CHAPTER 69 CERVICAL, THORACIC, AND LUMBAR FRACTURES
Spinal column injuries in the United States occur at a rate of 4 to 5.3 injuries per 100,000 households. The most common causes of spinal column injuries include motor vehicle accidents (45%), falls (20%), sports-related accidents (15%), violence (15%), and miscellaneous causes (5%).
NEUROLOGIC INJURY
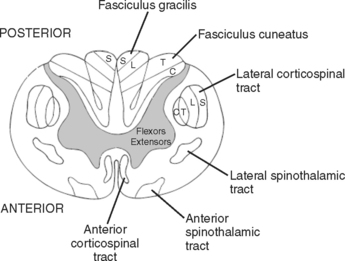
The end of the spinal cord (conus medullaris) is located at L1-L2 intervertebral disk. Below the level of the conus medullaris, the spinal canal is occupied by the lower motor roots called the cauda equina. As a lower motor neuron lesion, injury to the nerve roots has a much better prognosis for recovery than injury to the spinal cord (Figure 1).
Classification of Neurologic Injury
The secondary survey in patients with spinal cord injury includes a precise definition of neurologic deficits. Classification systems are useful to compare outcomes between different studies. While a variety of clinical grading systems exist, the American Spinal Injury Association (ASIA) scale has become the most widely accepted. The ASIA scale identifies motor, sensory, and general impairment deficits, and incorporates the functional independence measure (see page 163).
Incomplete Spinal Cord Syndromes
Four incomplete spinal cord syndromes are defined based on the location of the trauma to the spinal cord. Central cord syndrome is the most common pattern of injury, resulting from gray matter destruction, which is worst in the central region of the spinal cord. This injury pattern often occurs due to hyperextension injury in a patient with degenerative cervical spinal stenosis. The patient experiences motor and sensory deficits that are worse in the upper than in the lower extremities. The overall prognosis for central spinal cord injuries is good, with 75% of the patients experiencing at least partial motor recovery and most regaining the ability to ambulate.
Posterior cord syndrome is the rarest and causes decreased position and pressure sensation.
CERVICAL SPINE TRAUMA
Anatomy
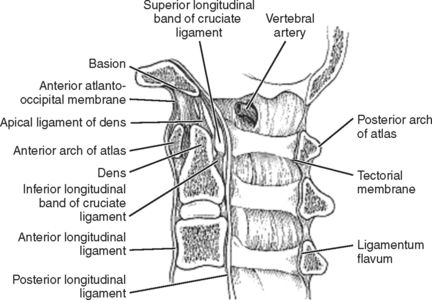
Spinal stability primarily stems from ligament and disk integrity. Craniocervical stability involves intact anterior and posterior atlanto-occipital membranes and articular capsules. The atlantoaxial joint is stabilized by the transverse ligament primarily with the paired alar and apical ligaments provided secondary stabilization. The posterior ligamentum nuchae, interspinous ligaments, and ligamentum flavum acts as a “tension band” to provide resistance against flexion distraction injuries. The atlantoaxial joint provides 50% of the overall cervical rotation (Figure 2).
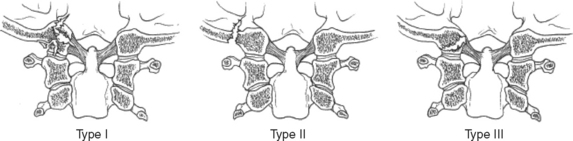
Occipital Condyle Fracture
Stable type I, II, and III fractures can be managed in a cervical collar for 6–8 weeks. Displaced type II or III fractures are managed in a halo vest for 8–12 weeks. Grossly unstable type III fractures require occiput to C2 fusion and should raise the suspicion for an underlying occipitocervical dissociation. Cranial nerve palsies may develop days to weeks after the injury and most frequently involve cranial nerves IX, X, and XI (Figure 3).
Atlas Fractures
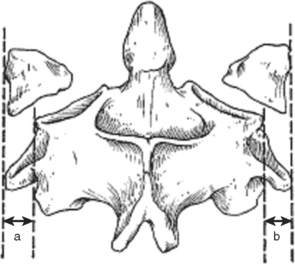
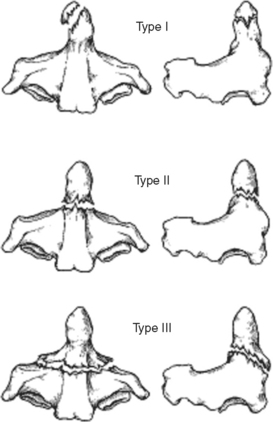
Atlas fractures comprise 7% of the cervical spine fractures. Fractures can involve the anterior or posterior arch, lateral masses, and transverse processes. Jefferson or burst fractures are bilateral, involving both the anterior and posterior arches resulting from axial load (Figure 4). Atlantoaxial stability depends on the integrity of the transverse ligament. Combined lateral mass displacement greater than 7 mm on AP radiographs (Figure 5).

Figure 4 Types of C1 arch fractures.
(From Hasharoni A, Errico TJ: Fracture of the first cervical vertebra. In Clark CR, Dvorak J, Ducker TB, et al., editors: The Cervical Spine, 4th ed. Philadelphia, Lippincott-Raven, 2005, p. 610.)
Dens Fractures
Dens fractures have been classified by Anderson and D’Alonzo (Table 1; Figure 6). Type I and III fractures can generally be treated with an external orthosis. Management of type II fractures is more problematic and depends on patient age and associated injuries, as well as fracture displacement and stability. While nondisplaced fractures can sometimes be treated successfully with a halo vest, indications to operate include fracture comminution, displacement greater than 6 mm, posterior angulation, delay in diagnosis, and patient age greater than 50 years old. In general, elderly patients can be considered for C1-C2 fusion because of their decreased healing rates and poor tolerance of halo vest. Severely debilitated patients, on the other hand, can be treated with a cervical collar until comfortable, with the understanding that a successful fusion may not occur.
| Type I | Avulsion fractures of tip |
| Type II | Waist fractures |
| Type III | Fracture extends into C2 body |
Source: Anderson LD, D’Alonzo RT: Fractures of the odontoid process of the axis. J Bone Joint Surg 56:1663–1674, 1974.
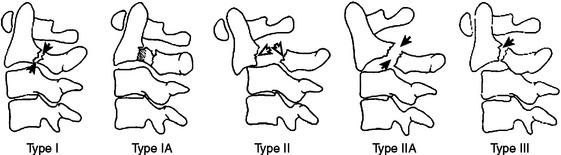
Traumatic Spondylolisthesis of Axis
Bilateral fractures of the par interarticularis are called hangman’s fractures. Most injuries are caused by motor vehicle accidents. Hangman’s fractures are classified by Levine and Edwards (Table 2; Figure 7). Type I fractures require 6–12 weeks of halo vest immobilization. Surgical options for type II and III fractures include reduction followed by anterior C2-C3 interbody fusion, posterior C1-C3 fusion, or bilateral C2 pars screw osteosynthesis.
| Type I | Fractures with <3 mm of displacement and no angulation due to axial compression and hyperextension |
| Type IA | Asymmetric fracture line with minimal angulation or displacement due to hyperextension with lateral bending forces |
| Type II | Fractures with >3 mm of translation and angulation due to hyperextension and axial loading followed by rebound flexion |
| Type IIA | Fractures demonstrate angulation without translation due to a flexion-distraction injury |
| Type III | Fractures include C2-C3 facet dislocation due to hyperextension followed by flexion mechanism |
Source: Levine AM, Edwards CC: The management of traumatic spondylo-listhesis of the axis. J Bone Joint Surg 67:221–226, 1985.
Subaxial Spine Fractures
Subaxial cervical spine fractures can be subclassified many ways. The most common injuries include compression, burst, and teardrop injuries.
THORACIC AND LUMBAR SPINE TRAUMA
Fractures
Denis’s three-column concept is frequently used because it includes the injury patterns most commonly seen and relates them to a specific mechanism of injury. The classification includes both minor and major injuries. Minor injuries include isolated fractures to the articular process, transverse process, and pars interarticularis. Major fracture types include compression, burst, flexion distraction, and fracture dislocations (Figure 8).
Compression Fractures
A compression fracture results from an axial load involves the anterior column of the spine. Radiographs show a wedge shaped defect in the vertebral body with varying degrees of kyphosis. Patients who are neurologically intact with less than 30 degrees of kyphosis and less than 50% vertebral body height loss can be managed in a hyperextension orthosis. Patients who do not meet these criteria need to be watched carefully for possible failure of the posterior ligamentous structures. Patients with fractures above T6 should wear a cervical extension for better spinal control (Figure 9).
Burst Fractures
Burst fractures also occur from axial loads but involve the anterior and middle columns. Involvement of the posterior column equates to overall instability. Radiographically, burst fractures demonstrate widening of the pedicles and varying degrees of retropulsion into the canal. Patients without neurologic deficits, kyphosis less than 30 degrees, and less than 50% vertebral body height loss can be managed with a thoracolumbar orthosis for 3 months. Patients who do not meet these criteria should undergo a posterior instrumented fusion procedure (Figure 10).
Flexion Distraction
Flexion distraction injuries occur when the flexion moment occurs anterior to the vertebral column. This injury typically occurs in motor vehicle accidents where the lap belt acts as a fulcrum, and the anterior column fails in compression, whereas the middle and posterior columns fail in tension. Purely ligamentous injuries have a poor propensity to heal and usually require short-segment posterior procedures. Pure bony injuries have the potential to heal without surgical intervention as long as a nonunion or deformity does not occur (Figure 11).
Thoracolumbar Junction and Lumbar Spine Fractures
The thoracic spinal cord has poor vascularity as well as a constant medullary artery (artery of Adamkiewicz). This medullary artery originates from the intercostal artery on the left side between T10 and T12, and has an anastamoses with the anterior spinal artery. Injury to the artery of Adamkiewicz via trauma or iatrogenic can lead to frank paralysis.
Allen BL, Ferguson RL, Lehman TR, et al. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7:1-27.
An HS, Simpson JM, Ebranheim NA, et al. Low lumbar burst fractures. Orthopedics. 1992;15:367-373.
Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. JBGS. 1974;56:1663-1674.
Anderson PA, Montesano PX. Orthology and treatment of occipital condyle fractures. Spine. 1988;13:731-736.
Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg [Am]. 1979;61:1119-1142.
Bracken MB, Sheppard MJ, Collins WF, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal cord injury: results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990;322:1405-1411.
Chapman JR, Anderson PA. Thoracolumbar spine fractures with neurologic deficit. Orthop Clin North Am. 1994;25:595-612.
Delamarter RB, Sherman JE, Carr JB. Cauda equine syndrome: neurologic recovery following immediate, early, or late decompression. Spine. 1991;16:1022-1029.
Denis F. Instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop. 1984;189:65-76.
Hoffman JR, Mower WR, Wolfson AB, et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. N Engl J Med. 2000;343:94-99.
Hurlbert RJ: The role of steroids in acute spinal cord injury: an evidence-based analysis. Spine 26(Suppl 24):S39-S46.
Joint Section on Disorders of the Spine and Peripheral Nerves, American Association of Neurological Surgeons/Congress of Neurological Surgeons. management of vertebral artery injuries after nonpenetrating cervical trauma. Guidelines for management of acute cervical spinal injuries. Neurosurgery. 2002;50(3):S1-179.
Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. JBGS. 1985;67:217-226.
Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201.
Peris MD, Donaldson WF, Towers J, et al. Helmet and shoulder pad removal in suspected cervical spine injury. Spine. 2002;27:995-999.
Nesathurai S. Steroids and spinal cord injury: revisiting the NASCIS II and NASCIS III trials. J Trauma. 1998;45:1088-1093.
White AA, Panjabi MM. Clinical Biomechanics of the Spine, 2nd ed. Philadelphia: JB Lippincott, 1990.
Wood K, Butterman G, Mehbod A, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. J Bone Joint Surg [Am]. 2003;85:773-781.
Yue J, Sossan A, Selgrath C, et al: The treatment of unstable thoracic spine fractures with transpedicular screw instrumentation: a 3 year consecutive series. Spine 27:2782–2787.