CHAPTER 220 Cervical Spine Disorders in Children
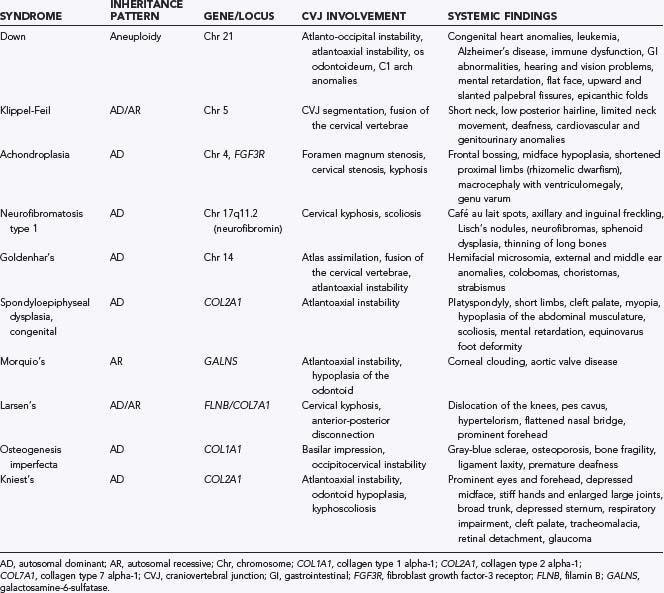
The true prevalence of congenital abnormalities of the cervical spine is unknown, although the incidence is probably underrepresented because many are asymptomatic. Some authors have reported that congenital anomalies of the cervical spine in children with Klippel-Feil syndrome (KFS), a relatively common congenital spine disorder, occur in 1 in 40,000 to 42,000 births.1–3 Population-based studies to estimate the incidence and prevalence of congenital cervical spine abnormalities are not available. Although some developmental abnormalities are isolated sporadic cases, many are found as part of a multisystem or syndromic anomaly (Table 220-1).4
Working knowledge of the anatomy and embryology of the pediatric cervical spine is crucial to properly identify congenital abnormalities, differentiate congenital from traumatic lesions, and approach the region at surgery. We refer the reader to several publications that describe pediatric cervical spine anatomy and embryology in detail.5–26
Specific Conditions
Down Syndrome
Down syndrome (trisomy 21) is the most common inherited chromosomal disorder, with an estimated prevalence of 1 in 700 live births. Occipitoatlantal subluxation and atlantoaxial subluxation are the two most common cervical spine problems seen in patients with Down syndrome. Patients with symptomatic atlantoaxial or occipitocervical instability may suffer from neck pain, torticollis, myeloradiculopathy, spasticity, hyperreflexia, or clonus.27,28
Occipitocervical instability is present to some degree in 40% to 50% of children with Down syndrome. To date, no studies have looked at the natural history of this problem. The normal occipitoatlantal joint is composed of reniform-shaped occipital condyles seated on cup-shaped articular facets supported by the capsular ligaments.29 Analysis of the occipitocervical junction in children with Down syndrome demonstrated that the superior articular surface of C1 and the occipital condyle are flattened in these patients.30 Surgical treatment is generally recommended in patients who have more than 10 mm of subluxation at the occipitoatlantal joint, although that decision must be made on an individual basis because of the low incidence of spinal cord injury in otherwise asymptomatic patients.29–31
Atlantoaxial subluxation is related to either the excessive ligamentous laxity or the osseous abnormalities in patients with Down syndrome. Radiographic atlantoaxial instability, as determined by the atlantodental interval and measurements of spinal canal diameter, is present in 10% to 30% of patients with Down syndrome,29,32–35 although only 1% of such patients have symptomatic C1-2 instability.27,28 One study of pediatric patients with Down syndrome and symptomatic atlantoaxial instability found that more than 80% of patients had os odontoideum.28
Suggestions have been made to screen children with Down syndrome for instability (Fig. 220-1).29,34,36 Cervical radiographs, including flexion and extension views, should be performed initially at 3 years of age to assess for excessive motion. If radiographs are normal, they may be repeated every 5 years or at the time of consideration for participation in the Special Olympics.29,34,36 For patients with abnormal results on screening studies (occipitocervical subluxation >10 mm, atlantodental interval >4.5 mm, or neural canal <12 mm), careful yearly follow-up is indicated. Surgical correction may be required if neurological signs and symptoms are present, if magnetic resonance imaging (MRI) shows spinal cord injury, if subluxation is progressive over time, or if an os odontoideum is present.29
Klippel-Feil Syndrome
First described in 1912,37 the now-classic triad of a short neck, low hairline, and limited neck mobility is known as Klippel-Feil syndrome, although less than 50% of patients with congenital fusion of the cervical spine have all three signs. Patients without all three signs are considered to have Klippel-Feil variant.1
The most common clinical finding in patients with KFS is a limited range of neck motion, particularly with lateral bending. Patients with extensive neck fusion and fusion of the craniovertebral junction are seen at an earlier age than those with subaxial fusion.4 Patients with C1-2 fusion are often first evaluated for pain in childhood, whereas those with lower cervical fusion are seen in the second or third decade of life or later when symptomatic junctional degeneration develops. Torticollis or neck webbing is present in just 20% of patients with KFS and is not specific to any particular cervical spine anomaly.38,39 Neurological abnormalities seen in patients with KFS include brainstem dysfunction, myeloradiculopathy, and headaches.
Among several classification schemes for KFS developed over the years,39–41 the most recent, presented by Tracy and colleagues, separates KFS into four classes and incorporates the mode of inheritance (Table 220-2).40
| TYPE | INHERITANCE PATTERN | CHARACTERISTICS |
|---|---|---|
| KF1 | Autosomal recessive | Fusion at C1, with or without caudal fusion; associated with other anomalies |
| KF2 | Autosomal dominant | 100% penetrance of C2-3 fusion |
| KF3 | Autosomal dominant or recessive | Congenital fusions caudal to C2-3 |
| KF4 (Wildervanck’s syndrome) | X-linked dominantly inherited pattern; hemizygous lethal | Congenital cervical fusion, hearing loss, Duane’s anomaly (congenital disorder of eye movement) |
Achondroplasia
Achondroplasia, the most common form of dwarfism, is characterized by disproportionate shortening of the proximal ends of limbs relative to the trunk. It occurs in 1 in 26,000 to 28,000 births, with an estimated incidence of 0.03% to 0.05% of all live births.42–44 It is inherited in autosomal dominant fashion, with 80% of cases attributed to spontaneous point mutations in the fibroblast growth factor receptor 3 gene located on chromosome 4.42,44 The cause of achondroplasia is a decrease in the rate of endochondral bone formation with normal formation of membranous bone.
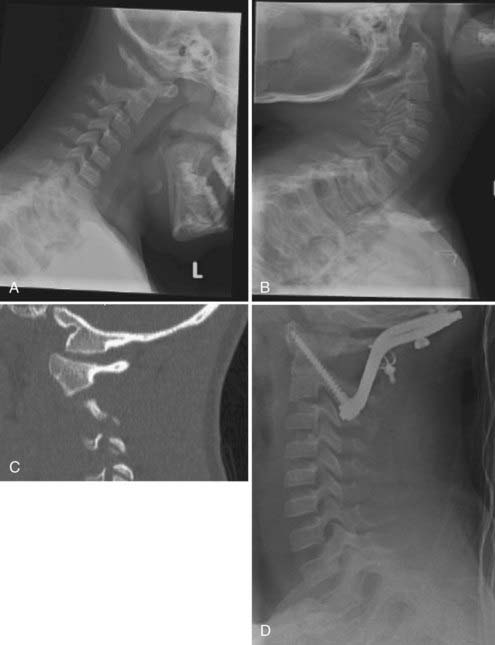
The predominant spinal condition in achondroplasia is compression, which can occur at the foramen magnum, subaxial cervical spine, or thoracolumbar spine (Fig. 220-2). The clinical features of patients with cervicomedullary compression secondary to stenosis of the foramen magnum include bulbar findings, myeloradiculopathy, hydrocephalus, and respiratory disorders. Symptoms of cervicomedullary compression in infants include excessive hypotonia, poor head control, feeding or sleep abnormalities, and apnea. The respiratory disturbances may have a multifactorial cause. Neurological findings may be difficult to detect in young patients because many children with achondroplasia are normally hypotonic during early infancy, although they often exhibit developmental delay in achieving motor milestones.45 A small percentage of patients with stenosis of the foramen magnum have symptoms of cervicomedullary compression.45,46 In a prospective evaluation of 53 infants with achondroplasia, more than 70% had foramen magnum stenosis, but less than 10% demonstrated clinical symptoms of cervicomedullary compression.46
Sudden death as a catastrophic consequence of cervicomedullary compression has been reported in infants with achondroplasia.46,47 Hecht and colleagues reported a 7.5% risk for sudden death within the first year of life and a 2.5% risk for sudden death between 1 and 4 years of age in children with achondroplasia.47
Goldenhar’s Syndrome
Spinal abnormalities associated with GS include vertebral hypoplasia, failure of segmentation, and failure of vertebral formation. Segmentation defects are more common in the cervical spine, whereas vertebral formation abnormalities more frequently occur in the thoracolumbar spine. In one series, 60% of children with GS had vertebral anomalies,48 including block vertebrae (most often involving fusion of C3 and C4), unilateral thoracolumbar hemivertebrae, spina bifida occulta, butterfly vertebrae, and sacral agenesis. Many patients had abnormalities at multiple spinal levels.
Upper cervical spine anomalies may also be seen in association with GS. One group reported a 12% incidence of vertebral segmentation anomalies and occipitalization of the atlas.48 Odontoid hypoplasia with atlantoaxial instability has also been reported.49
Spondyloepiphysial Dysplasia
The most common spinal abnormalities in children with SED are odontoid hypoplasia and ligamentous laxity. Spinal cord compression from atlantoaxial instability causes myelopathy in as many as 35% of children with SED. The myelopathy usually develops gradually and is manifested as delayed motor development, slowly progressive weakness, spasticity, sleep apnea, and other respiratory abnormalities. Atlantoaxial instability has been found to progress with age in SED. Those with spinal canal diameters smaller than 10 mm at the level of the axis are at significantly increased risk for spinal cord compression.50,51
Morquio’s Syndrome
Mucopolysaccharidosis (MPS) type IV, or Morquio’s syndrome, is an autosomal recessive lysosomal storage disease that results from an inability to metabolize keratan sulfate, a glycosaminoglycan found predominantly in cartilage and the cornea.52,53 Patients often appear normal at birth and have normal growth and development for the first 2 years of life until the underlying skeletal abnormalities become clinically apparent between 2 and 6 years of age. The incidence of MPS IV is 1 in 40,000 live births. Many patients survive to early adulthood, at which time they may succumb to the cardiopulmonary and neurological complications of the disorder.
The most common spinal abnormality is atlantoaxial subluxation with spinal cord compression.54 Atlantoaxial subluxation has been identified in 42% to 90% of patients with Morquio’s syndrome.55 Odontoid dysplasia, which may be manifested as hypoplasia, aplasia, or os odontoideum, is common in MPS IV.
Osteogenesis Imperfecta
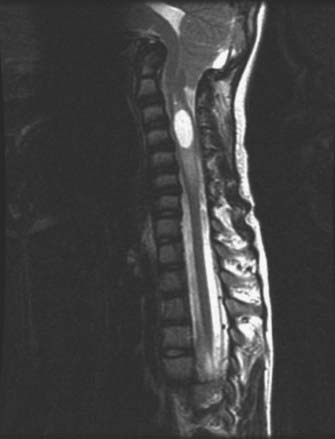
Osteogenesis imperfecta (OI) is a hereditary disorder caused by a defect in collagen production. The disease is characterized by osteopenia, fragile bones susceptible to fracture, short stature, and progressive skeletal deformity.56 The most commonly used classification system for OI is the Sillence classification system.57,58 Type I is mild with no long bone deformities, type II is lethal in the perinatal period with in utero fractures, type III is the most severe form in children who survive the perinatal period, and type IV is an undefined type with moderate bone deformities and variable short stature. Abnormalities at the craniovertebral junction are most commonly seen with type IV OI, with a prevalence ranging from rare to 25%.57 Osteoporotic bones resulting in repetitive microfracture cause infolding of the occipital condyles with elevation of the clivus and posterior cranial fossa. This leads to upward migration of the cervical spine into the foramen magnum and symptomatic compression of the brainstem and lower cranial nerves (Fig. 220-3).59
Larsen’s Syndrome
Larsen’s syndrome is a rare congenital disorder of connective tissue.60–69 The cervical spine is more commonly affected than the thoracic or lumbar spine. The most characteristic abnormalities include hypoplastic or flattened vertebral bodies, dysraphism, hemivertebrae, and wedged vertebrae.63,64 Midcervical subluxations and kyphosis have been described in 12% of patients with Larsen’s syndrome.64,70 With progression of the curve and increased instability, progressive myelopathy, segmental weakness, and even death may ensue as a result of respiratory insufficiency.61–6365 Cervical kyphosis associated with anterior-posterior disconnection syndrome has also been described.66,67,71
Neurofibromatosis Type 1
Neurofibromatosis type 1 (NF1) is the most common neurocutaneous syndrome, with an incidence of 1 in 3300 individuals.72,73 Spinal lesions occurring in patients with NF1 include cervical kyphosis, spinal meningocele, dural ectasia, and paravertebral tumors.74–78 Progressive cervical kyphosis may occur as a result of intrinsic ligamentous abnormality and abnormal bony architecture (Fig. 220-4). Cervical kyphosis can also occur after resection of soft tissue or extradural neurofibromas. The most common spine tumors in patients with NF1 are paraspinal neurofibromas.75 Growth of these lesions may result in expansion of the foramina, enlargement of the spinal canal, and widening of the interpedicular distance, all of which may contribute to the development of instability and scoliosis. These lesions are often asymptomatic.
Reconstruction of the cervical spine to correct kyphotic abnormalities in patients with NF1 is typically done from the anterior direction first, with multilevel diskectomies, fusions, and instrumentation at the appropriate level, followed by posterior rib and cable arthrodesis if necessary.79 Normal cervical alignment is the ultimate goal.
Kniest’s Syndrome
Kniest’s syndrome is a form of skeletal dysplasia characterized by typical facial features and large, stiff joints with contractures.80 The syndrome is similar to metatrophic dysplasia because of the enlarged, stiff joints and similar to SED because of impaired spinal and epiphyseal growth. Patients with Kniest’s syndrome have soft cartilage, which leads to osteopenia of the spine and extremities.
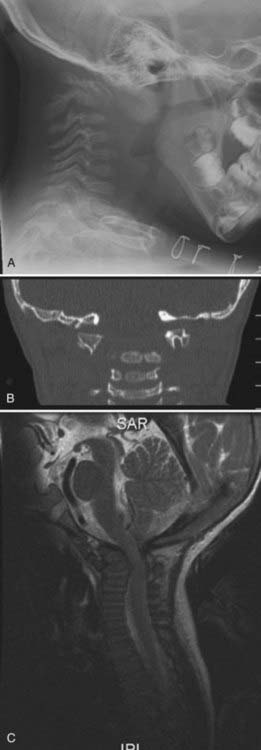
All regions of the spine are affected in patients with Kniest’s syndrome, with the most common problems being atlantoaxial instability, odontoid hypoplasia, cervical hypoplasia and instability, and kyphoscoliosis of the thoracolumbar spine (Fig. 220-5).81–84 Surgical challenges may be extreme because of poor bone quality and small patient size.
Os Odontoideum
Although os odontoideum may be more of a posttraumatic than congenital disorder, its existence is significant and should be discussed in the context of congenital cervical lesions. Os odontoideum consists of dissociation between the body of C2 and the dens such that a disconnected ossicle takes the place of the intact odontoid process.85
Patients with atlantoaxial instability from os odontoideum may be at risk for significant neurological injury. Most patients have neck pain and headaches from the instability, but instances of myelopathy, transient quadriparesis, and even sudden death after minor trauma have been reported as well.32 If instability is suspected, dynamic imaging with flexion and extension views should be obtained, augmented by CT or MRI. Posterior stabilization with rigid instrumentation techniques, without the use of a halo orthosis, has been shown to be extremely safe and effective for managing this disorder.28,86–95
Management of Specific Abnormalities by Anatomic Level
Occipitoatlantoaxial Level
Special situations arise in patents with basilar invagination or basilar impression. Basilar invagination is characterized by encroachment of the foramen magnum by the upper cervical elements, usually the odontoid.96–98 Basilar invagination may be associated with a variety of craniovertebral disorders, including occipitalization of the atlas, Chiari I malformation, syringomyelia, scoliosis, and KFS. Basilar impression has clinical characteristics similar to basilar invagination, but it is due to a bone-softening disorder such as OI.
Treatment of older children with basilar invagination or basilar impression usually begins with cranial traction and reduction. If the impression can be reduced, a posterior occipitocervical stabilization procedure can then be performed to maintain the reduction. If the invagination cannot be reduced or if the patient will not tolerate traction (common in younger children), transoral odontoid resection is performed, followed by posterior occipitocervical fusion. Patients with associated Chiari malformations will require suboccipital decompression, C1 laminectomy, and duraplasty during their posterior stabilization and fusion procedures.96–102
Subaxial Cervical Spine Anomalies
The decision to perform operative stabilization in a child with a congenital cervical spine lesion below C2 is based on evidence of cervical spinal instability, neurological deficit caused by a compressive lesion, and progressive deformity. Radiographic evidence of cervical spine instability is not absolute, but the following serve as useful guidelines: vertebral body angulation greater than 15 degrees, vertebral body subluxation greater than 5 mm, or unilateral or bilateral locked facets.79 Kyphotic angulation of more than 7 degrees probably represents significant ligamentous instability and predisposes the juvenile cervical spine to further kyphosis and instability.
Surgical stabilization for single-level cervical instability may be addressed from either an anterior or posterior direction. Typically, anterior cervical diskectomy and allograft fusion with rigid instrumentation or screw/rod instrumentation and fusion from a posterior direction will provide a solid arthrodesis. Multilevel cervical anomalies, including spondylolysis, high-grade spondylolisthesis, and significant kyphotic deformities, are uncommon but especially challenging from a surgical perspective.103–109 Surgical reconstruction for significant cervical deformities may be performed in staged fashion, first from the anterior direction with multilevel diskectomies or corpectomies, followed by posterior arthrodesis if necessary.79 Preoperative reduction with cervical traction may be useful in select, cooperative patients. Close attention must be paid to bone quality at surgery, and rigid internal fixation is important for achieving normal cervical alignment.
Bagley CA, Pindrik JA, Bookland MJ, et al. Cervicomedullary decompression for foramen magnum stenosis in achondroplasia. J Neurosurg. 2006;104:166-172.
Brockmeyer D. Advanced occipitocervical surgery in children. In: Brockmeyer D, editor. Advanced Pediatric Craniocervical Surgery. New York: Thieme; 2006:93-108.
Brockmeyer D. Down syndrome and craniovertebral instability. Topic review and treatment recommendations. Pediatr Neurosurg. 1999;31:71-77.
Brockmeyer DL, York JE, Apfelbaum RI. Anatomical suitability of C1-2 transarticular screw placement in pediatric patients. J Neurosurg. 2000;92:7-11.
Browd S, Healy LJ, Dobie G, et al. Morphometric and qualitative analysis of congenital occipitocervical instability in children: implications for patients with Down syndrome. J Neurosurg. 2006;105:50-54.
Dias MS. Normal and abnormal development of the spine. Neurosurg Clin N Am. 2007;18:415-429.
Gluf WM, Brockmeyer DL. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 67 pediatric patients. J Neurosurg Spine. 2005;2:164-169.
Goel A. Progressive basilar invagination after transoral odontoidectomy: treatment by atlantoaxial facet distraction and craniovertebral realignment. Spine. 2005;30:E551-E555.
Goel A. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;45:1497-1499.
Healey D, Letts M, Jarvis JG. Cervical spine instability in children with Goldenhar’s syndrome. Can J Surg. 2002;45:341-344.
Janus GJ, Engelbert RH, Beek E, et al. Osteogenesis imperfecta in childhood: MR imaging of basilar impression. Eur J Radiol. 2003;47:19-24.
Klimo PJr, Kan P, Rao G, et al. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neurosurg Spine. 2008;9:332-342.
Klimo PJr, Rao G, Brockmeyer D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007;18:463-478.
Klippel M, Feil A. The classic: a case of absence of cervical vertebrae with the thoracic cage rising to the base of the cranium (cervical thoracic cage). Clin Orthop Relat Res. 1975;109:3-8.
Laville JM, Lakermance P, Limouzy F. Larsen’s syndrome: review of the literature and analysis of thirty-eight cases. J Pediatr Orthop. 1994;14:63-73.
Lowry DW, Pollack IF, Clyde B, et al. Upper cervical spine fusion in the pediatric population. J Neurosurg. 1997;87:671-676.
Madera M, Crawford A, Mangano FT. Management of severe cervical kyphosis in a patient with Larsen syndrome. J Neurosurg Pediatr. 2008;1:320-324.
Menezes AH, Ryken TC. Craniovertebral abnormalities in Down’s syndrome. Pediatr Neurosurg. 1992;18:24-33.
Pauli RM, Scott CI, Wassman ERJr, et al. Apnea and sudden unexpected death in infants with achondroplasia. J Pediatr. 1984;104:342-348.
Pueschel SM, Scola FH. Atlantoaxial instability in individuals with Down syndrome: epidemiologic, radiographic, and clinical studies. Pediatrics. 1987;80:555-560.
Ryken TC, Menezes AH. Cervicomedullary compression in achondroplasia. J Neurosurg. 1994;81:43-48.
Stevens JM, Kendall BE, Crockard HA, et al. The odontoid process in Morquio-Brailsford’s disease. The effects of occipitocervical fusion. J Bone Joint Surg Br. 1991;73:851-858.
Tracy MR, Dormans JP, Kusumi K. Klippel-Feil syndrome: clinical features and current understanding of etiology. Clin Orthop Relat Res. 2004;424:183-190.
1 Tracy MR, Dormans JP, Kusumi K. Klippel-Feil syndrome: clinical features and current understanding of etiology. Clin Orthop Relat Res. 2004;424:183-190.
2 Tredwell SJ. Craniovertebral abnormalities in Down’s syndrome. Pediatr Neurosurg. 1993;19:224.
3 Tredwell SJ, Smith DF, Macleod PJ, et al. Cervical spine anomalies in fetal alcohol syndrome. Spine. 1982;7:331-334.
4 Klimo PJr, Rao G, Brockmeyer D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007;18:463-478.
5 Calvy TM, Segall HD, Gilles FH, et al. CT anatomy of the craniovertebral junction in infants and children. AJNR Am J Neuroradiol. 1987;8:489-494.
6 Christ B, Wilting J. From somites to vertebral column. Ann Anat. 1992;174:23-32.
7 David KM, McLachlan JC, Aiton JF, et al. Cartilaginous development of the human craniovertebral junction as visualised by a new three-dimensional computer reconstruction technique. J Anat. 1998;192:269-277.
8 Dias MS. Normal and abnormal development of the spine. Neurosurg Clin N Am. 2007;18:415-429.
9 Dias MS, Walker ML. The embryogenesis of complex dysraphic malformations: a disorder of gastrulation? Pediatr Neurosurg. 1992;18:229-253.
10 Khanna G, El-Khoury GY. Imaging of cervical spine injuries of childhood. Skeletal Radiol. 2007;36:477-494.
11 Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539-560.
12 Wang JC, Nuccion SL, Feighan JE, et al. Growth and development of the pediatric cervical spine documented radiographically. J Bone Joint Surg Am. 2001;83:1212-1218.
13 Byrd SE, Comiskey EM. Postnatal maturation and radiology of the growing spine. Neurosurg Clin N Am. 2007;18:431-461.
14 Sze G, Baierl P, Bravo S. Evolution of the infant spinal column: evaluation with MR imaging. Radiology. 1991;181:819-827.
15 Sze G, Bravo S, Baierl P, et al. Developing spinal column: gadolinium-enhanced MR imaging. Radiology. 1991;180:497-502.
16 Ogden JA. Radiology of postnatal skeletal development. XII. The second cervical vertebra. Skeletal Radiol. 1984;12:169-177.
17 Ogden JA. Radiology of postnatal skeletal development. XI. The first cervical vertebra. Skeletal Radiol. 1984;12:12-20.
18 Ogden JA, Murphy MJ, Southwick WO, et al. Radiology of postnatal skeletal development. XIII. C1-C2 interrelationships. Skeletal Radiol. 1986;15:433-438.
19 Bailey DK. The normal cervical spine in infants and children. Radiology. 1952;59:712-719.
20 Muller F, O’Rahilly R. Somitic-vertebral correlation and vertebral levels in the human embryo. Am J Anat. 1986;177:3-19.
21 Muller F, O’Rahilly R. Occipitocervical segmentation in staged human embryos. J Anat. 1994;185(pt 2):251-258.
22 Muller F, O’Rahilly R. Segmentation in staged human embryos: the occipitocervical region revisited. J Anat. 2003;203:297-315.
23 O’Rahilly R, Muller F, Meyer DB. The human vertebral column at the end of the embryonic period proper. 1. The column as a whole. J Anat. 1980;131:565-575.
24 O’Rahilly R, Muller F, Meyer DB. The human vertebral column at the end of the embryonic period proper. 2. The occipitocervical region. J Anat. 1983;136:181-195.
25 O’Rahilly R, Muller F, Meyer DB. The human vertebral column at the end of the embryonic period proper. 3. The thoracicolumbar region. J Anat. 1990;168:81-93.
26 O’Rahilly R, Muller F, Meyer DB. The human vertebral column at the end of the embryonic period proper. 4. The sacrococcygeal region. J Anat. 1990;168:95-111.
27 Davidson RG. Atlantoaxial instability in individuals with Down syndrome: a fresh look at the evidence. Pediatrics. 1988;81:857-865.
28 Nader-Sepahi A, Casey AT, Hayward R, et al. Symptomatic atlantoaxial instability in Down syndrome. J Neurosurg. 2005;103:231-237.
29 Brockmeyer D. Down syndrome and craniovertebral instability. Topic review and treatment recommendations. Pediatr Neurosurg. 1999;31:71-77.
30 Browd S, Healy LJ, Dobie G, et al. Morphometric and qualitative analysis of congenital occipitocervical instability in children: implications for patients with Down syndrome. J Neurosurg. 2006;105:50-54.
31 Menezes AH. Craniovertebral junction anomalies: diagnosis and management. Semin Pediatr Neurol. 1997;4:209-223.
32 Menezes AH, Ryken TC. Craniovertebral abnormalities in Down’s syndrome. Pediatr Neurosurg. 1992;18:24-33.
33 Pizzutillo PD, Herman MJ. Cervical spine issues in Down syndrome. J Pediatr Orthop. 2005;25:253-259.
34 Pueschel SM, Scola FH. Atlantoaxial instability in individuals with Down syndrome: epidemiologic, radiographic, and clinical studies. Pediatrics. 1987;80:555-560.
35 Roy M, Baxter M, Roy A. Atlantoaxial instability in Down syndrome—guidelines for screening and detection. J R Soc Med. 1990;83:433-435.
36 Pueschel SM, Scola FH, Pezzullo JC. A longitudinal study of atlanto-dens relationships in asymptomatic individuals with Down syndrome. Pediatrics. 1992;89:1194-1198.
37 Klippel M, Feil A. The classic: a case of absence of cervical vertebrae with the thoracic cage rising to the base of the cranium (cervical thoracic cage). Clin Orthop Relat Res. 1975;109:3-8.
38 Hensinger RN, Lang JE, MacEwen GD. Klippel-Feil syndrome; a constellation of associated anomalies. J Bone Joint Surg Am. 1974;56:1246-1253.
39 Baba H, Maezawa Y, Furusawa N, et al. The cervical spine in the Klippel-Feil syndrome. A report of 57 cases. Int Orthop. 1995;19:204-208.
40 Clarke RA, Catalan G, Diwan AD, et al. Heterogeneity in Klippel-Feil syndrome: a new classification. Pediatr Radiol. 1998;28:967-974.
41 Herman MJ, Pizzutillo PD. Cervical spine disorders in children. Orthop Clin North Am. 1999;30:457-466. ix
42 Ruiz-Garcia M, Tovar-Baudin A, Del Castillo-Ruiz V, et al. Early detection of neurological manifestations in achondroplasia. Childs Nerv Syst. 1997;13:208-213.
43 Ryken TC, Menezes AH. Cervicomedullary compression in achondroplasia. J Neurosurg. 1994;81:43-48.
44 Bagley CA, Pindrik JA, Bookland MJ, et al. Cervicomedullary decompression for foramen magnum stenosis in achondroplasia. J Neurosurg. 2006;104:166-172.
45 Rimoin DL. Cervicomedullary junction compression in infants with achondroplasia: when to perform neurosurgical decompression. Am J Hum Genet. 1995;56:824-827.
46 Pauli RM, Scott CI, Wassman ERJr, et al. Apnea and sudden unexpected death in infants with achondroplasia. J Pediatr. 1984;104:342-348.
47 Hecht JT, Francomano CA, Horton WA, et al. Mortality in achondroplasia. Am J Hum Genet. 1987;41:454-464.
48 Gibson JN, Sillence DO, Taylor TK. Abnormalities of the spine in Goldenhar’s syndrome. J Pediatr Orthop. 1996;16:344-349.
49 Healey D, Letts M, Jarvis JG. Cervical spine instability in children with Goldenhar’s syndrome. Can J Surg. 2002;45:341-344.
50 Miyoshi K, Nakamura K, Haga N, et al. Surgical treatment for atlantoaxial subluxation with myelopathy in spondyloepiphyseal dysplasia congenita. Spine. 2004;29:E488-E491.
51 Nakamura K, Miyoshi K, Haga N, et al. Risk factors of myelopathy at the atlantoaxial level in spondyloepiphyseal dysplasia congenita. Arch Orthop Trauma Surg. 1998;117:468-470.
52 De Franceschi L, Roseti L, Desando G, et al. A molecular and histological characterization of cartilage from patients with Morquio syndrome. Osteoarthritis Cartilage. 2007;15:1311-1317.
53 Montano AM, Tomatsu S, Gottesman GS, et al. International Morquio A Registry: clinical manifestation and natural course of Morquio A disease. J Inherit Metab Dis. 2007;30:165-174.
54 Takeda E, Hashimoto T, Tayama M, et al. Diagnosis of atlantoaxial subluxation in Morquio’s syndrome and spondyloepiphyseal dysplasia congenita. Acta Paediatr Jpn. 1991;33:633-638.
55 Stevens JM, Kendall BE, Crockard HA, et al. The odontoid process in Morquio-Brailsford’s disease. The effects of occipitocervical fusion. J Bone Joint Surg Br. 1991;73:851-858.
56 Engelbert RH, Gerver WJ, Breslau-Siderius LJ, et al. Spinal complications in osteogenesis imperfecta: 47 patients 1-16 years of age. Acta Orthop Scand. 1998;69:283-286.
57 Sillence DO. Craniocervical abnormalities in osteogenesis imperfecta: genetic and molecular correlation. Pediatr Radiol. 1994;24:427-430.
58 Sillence DO, Rimoin DL. Classification of osteogenesis imperfect. Lancet. 1978;1:1041-1042.
59 Janus GJ, Engelbert RH, Beek E, et al. Osteogenesis imperfecta in childhood: MR imaging of basilar impression. Eur J Radiol. 2003;47:19-24.
60 Larsen LJ, Schottstaedt ER, Bost FC. Multiple congenital dislocations associated with characteristic facial abnormality. J Pediatr. 1950;37:574-581.
61 Laville JM, Lakermance P, Limouzy F. Larsen’s syndrome: review of the literature and analysis of thirty-eight cases. J Pediatr Orthop. 1994;14:63-73.
62 Micheli LJ, Hall JE, Watts HG. Spinal instability in Larsen’s syndrome: report of three cases. J Bone Joint Surg Am. 1976;58:562-565.
63 Banks JT, Wellons JC3rd, Tubbs RS, et al. Cervical spine involvement in Larsen’s syndrome: a case illustration. Pediatrics. 2003;111:199-201.
64 Bowen JR, Ortega K, Ray S, et al. Spinal deformities in Larsen’s syndrome. Clin Orthop Relat Res. 1985;197:159-163.
65 Forese LL, Berdon WE, Harcke HT, et al. Severe mid-cervical kyphosis with cord compression in Larsen’s syndrome and diastrophic dysplasia: unrelated syndromes with similar radiologic findings and neurosurgical implications. Pediatr Radiol. 1995;25:136-139.
66 Katz DA, Hall JE, Emans JB. Cervical kyphosis associated with anteroposterior dissociation and quadriparesis in Larsen’s syndrome. J Pediatr Orthop. 2005;25:429-433.
67 Luk KD, Yip DK. Congenital anteroposterior spinal dissociation in Larsen’s syndrome: report on two operated cases with long-term follow-up. Spine. 2002;27:E296-E300.
68 Weisenbach J, Melegh B. Vertebral anomalies in Larsen’s syndrome. Pediatr Radiol. 1996;26:682-683.
69 Johnston CE2nd, Birch JG, Daniels JL. Cervical kyphosis in patients who have Larsen syndrome. J Bone Joint Surg Am. 1996;78:538-545.
70 Madera M, Crawford A, Mangano FT. Management of severe cervical kyphosis in a patient with Larsen syndrome. J Neurosurg Pediatr. 2008;1:320-324.
71 Sakaura H, Matsuoka T, Iwasaki M, et al. Surgical treatment of cervical kyphosis in Larsen syndrome: report of 3 cases and review of the literature. Spine. 2007;32:E39-E44.
72 Al-Otibi M, Rutka JT. Neurosurgical implications of neurofibromatosis type I in children. Neurosurg Focus. 2006;20(1):E2.
73 Cnossen MH, de Goede-Bolder A, van den Broek KM, et al. A prospective 10 year follow up study of patients with neurofibromatosis type 1. Arch Dis Child. 1998;78:408-412.
74 Rockower S, McKay D, Nason S. Dislocation of the spine in neurofibromatosis. A report of two cases. J Bone Joint Surg Am. 1982;64:1240-1242.
75 Khong PL, Goh WH, Wong VC, et al. MR imaging of spinal tumors in children with neurofibromatosis 1. AJR Am J Roentgenol. 2003;180:413-417.
76 Thakkar SD, Feigen U, Mautner VF. Spinal tumours in neurofibromatosis type 1: an MRI study of frequency, multiplicity and variety. Neuroradiology. 1999;41:625-629.
77 Lee M, Rezai AR, Freed D, et al. Intramedullary spinal cord tumors in neurofibromatosis. Neurosurgery. 1996;38:32-37.
78 Isu T, Miyasaka K, Abe H, et al. Atlantoaxial dislocation associated with neurofibromatosis. Report of three cases. J Neurosurg. 1983;58:451-453.
79 Brockmeyer D. Advanced surgery for the subaxial cervical spine in children. In: Brockmeyer D, editor. Advanced Pediatric Craniocervical Surgery. New York: Thieme; 2006:109-122.
80 Spranger J, Winterpacht A, Zabel B. Kniest dysplasia: Dr. W. Kniest, his patient, the molecular defect. Am J Med Genet. 1997;69:79-84.
81 Ain MC, Chaichana KL, Schkrohowsky JG. Retrospective study of cervical arthrodesis in patients with various types of skeletal dysplasia. Spine. 2006;31:E169-E174.
82 Merrill KD, Schmidt TL. Occipitoatlantal instability in a child with Kniest syndrome. J Pediatr Orthop. 1989;9:338-340.
83 Spranger JW, Maroteaux P. Kniest disease. Birth Defects Orig Artic Ser. 1974;10:50-56.
84 Westvik J, Lachman RS. Coronal and sagittal clefts in skeletal dysplasias. Pediatr Radiol. 1998;28:764-770.
85 Klimo PJr, Kan P, Rao G, et al. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neurosurg Spine. 2008;9:332-342.
86 Menezes AH. Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervical junction.”. Childs Nerv Syst. 2008;24:1187-1193.
87 Menezes AH. Specific entities affecting the craniocervical region: Down’s syndrome. Childs Nerv Syst. 2008;24:1165-1168.
88 Ahmed R, Traynelis VC, Menezes AH. Fusions at the craniovertebral junction. Childs Nerv Syst. 2008;24:1209-1224.
89 Reilly CW, Choit RL. Transarticular screws in the management of C1-C2 instability in children. J Pediatr Orthop. 2006;26:582-588.
90 Leonard JR, Wright NM. Pediatric atlantoaxial fixation with bilateral, crossing C-2 translaminar screws. Technical note. J Neurosurg. 2006;104:59-63.
91 Gluf WM, Brockmeyer DL. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 67 pediatric patients. J Neurosurg Spine. 2005;2:164-169.
92 Dai L, Yuan W, Ni B, et al. Os odontoideum: etiology, diagnosis, and management. Surg Neurol. 2000;53:106-108.
93 Brockmeyer DL, York JE, Apfelbaum RI. Anatomical suitability of C1-2 transarticular screw placement in pediatric patients. J Neurosurg. 2000;92:7-11.
94 Lowry DW, Pollack IF, Clyde B, et al. Upper cervical spine fusion in the pediatric population. J Neurosurg. 1997;87:671-676.
95 Stevens JM, Chong WK, Barber C, et al. A new appraisal of abnormalities of the odontoid process associated with atlanto-axial subluxation and neurological disability. Brain. 1994;117:133-148.
96 Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1:281-286.
97 Goel A. Progressive basilar invagination after transoral odontoidectomy: treatment by atlantoaxial facet distraction and craniovertebral realignment. Spine. 2005;30:E551-E555.
98 Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88:962-968.
99 Brockmeyer D. Advanced occipitocervical surgery in children. In: Brockmeyer D, editor. Advanced Pediatric Craniocervical Surgery. New York: Thieme; 2006:93-108.
100 Goel A. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;45:1497-1499.
101 Goel A, Sharma P. Craniovertebral junction realignment for the treatment of basilar invagination with syringomyelia: preliminary report of 12 cases. Neurol Med Chir (Tokyo). 2005;45:512-517.
102 Menezes AH. Craniovertebral junction database analysis: incidence, classification, presentation, and treatment algorithms. Childs Nerv Syst. 2008;24:1101-1108.
103 Cautilli RA, Joyce MF, Lin PM. Congenital elongation of the pedicles of the sixth cervical vertebra in identical twins. J Bone Joint Surg Am. 1972;54:653-656.
104 Dawley JA. Spondylolisthesis of the cervical spine. Case report. J Neurosurg. 1971;34:99-101.
105 Forsberg DA, Martinez S, Vogler JB3rd, et al. Cervical spondylolysis: imaging findings in 12 patients. AJR Am J Roentgenol. 1990;154:751-755.
106 Goupille P, Fouquet B, Cotty P, et al. Cervical spondylolysis. AJR Am J Roentgenol. 1991;157:1127-1128.
107 Legaye J, Horduna M. Cervical spondylolysis in a child: a case with hypermobility. Spine J. 2009;9:e15-e19.
108 Poggi JJ, Martinez S, Hardaker WTJr, et al. Cervical spondylolysis. J Spinal Disord. 1992;5:349-356.
109 Tokgozoglu AM, Alpaslan AM. Congenital spondylolisthesis in the upper spinal column. Management of two cases. Spine. 1994;19:99-102.