a known irritant substance (13). They are based on the topical application of sodium lauryl sulfate (SLS), or other chemicals, followed by the assessment of cutaneous irritation through several procedures, such as colorimetry (visual erythema after the application of varying concentrations of methyl nicotinate or SLS to the forearm), laser Doppler velocimetry (vasodilatory effect following nicotinate test), electrical capacitance or corneometry (skin hydration), and reflectance (14).
These methods are suitable noninvasive tools to objectively quantify sensitive skin but may occasionally require robust specialized appliances.
Dermal Function Tests
These types of tests relies on the measurement of structural or physiological cutaneous changes after the application of topical irritants, such as SLS or others. TEWL, cutaneous pH, and epidermal thickness, measured by ultrasonography, optical microscopy, or confocal microscopy, as well as skin penetrability, assessed with UV light, are the parameters most commonly used (13,14,24).
Although dermal function tests are highly accurate quantitative methods, their use is mainly limited to the investigation field, as they are especially very time consuming and require expensive and specialized tools to be carried out in daily clinical practice (14,29,30).
TEWL assessment is the most frequent procedure performed to evaluate and quantify the function of stratum corneum (24). The basal evaluation of TEWL is able to measure preclinical disease without altering the underlying skin condition by a noninvasive estimation of water pressure gradient above the skin surface (13,24). Some studies have proposed a combined assessment of desorption curves of TEWL and plastic occlusion test to quantify the severity of sensitive skin objectively. Most investigators already prefer this new approach, as changes on skin barrier can be dynamically assessed (26,31).
Contact Tests
To conclude the diagnosing process of sensitive skin properly, Pons-Guiraud (12) recommends performing patch tests in order to find out any sources of allergic contact dermatitis and advise the patient accordingly. In addition to standard series, these patients should be tested with their own products of daily use and specific batteries that include the most common allergens present in cosmetic and personal care products (24,26). Likewise, open and repeated application tests must be performed before making a final diagnosis (32). When photoallergic contact dermatitis or contact urticaria is suspected, workup should include photopatch and hypersensitivity test type 1, respectively (14).
Other Evaluations
Finally, if the whole complementary exams do not reveal any underlying signs suggestive of sensitive skin, the patient should be referred to mental health care providers (14,24).
Conclusion
The high prevalence and complex physiopathological origin of sensitive skin represent a challenge for dermatologists who face an increasing demand for the management of this condition. Because the manifestations of skin sensitivity are mainly subjective and transient, symptoms self-reported by the patients through self-assessment questionnaires, along with an accurate clinical evaluation, remain the best methods of diagnosis. Developing standardized and reproducible testing methods that let physicians objectively quantify the severity of the disease to advise and treat patients properly remains a real need not yet covered.
REFERENCES
1. Kligman AM, Sadiq I, Zhen Y, Crosby M. Experimental studies on the nature of sensitive skin. Skin Res Technol 2006; 12: 217–222.
2. Slodownik D, Williams J, Lee A, Tate B et al. Controversies regarding the sensitive skin syndrome. Expert Rev Dermatol 2007; 2: 579–584.
3. Kamide R, Misery L, Perez-Cullell N, Sibaud V et al. Sensitive skin evaluation in the Japanese population. J Dermatol 2013; 40: 177–181.
4. Misery L, Myon E, Martin N, Consoli S et al. Sensitive skin: Psychological effects and seasonal changes. J Eur Acad Dermatol Venereol 2007; 21: 620–628.
5. Farage MA, Katsarou A, Maibach HI. Sensory, clinical and physiological factors in sensitive skin: A review. Contact Derm 2006; 55: 1–14.
6. Misery L. How the skin reacts to environmental factors. J Eur Acad Dermatol Venereol 2007; 21: 5–8.
7. Berardesca E, Farage M, Maibach H. Sensitive skin: An overview. Int J Cosmet Sci 2013; 35: 2–8.
8. Simion FA, Rau AH. Sensitive skin. Cosmet Toilet 1994; 109: 43–50.
9. Richters R, Falcone D, Uzunbajakava N, Verkruysse W et al. What is sensitive skin? A systematic literature review of objective measurements. Skin Pharmacol Physiol 2015; 28: 75–83.
10. Diogo L, Papoila AL. Is it possible to characterize objectively sensitive skin? Skin Res Technol 2010; 16: 30–37.
11. Misery L, Sibaud V, Merial-Kieny C, Taïeb C. Sensitive skin in the American population: Prevalence, clinical data, and role of the dermatologist. Int J Dermatol 2011; 50: 961–967.
12. Pons-Guiraud A. Sensitive skin: A complex and multifactorial syndrome. J Cosmet Dermatol 2004; 3: 145–148.
13. Primavera G, Beradesca E. Sensitive skin: Mechanisms and diagnosis. Int J Cosmet Sci 2005; 27: 1–10.
14. Rodrigues-Barata R, Conde Salazar-Gómez L. Sensitive skin. Piel 2013; 28: 520–530.
15. Willis CM, Shaw S, De Lacharrière O, Baverel M et al. Sensitive skin: An epidemiological study. Br J Dermatol 2001; 145: 258–261.
16. Simion FA, Rhein LD, Morrison BM Jr, Scala DD et al. Self-perceived sensory responses to soaps and synthetic detergent bars correlate with clinical signs of irritation. J Am Acad Dermatol 1995; 32: 205–207.
17. Gougerot A, Vigan M, Bourrain SL. Le SIGL: Un outil d’évaluation clinique des peaux réactives? Nouv Dermatol 2007; 26: 13–15.
18. Querleux B, Dauchot K, Jourdain R, Bastien P et al. Neural basis of sensitive skin: An fMRI study. Skin Res Technol 2008; 14: 454–461.
19. Misery L, Sibaud V, Ambronati M, Macy G et al. Sensitive scalp: Does this condition exist? An epidemiological study. Contact Dermatitis 2008; 58: 234–238.
20. Saint-Martory C, Roguedas-Contios AM, Sibaud V, Degouy A et al. Sensitive skin is not limited to the face. Br J Dermatol 2008; 158: 130–133.
21. Misery L, Rahhali N, Ambonati M, Black D et al. Evaluation of sensitive scalp severity and symptomatology by using a new score. J Eur Acad Dermatol Venereol 2011; 25: 1295–1298.
22. Farage MA, Katsarou A, Maibach HI. Sensory, clinical and physiological factors in sensitive skin: A review. Contact Dermatitis 2006; 55: 1–14.
23. Farage MA, Maibach HI. Sensitive skin syndrome: Methodological approaches. Cosmet Toil 2008; 123: 28–33.
24. Inamadar A, Palit A. Sensitive skin: An overview. Indian J Dermatol Venereol Leprol 2013; 79: 9–16.
25. Frosch PJ, Kligman AM. A method of appraising the stinging capacity of topically applied substances. J Soc Cosmet Chem 1977; 28: 197–209.
26. Escalas-Taberner J, González-Guerra E, Guerra-Tapia A. Sensitive skin: A complex syndrome. Actas Dermosifiliogr 2011; 102: 563–571.
27. Marriott M, Holmes J, Peters L, Cooper K et al. The complex problem of sensitive skin. Contact Derm 2005; 53: 93–99.
28. Green BG, Shaffer GS. Psychophysical assessment of the chemical irritability of human skin. J Soc Cosmet Chem 1992; 43: 131–147.
29. Farage MA, Maibach HI. Sensitive skin: Closing in on a physiological cause. Contact Dermatitis 2010; 62: 137–149.
30. Farage M, Robinson M. Sensitive skin: Intrinsic and extrinsic contributors. In: Lode´n M, Maibach HI, editors. Treatment of Dry Skin Syndrome. Berlin–Heidelberg: Springer-Verlag 2012; 95–109.
31. Pinto P, Rosado C, Parreirão C, Rodrigues LM. Is there any barrier impairment in sensitive skin?: A quantitative analysis of sensitive skin by mathematical modeling of transepidermal water loss desorption curves. Skin Res Technol 2011; 17: 181–185.
32. Lev-Tov H, Maibach H. The sensitive skin syndrome. Indian J Dermatol 2012; 57: 419–423.