20
Cervical neoplasia
Introduction
Cervical cancer is the most common cancer among women in many developing countries, and worldwide, there are over 450 000 cases each year. The overall lifetime risk is about 5% in parts of Africa, India and Latin America, compared with 1% in Europe and North America. About 3400 cases of cervical cancer are presently diagnosed each year in the UK, and 1300 of these women will die from the disease. In the UK, cervical cancer is relatively uncommon, representing around 2% of female cancers. It is however the most common cancer in young females.
Fortunately, cervical cancer has a premalignant phase and many of the criteria for a suitable screening programme are fulfilled. The aim of this screening is to detect premalignant cervical disease by means of a ‘smear test’ and treat the premalignant disease before invasion occurs. Both the incidence and mortality have fallen considerably since the introduction of this screening programme.
Cervical intraepithelial and cervical cancer screening
Transformation zone
Cervical intraepithelial neoplasia (CIN) develops in the transformation zone of the cervix. Understanding the transformation zone is the key to understanding cervical cancer screening. The endocervix is lined by columnar epithelium and the ectocervix by squamous epithelium. Under the influence of oestrogen, part of the endocervix everts, thereby exposing the columnar epithelium to the chemical environment of the upper vagina (Fig. 20.1). The change in pH, along with other factors, causes the delicate columnar epithelium cells to transform into squamous epithelium through the process of metaplasia. CIN can develop in this transformation zone and it is this area which is sampled cytologically.
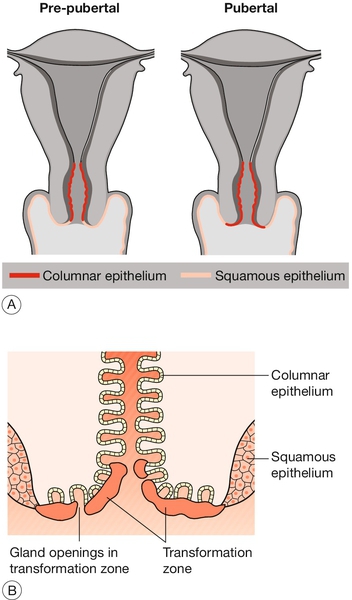
Fig. 20.1The transformation zone.
(A) The cervix everts at puberty, exposing the columnar epithelium of the endocervical canal. (B) This epithelium, referred to as the transformation zone, gradually undergoes metaplasia to squamous epithelium.
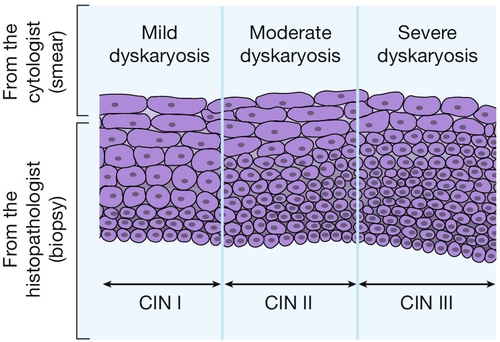
Cells shed from the surface may be sampled by a variety of devices, so that cells from both the endocervix and ectocervix can then be examined microscopically for cytological abnormalities. Cellular abnormalities are classified into different degrees of ‘dyskaryosis’. Although dyskaryosis is a cytological diagnosis (Fig. 20.2), the degree of dyskaryosis correlates to some extent, with the degree of cervical intraepithelial neoplasia, which is a histological diagnosis (Figs 20.3 and 20.4). The difference being that cytology looks at individual cells, whereas histology examines the cells as a tissue and therefore has architecture. As well as examining the desquamated cervical cells, cervical smear reports may also identify infection such as candidal, trichomonal or wart virus infection. Rarely, they may identify cells from other parts of the genital tract, such as malignant endometrial or ovarian cells.
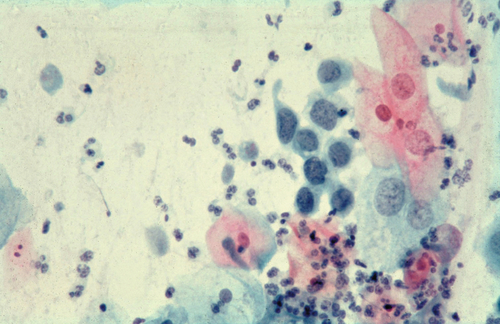
Fig. 20.2Slide prepared from a cervical smear.
There is moderate dysplasia with hyperchromasia, irregular nuclei and multinucleation. This slide also shows Trichomonas vaginalis, leucocytosis and a spermatozoon.
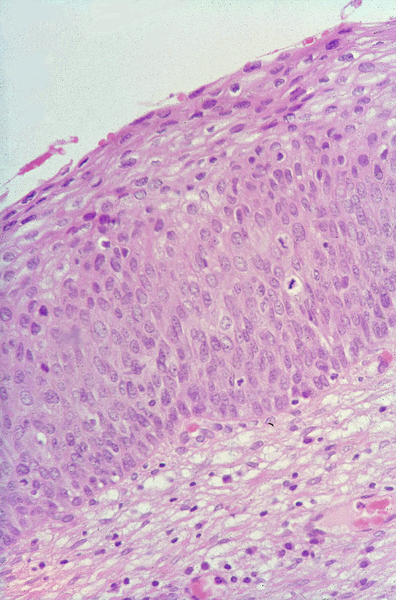
Fig. 20.4CIN II in a biopsy specimen.
There are abnormal cells arising from the basal layer, but not extending to the full thickness of the epithelium.
The precise rates of progression and spontaneous resolution of the disease are unknown. Roughly one-third of lesions will progress to the next stage (CIN I–II, CIN II–III, etc.), a third will remain unchanged and a third will regress. The duration of progression to invasive carcinoma is variable, but the average is perhaps around 10 years.
Screening recommendations
In the UK, there is an organized systematic computerized screening programme with national recommendations to screen from the ages of 20–65 years. Different regions, however, have different protocols, and England has recently recommended screening from the age of 25 years.
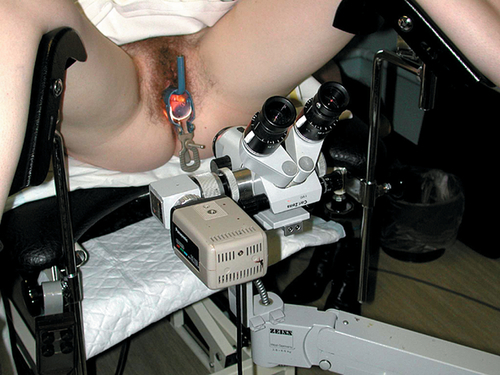
Colposcopy
Significant dyskaryosis on a cervical smear is an indication for further assessment with colposcopy. This is a procedure by which the cervix is examined in more detail using a type of binocular microscope referred to as a ‘colposcope’ (Fig. 20.5). Although moderate and severe dyskaryosis are absolute indications for colposcopy, controversy exists as to whether it is required for mild dyskaryosis. Some believe it is important, while others are concerned it may lead to over-treatment of lesions, which will often regress spontaneously. The indications for colposcopy are listed in Box 20.1.
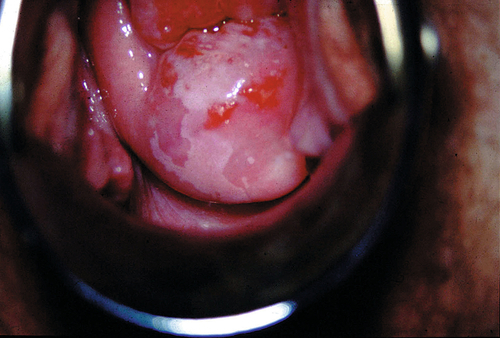
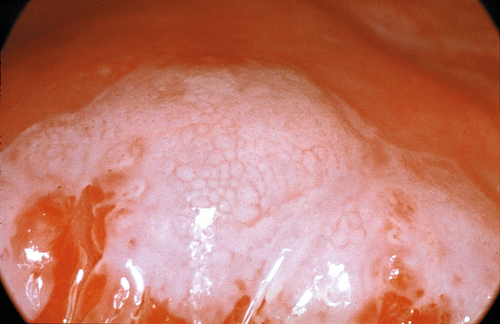
The patient is placed in the lithotomy position and a bivalve speculum is then inserted to allow visualization of the cervix. It is important to identify the squamocolumnar junction (SCJ). Abnormal epithelium, such as CIN, contains an increased amount of protein and lower levels of glycogen than normal epithelium. If acetic acid is applied to the cervix, the protein coagulates and the abnormal cells appear white: ‘aceto-white’ (Fig. 20.6). There may also be a ‘mosaic’ pattern with patches of aceto-white separated by areas of red vessels (Fig. 20.7). Some of the vascular patterns may appear ‘punctated’ if the vessels are viewed end-on. The inter-vessel distance increases with more severe lesions, and bizarre branching with coarse punctation and atypical vessels suggests invasive disease. Lugol’s iodine (Schiller’s iodine) stains glycogen mahogany brown, and the abnormal cells, which have less glycogen and therefore take up less iodine, can also be viewed in this way.
Treatment of CIN
High-grade CIN (CIN II and III) requires treatment. With CIN I, there is more controversy and generally a period of cytological surveillance will be employed, as many of these lesions will spontaneously resolve. If high-grade CIN is suspected colposcopically, the options are to treat immediately (termed ‘see-and-treat’) using an excisional method (e.g. large loop excision of the transformation zone, LLETZ) or to biopsy to confirm high-grade CIN and treat thereafter. This depends on the certainty of the colposcopic findings and the likelihood that the patient will attend for the follow-up.
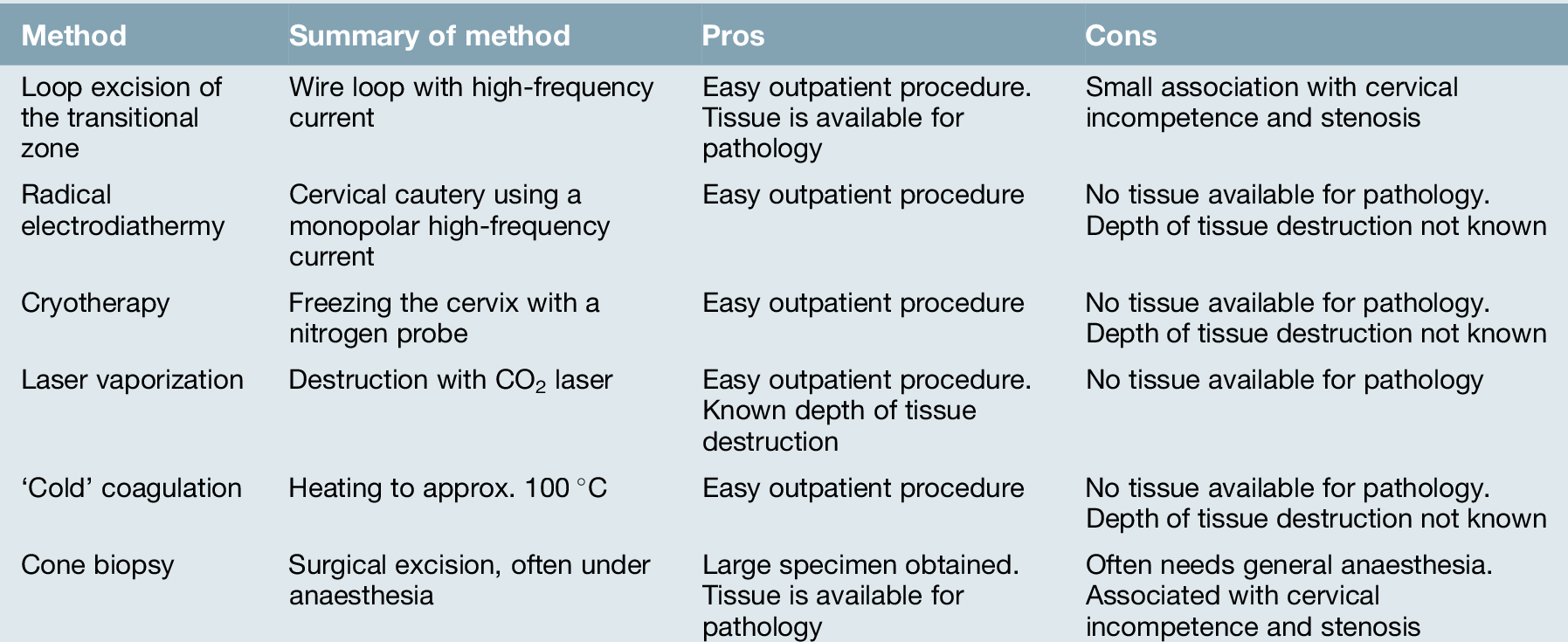
The cervix is infiltrated directly with local anaesthetic, and a loop diathermy excision or some other form of excision is performed (Fig. 20.8). The alternative of ablating the area has the disadvantage that the histological assessment is less complete (see Table 20.1). As smoking is an aetiological factor, its cessation should be discussed with the patient.

Fig. 20.8An area of CIN II has been excised using a loop (Table 20.1).
The cauterized area heals spontaneously.
Follow-up
Any woman who has had CIN, whether treated or not, continues to be at risk of developing cervical cancer due to either incomplete treatment of her CIN or the development of new disease. Follow-up is therefore important and this is usually carried out cytologically by repeating smears. Colposcopy can also be used. National protocols vary, but, following successful treatment of CIN, it is reasonable to arrange a follow-up smear after 6 months, and then annually for 5–10 years, before returning to the national screening programme if the smears have been negative.
Success of the UK cervical screening programme
The aim of screening is to identify women at high risk of cervical cancer to enable intervention at a time that allows treatment to substantially reduce this risk. The screening programme, although successful, will not be able to prevent all cervical cancers. It is estimated that for the UK cervical screening programme, for women aged between 25 and 49 years, 3-yearly screening prevents 84 cervical cancers out of every 100 that would develop without screening.
Cervical cancer
Aetiological factors
Cervical cancer arises from areas of CIN, as noted above. At least 30% of patients with CIN III, if left untreated, will probably go on to develop invasive disease over a period of 5–20 years.
Sexual behaviour
Cervical cancer is usually a disease of sexually active women and has been linked mainly to human papillomavirus (HPV). Women with cervical cancer are likely to have had more sexual partners and to have started intercourse earlier, and are less likely to have used barrier methods of contraception, compared with other women. The sexual behaviour of their partners may also be important. The disease is more frequent in parous women.
Human papillomavirus
A strong association has been observed between HPV serotypes 16 and 18, pre-invasive disease and invasive cervical cancer. It is believed that certain serotypes of HPV are important cofactors in the development of cervical cancer and may act by producing proteins (E6/7) which affect the action of the p53 gene product. The p53 gene is important in repairing DNA, and, if damaged, may predispose to malignant change. HPV is present in around one-third of all women in their 20s in the UK.
The combined oral contraceptive pill
Studies have shown that prolonged use of the oral contraceptive pill increases the risk of cervical cancer up to four-fold, but only in women who carry HPV. It can be argued that this effect is attributable to differences in sexual behaviour, rather than to the pill itself.
Smoking
Women who smoke are also at increased risk of developing cervical cancer. This may be due to alterations in immune function in the cervical epithelium or chemical carcinogenesis.
Future prevention
As certain subtypes of HPV are now known to be the main aetiological factors associated with the development of cervical cancer, there has been significant effort to develop a vaccine to these virus subtypes. Two separate vaccines have been developed with the aim of protecting an individual from the common oncogenic HPV subtypes. Cervarix and Gardasil have now passed through clinical trials and are available in many countries. It is thought that for these vaccines to be most effective, girls should be inoculated before they have become sexually active. Routine inoculation of girls at the age of 12–13 has commenced in the UK. The intended benefit is to reduce the incidence of cervical carcinoma by 70%. As not every cervical cancer will be prevented, however, it is important that cervical screening continues.
Presentation
Patients with cervical cancer may present with post-coital bleeding, intermenstrual bleeding, menorrhagia or an offensive vaginal discharge. In early cases, there may be no symptoms, and the diagnosis is made only after abnormal cervical cytology is discovered. Other symptoms such as backache, referred leg pain, leg oedema, haematuria or alteration in bowel habit, are usually associated with advanced-stage disease. General malaise, weight loss and anaemia are also late features.
Three categories of clinical appearance are described.
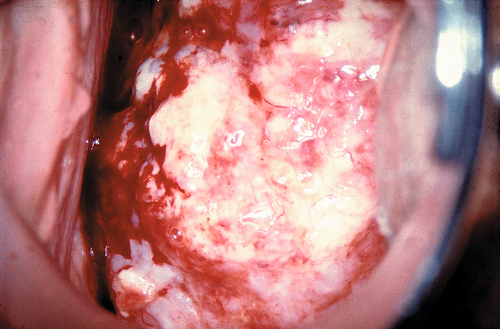
1. The most common is an exophytic lesion (Fig. 20.9). It usually arises on the ectocervix, often producing a large friable polypoid mass which bleeds easily. It can also arise from within the endocervical canal so that the canal becomes distended and ‘barrel-shaped’.
2. An infiltrating tumour shows little ulceration or exophytic growth but tends to produce a hard indurated cervix
3. An ulcerative tumour erodes a portion of the cervix and vaginal vault, producing a crater with local infection and seropurulent discharge.
Pathology
The majority of cervical cancers are squamous, and may be of keratinizing (the commonest), large cell, non-keratinizing and small cell subtypes. Around 10–25% are adenocarcinomas. There may also be coexistent squamous metaplasia or neoplasia (adenosquamous carcinoma).
Spread
Cervical cancer spreads by direct extension into adjacent structures and via the draining lymphatics. Blood-borne metastases are rare. Direct invasion beyond the cervix is usually into the upper vagina, parametrium and pelvic sidewall, and this tumour may lead to ureteric obstruction. There may also be invasion of the bladder and rectum.
There is no predictable pattern of lymphatic spread, with paracervical, parametrial and both internal and external iliac nodes potentially involved. There may also be spread to the common iliac, para-aortic and left supraclavicular area.
The risk of lymph node metastases correlates with both stage and tumour volume. Around 10% of patients with apparent stage I disease have pelvic node involvement. The incidence of para-aortic node involvement is less, at around 5% of patients with stage I disease and 25% with stage III disease.
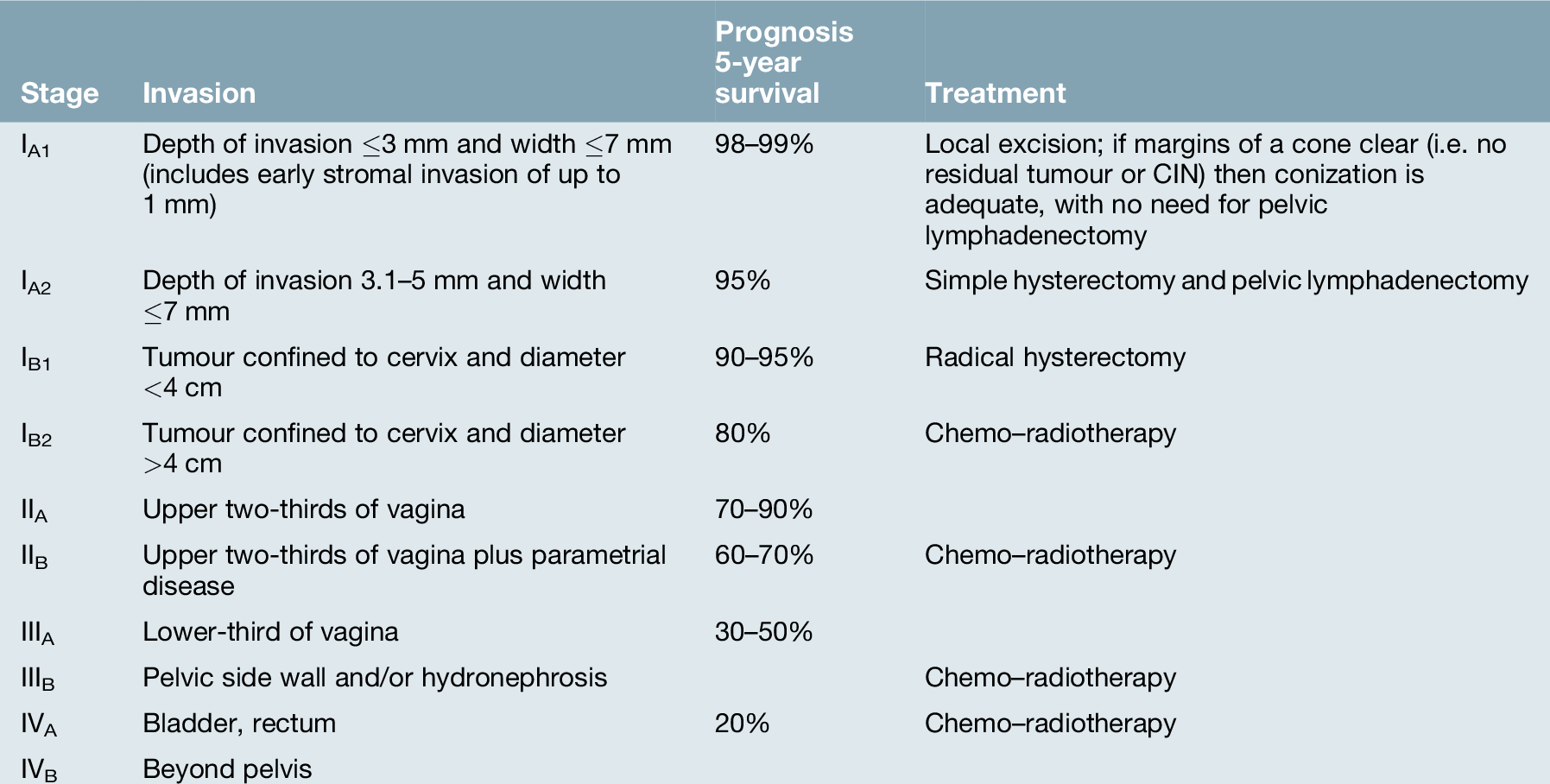
Staging, investigation and prognostic factors
Cervical cancer is staged (FIGO) by clinical examination (Table 20.2), which is often carried out under anaesthetic, and the diagnosis confirmed histologically by biopsy. The examination should include a rectovaginal examination to assess parametrial involvement. The stage is not altered by subsequent radiological (e.g. MRI or CT) or surgico–pathological findings (although in early disease, the histological dimensions of the tumour are important). Although this may seem inconsistent, it is to maintain consistency with other parts of the world where the disease is more common but where ‘high tech’ imaging is not always available. Despite this, clinical management is based upon the best assessment of the disease. The use of MRI and CT scanning has replaced the use of cystoscopy and intravenous urography (IVU) in many centres. The use of PET/CT is now being more widely used to assess the extent of lymph node involvement and this allows more individualized radiotherapy. If nodes are radiologically suspicious, for example, it is likely to be more appropriate to avoid surgery and treat with chemotherapy and radiotherapy.
Although in developed countries a greater proportion of cases present with stage I disease, in worldwide terms, the majority (> 75%) of women with cervical cancer present with advanced stage (stage III/IV) disease. The prognosis for patients with early-stage disease is relatively good (Table 20.2) but the prognosis for patients with advanced-stage disease is poor.
Management
Stage IA1–IA2
Stage IA1 can be cured by simple excision. If preservation of fertility is required, a cone biopsy with close cytological follow-up may be adequate treatment; where preservation of fertility is not important, simple hysterectomy is preferable. In all other cases of stage I disease, more aggressive treatment with either radical radiotherapy or radical surgery is required. With stage IA2 there is around 5% chance of nodal involvement. In these patients, local excision, as above, would be combined with formal pelvic lymphadenectomy. If these nodes are positive, adjuvant radiotherapy would be required too.
Stage IB–IIA
The choice between radical hysterectomy and radical radiotherapy is determined by the size and distribution of the cancer as well as the clinical condition of the patient. There is no difference in survival between the two methods but there are significant differences in morbidity.
Radical hysterectomy and pelvic lymphadenectomy involve total hysterectomy, excision of the parametria, upper two-thirds of the vagina and paracolpos, as well as dissection of the pelvic lymph nodes. The key surgical principle is to obtain a satisfactory surgical margin and to be able to histologically assess the draining lymphatics. Oophorectomy may be performed if appropriate, but the ovaries are rarely the site of metastatic spread and usually can be safely conserved. The operative mortality is < 1%, although potential morbidity includes infection, thromboembolic disease, haemorrhage and ureteric fistulae. There are also medium-term problems with reduced bladder sensation and voiding difficulties, together with long-term problems of high residual urinary volumes, recurrent urinary infections, stress incontinence and lymphocyst formation.
Radical radiotherapy usually consists of external beam therapy (teletherapy) to the pelvis and local vaginal therapy (brachytherapy). There is now evidence that combining this with cisplatin chemotherapy, increases the survival rate and this has become the standard of care. Teletherapy is delivered in fractions over a number of weeks to treat the pelvic lymphatics, whereas with brachytherapy a vaginal delivery system is inserted and left in situ for 12–18 h to irradiate central disease. In the UK, brachytherapy is now in the form of high-dose radiotherapy, which results in much shorter treatment times. The radiation dose which can be given is limited by the size of the lesion and the proximity of the bladder and bowel, both of which are particularly susceptible to radiation damage. The principal morbidity results from vaginal dryness, which can lead to sexual dysfunction, radiation cystitis, proctitis and vaginal stenosis. As this morbidity often gets worse with time, surgery is considered to be more suitable for those patients who are younger. In those found to have positive pelvic nodes postoperatively, it is usual to offer adjuvant chemotherapy and radiotherapy (chemo–radiotherapy).
Patients with stage IB1 will be offered either surgery or chemo–radiotherapy. In most modern cancer centres, patients will be extensively imaged. If there is a suggestion of extension outwith the cervix, then chemo–radiotherapy would be advised rather than surgery. There are two reasons for this: first, the morbidity associated with radical surgery plus chemo–radiotherapy is significantly greater that with the latter alone and second, if the cervix has been removed, it is not possible to give the high doses, via brachytherapy, that are required to achieve local control.
Similarly, for patients with stage IB2 and stage IIA, chemo–radiotherapy would now normally be advised. The reason for this is that even if radical surgery was to be successful, the likelihood of an unsatisfactory margin or positive nodes is sufficiently great to make adjuvant treatment likely.
For patients with small stage IB1 lesions that have been assessed in detail with MRI/CT imaging, and in whom future fertility is important, there is the possibility of radical local treatment. This is called radical trachelectomy and lymphadenectomy. The cervix is removed along with the paracervical tissues but the uterus is left in situ with a special suture left to maintain ‘cervical competence’. The lymph nodes are also removed. This approach is still being evaluated – although it offers the patient the potential of future pregnancy, it is not without significant problems.
Stage IIB–IV
The treatment of advanced-stage disease usually involves radical radiotherapy in combination with cisplatin chemotherapy. Failure to cure inoperable cervical cancer may result from suboptimal treatment of the central disease or the existence of lymph node metastases. With large lesions, the sensitivity of adjacent structures to radiation may prevent the use of curative radiation doses at the tumour periphery, and furthermore, some tumours may be radio-resistant.
Recurrent disease
Those patients with recurrence have a 1-year survival of around 10–15%. Most recurrences are suitable for palliative care only. If the patient has not been previously treated with radiotherapy, this may be a treatment option, but the majority of patients will have already had radical radiotherapy. Patients with a central pelvic recurrence may be cured by pelvic exenteration (excision of vagina/uterus with the bladder or rectum or both). With careful selection, up to 60% of these cases may survive 5 years, but the operation is associated with major morbidity.
The remaining patients may benefit from chemotherapy to palliate symptomatic recurrence or radiotherapy to palliate recurrence involving bone or nerve roots. The most active chemotherapy agents are cisplatin and ifosfamide, and combinations based on these drugs cause initial tumour shrinkage in up to 70% of cases. The main benefit from chemotherapy is the relief of disease-related symptoms, such as pelvic pain, but chemotherapy itself can cause considerable toxicity and does not improve survival in these women.