26 Cervical Kyphosis
KEY POINTS
Biomechanics of the Cervical Spine
Cervical Motion and the Spinal Cord
Many studies have focused on the effect of neck motion on the spinal cord. These concepts become particularly important in the setting of cervical kyphosis as the spinal cord is stretched over the area of deformity. Cadaveric studies have demonstrated that neck motion may result in injury to the spinal cord when the tensile load on the spinal cord exceeds the strength of spinal cord fibers to bear this load. The mechanism of injury has been identified as loss of axonal integrity secondary to stretch-induced injury. This form of injury has significant consequences on the conduction of electrical signals through white matter. These conduction deficits are as follows1: transient ionic imbalances from altered axonal membrane permeability, conduction loss from myelin damage, and irreversible conduction loss in the setting of profound damage to axons. Furthermore, ischemic damage may result from impingement of transverse arterioles caused by anterior compression of the spinal cord.2 Cervical kyphosis can aggravate this compression, placing the patient at risk of significant spinal cord damage with the potential for serious functional consequences. Prevention of further neurological injury is of primary consideration in the management of patients with cervical kyphosis.
Degenerative Processes in the Cervical Spine
The evolutionary function of the cervical spine is to allow for support and orientation of the head. This places the head in an ideal position for use of all sensory modalities including vision, hearing, taste, and smell. The cervical spine also plays a crucial role in the protection of the spinal cord and nerve roots. In their review, Yoganandan and colleagues summarize how the various bones, muscles, tendons, ligaments, and connective tissue structures serve to maintain proper alignment throughout the various movements.3 However, each of the different tissues contributes differently because of its unique structure and composition. Though an in-depth review of the soft tissue biomechanics is beyond the scope of this discussion, there are certain factors which are pertinent in the diskussion of cervical kyphosis.
Ligamentous structures are composed of collagen fibers and serve to resist tensile or distractive forces at extremes of motion. Each of the ligaments of the cervical spine resists different external forces due to its particular orientation and the components to which it is attached. Resistance to distraction is most effective when the force is applied along the direction of the fibers. As an example, interspinous ligaments are crucial for resisting excessive movement during flexion. Likewise, the anterior longitudinal ligament is most important for resisting motion during extension of the neck. With age, the composition of ligaments changes to contain proportionately more elastin than collagen.4 As a result, the ligaments are not as resistant to distractive forces causing the spine to become less stable both at rest and during motion. With a kyphotic deformity, age and ligamentous laxity may contribute to progression of the deformity and cause abnormal stress on the posterior elements and disk spaces, leading to facet joint hypertrophy and osteophyte formation.
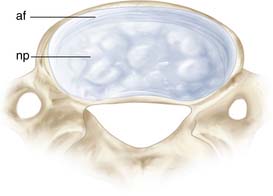
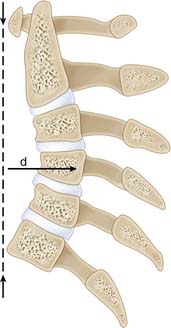
While ligaments serve to resist distractive forces, the structure of the intervertebral disk allows it to resist forces in several directions. The structure of the cervical disk is unique compared to the thoracic or lumbar spine, in that the annulus is not a circumferential structure.5 In the cervical spine, the annulus is thickest at the anterior portion of the disk and tapers laterally toward the uncovertebral joints. Posteriorly, there is a small remnant of the annulus in the midline position (Figure 26-2). The primary function of the intervertebral disk in the cervical spine is to resist compressive forces. Through the aging process, the normal physiology of the intervertebral disk changes such that the equilibrium of matrix synthesis and degradation is altered. Moreover, the structure of the matrix becomes increasingly disorganized, water is lost, and there is narrowing of the intervertebral disk.6 Progression of these degenerative changes is influenced by age-related changes to the vertebral body end plates which prohibit the passage of nutrients to the intervertebral disk. With the collapse of the disk comes concomitant loss of lordosis (Figure 26-3). Over time, these changes lead to wedging of the vertebral body and cervical kyphosis.
Clinical Case Example
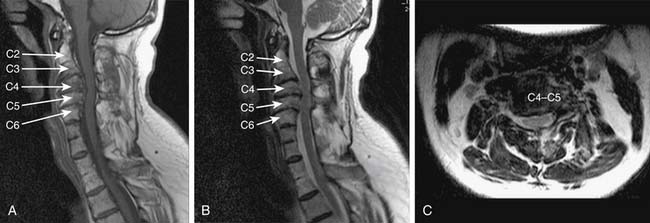
A 45-year-old right-handed man with Klippel-Feil syndrome presented with complaints of neck pain since the age of 12. He had also developed concomitant pain and numbness in the left upper extremity over the course of several years, which was exacerbated by extension of his neck. On clinical examination, the patient was noted to have significantly reduced range of motion in his neck on flexion and extension. Head rotation was limited to 45 degrees on either side of midline. Extension of his neck provoked a feeling of numbness which radiated into the fourth and fifth digits of his left hand. On motor examination, the patient had normal strength in all major muscle groups of the upper and lower extremities bilaterally. Tone was increased in all four limbs. A Hoffman reflex was present in the right hand and plantar responses were down-going bilaterally. He was also noted to have increased reflexes in the upper and lower extremities. Finger-to-nose and heel-to-shin testing were both normal. MR imaging demonstrated segmental kyphosis from C2 to C6 with spinal cord compression secondary to degenerative changes in the cervical spine (Figure 26-1).
Although muscles, ligaments, and intervertebral disks all play vital roles in maintaining proper alignment of the cervical spine, the importance of the bony structures cannot be ignored. The vertebral bodies are composed of cortical and cancellous bone, the latter being most responsible for resisting compressive forces.7 The vascularity of cancellous bone allows for alterations in bone composition consistent with systemic metabolic changes. Osteoporosis is one such degenerative disease which affects cancellous bone in the context of hormonal changes, lack of calcium and vitamin D, and reduced mobility. These factors may induce cellular changes to cancellous bone, causing osteoporosis and predisposing the patient to fractures of the vertebral bodies. Susceptibility to fractures is directly related to the structural changes that occur with osteoporosis.8 In normal bone, the trabeculae are organized in horizontal and vertical planes, which reinforce the strength of the bone. In osteoporotic bone, there is loss of horizontal trabeculae,8 which compromises the strength of bone and predisposes the patient to fractures in the setting of minor force loads. As degenerative changes in the ligaments and intervertebral disks progress, many of the forces are transferred to the vertebral bodies. With osteoporotic changes, the vertebral bodies are unable to provide the same strength against axial loading and wedging or fractures may result. Pathological fractures and wedging of the vertebral bodies are significant contributors to the development and progression of cervical kyphosis.
Cervical Kyphosis and Inflammatory Arthritides
Inflammatory rheumatic disorders are considered uncommon causes of cervical kyphosis. Ankylosing spondylitis affects the entire axial skeleton from sacrum to the cervical spine and is classified as a seronegative arthropathy. Although the exact pathogenesis of ankylosing spondylitis is not well understood, an inflammatory mechanism is postulated, and a large majority of patients will test positive for human leukocyte antigen-B27. Though fewer women than men tend to be affected by ankylosing spondylitis, they will more commonly have disease involving the cervical spine. Clinically, the disease affects synovial and cartilaginous joints. Though the vertebral column is routinely involved, large appendicular joints may also be damaged by synovitis and enthesitis.9 Due to the diffuse inflammatory changes seen with this condition, there is overall stiffening of the vertebral column and structural weakness. These changes affect the spine’s ability to compensate for external loads, and a predisposition for spinal fractures results. Though fractures may occur in any location along the vertebral column, the most common location for a spinal fracture in the setting of ankylosing spondylitis is the lower cervical spine.10 The fractures themselves may lead to kyphosis and neurological sequelae but the more common scenario is that of a chin-on-chest deformity due to severe kyphosis at the cervicothoracic junction.
Rheumatoid arthritis is another inflammatory condition, and generally affects the small joints of the feet, hands, elbows, wrists, hips, knees, ankles, and cervical spine in a variable fashion. There are numerous theories to explain the pathogenesis of rheumatoid arthritis, which are beyond the scope of this review. However, the clinical findings of painful, swollen, erythematous joints are the end result of destruction of synovial joints via the numerous pathways that have been described in the literature. These same inflammatory processes are responsible for facet joint erosion, disk space narrowing, and erosion of the vertebral bodies. As a result of these inflammatory processes, patients with rheumatoid arthritis are predisposed to three types of instability: atlantoaxial subluxation, cranial settling, and subaxial subluxation.11 The combination of cervical instability and predisposition to fractures may make the rheumatoid patient prone to significant kyphotic deformity in the cervical spine.
Management of the Patient with Cervical Kyphosis
Patient Assessment
In the assessment of a patient with cervical degenerative disease, a thorough history and physical examination are crucial. It is important to characterize the type of pain experienced by the patient. Regardless of the nature of the degenerative disease, certain characteristics of pain originating from the cervical spine are associated with favorable surgical outcomes. A patient may complain of midline neck pain and/or radicular pain involving one or both upper limbs. A mechanical nature may be suggested by exacerbation with certain neck movements, coughing, or straining. Stiffness and diskomfort may arise from muscles of the neck, adding a component of musculoskeletal pain difficult to treat through surgery alone. Nonspecific bodily pain is a major contributor to reported functional disability in patients with inflammatory arthritides.12,13 In addition to pain, upper extremity dermatomal numbness may provide clues to symptomatic motion segments. With progressive cervical kyphosis, patients may also complain of forward gaze, dysphagia, or respiratory difficulties.
Cervical myelopathy is another manifestation of degenerative spine disease. In the setting of cervical kyphosis, myelopathy is usually a result of chronic stretch injury and compression to the spinal cord. Patients may describe numbness, clumsiness of the hands, gait unsteadiness, and bowel or bladder difficulties. Physical examination may reveal spasticity, ataxic gait, and the presence of pathologic reflexes such as the Hoffman or Babinski signs. These symptoms are usually insidious in onset and progressive in nature. It is important to note that rheumatoid patients have a high incidence of morbidity and mortality following the onset of myelopathic symptoms.14
Physical examination in the setting of degenerative spine disease and cervical kyphosis is never complete without an assessment of the patient’s overall spinal alignment. Normal alignment of the spine aims to center the head and neck over the shoulder girdle and pelvis. One should also examine the range of motion of the neck. Patients with ankylosing spondylitis may present with severe cervicothoracic kyphosis and marked limitation in range of motion of the neck. These patients will not have correction of the kyphosis while lying in a recumbent position. Patients with rheumatoid arthritis may also demonstrate significant limitation in neck movement due to pain and muscle stiffness. Any anticipated surgical correction must consider preoperative alignment and range of motion not only to establish surgical objectives but to help define realistic outcomes.
Imaging
Studies have addressed normal alignment of the cervical spine,15 but none has provided a standardized definition of what constitutes normal cervical lordosis. Similarly, degree of kyphosis has not yet been systematically correlated with severity of presentation or natural history. As a result, decision making regarding correction of cervical kyphosis is dependent on the underlying degenerative disease and subjective clinical judgment about acceptable or unacceptable decompression and realignment. For example, kyphosis in the setting of rheumatoid arthritis often involves cranio-cervico-thoracic reconstruction whereas in the setting of ankylosing spondylitis, it typically involves segmental subtraction and reconstruction.
Surgical Decision-Making
Traditionally, the surgical management of cervical deformity has been considered primarily where there is evidence of radiographic instability. In their review, White and Panjabi16 describe clinical stability as the ability of the cervical spine to prevent neurological impairment, pain, or gross deformity under physiologic loads. In keeping with this definition, surgical management for cervical kyphosis should be considered where there is evidence of clinical instability as determined by the presence of intractable pain, progressive neurological impairment, or progressive deformity.
Although the criteria for surgical intervention are generally accepted, the timing of surgical intervention is debatable. Where intractable pain and progressive neurological deficits are the predominant symptoms, common-sense principles advocate early surgical intervention. However, in those patients with progressive but otherwise asymptomatic deformity, the picture is less clear. In a small retrospective study17 of thirteen patients, Iwasaki et al. examined predictive factors for the development of cervical kyphosis or myelopathy. The authors concluded that anterior osteophyte formation was representative of posterior ligamentous instability and predictive of progression of cervical kyphosis. In the same study, a ratio below 0.3 of the A-P diameter at the pontomedullary junction relative to the spinal cord diameter at the apex of kyphosis was felt to be predictive of progression of myelopathy. Despite this single study, there are no clear guidelines that serve to facilitate decision making.18 Nonetheless, it is immediately obvious to any spinal surgeon that progressive cervical deformity can ultimately result in severe pain and irreversible neurological compromise. Therefore, common-sense principles dictate that early surgical intervention is warranted in patients with progressive cervical deformity.
The Surgical Approach
Once a patient presents with intractable pain, neurological deficit, or progressive kyphotic deformity, a strategic surgical approach must be chosen. The approach must be such that the symptoms are relieved, cervical alignment is improved, and overall stability is conferred to the cervical spine. An important consideration in surgical decision-making is the presence or absence of a fixed kyphotic deformity. A fixed kyphotic deformity is one in which the deformity does not reduce spontaneously as the patient attempts to extend the neck. This is usually the result of a combination of underlying degenerative changes including vertebral wedging, osteophyte formation, or facet hypertrophy. In contrast, a reducible kyphotic deformity is one in which motion is preserved through the kyphotic segment during flexion and extension. When a fixed kyphotic deformity is present, the surgical approach must accommodate intraoperative reduction of the cervical deformity.19 In this circumstance, anterior osteophytes must be resected and disk spaces released in an attempt to reestablish sagittal alignment.
Once the decision has been made to proceed with surgery, one must decide which surgical approach will be most suitable—anterior, posterior, or both. Several issues deserve consideration as the surgical approach is selected. First and foremost, the goal of surgery is to decompress or otherwise preserve integrity of the underlying nerve roots and spinal cord. Only then does the goal become to reestablish sagittal alignment. However, as mentioned earlier, there is no standardized definition for normal cervical lordosis. An additional principle is that because of the sensitive nature of the spinal cord, anterior pathology should be treated with an anterior approach whereas posterior pathology should be treated via a posterior approach. Steinmetz et al.18 have proposed an algorithm for management of cervical kyphosis that considers each of these factors (Figure 26-4).
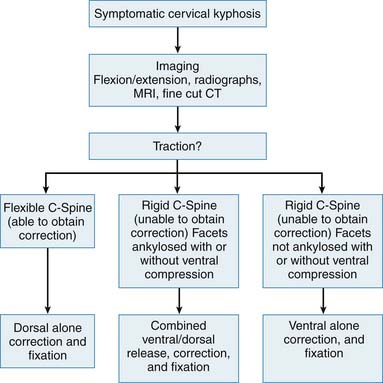
FIGURE 26-4 Treatment algorithm for correction of cervical deformity.
(Adapted from Steinmetz MP et al: Cervical deformity correction, Neurosurgery Suppl 60(1):S1-90-97, 2007.)
With this in mind, it is our experience that the majority of patients with cervical kyphosis can be managed through an anterior approach alone. This allows for superior correction of the deformity under distraction, is better tolerated by the patient, and does not violate the posterior tension band of the cervical spine. Also, if radicular pain is a major component of the patient’s symptomatology, an anterior approach allows for superior decompression of the cervical nerve roots. Finally and inarguably, it allows reconstruction of a failed anterior column through provision of additional anterior column support. Given the success of multilevel fusion with anterior approaches, the surgeon should not hesitate to perform multilevel diskectomies or, if necessary, corpectomies in order to ensure adequate decompression and alignment. If, due to the presence of severe kyphosis, a posterior approach is deemed necessary, this can often be combined with an anterior approach to ensure maximal decompression and fixation at the involved levels. Isolated posterior fixation is reserved for exceptional circumstances where a patient’s physical stature limits access to the anterior cervical spine.
Surgical Complications
Clinical Case Example
TREATMENT AND CLINICAL CHALLENGES
In our case, the patient has presented with progressive symptoms of neck pain, numbness involving the left upper extremity and early signs of myelopathy. On MR imaging, abnormalities in sagittal alignment are immediately evident (see Figure 26-1). Reversal of cervical lordosis can be seen in the subaxial cervical spine with a kyphotic deformity from C3 to C5. Compression of the cervical spinal cord is associated with this, accounting for the patient’s myelopathy. Fused segments can be appreciated at C2-C3, C7-T1, and T2-T3, consistent with a preexisting diagnosis of Klippel-Feil syndrome. Degenerative disk disease involving C2-C3, C3-C4, and C4-C5 is also noted. On axial imaging, left-sided foraminal stenosis is seen at the C3-C4 and C4-C5 levels. Given this patient’s neurological deficits and radiological evidence of kyphosis, the patient was advised to undergo surgical intervention.
The first objective of surgery was to ensure adequate decompression of the spinal cord. MR sequences show the bulk of the stenosis to be located through the kyphosis at C3 to C5. Thus the overall surgical strategy had to permit correction of sagittal alignment as well as relief of nerve root and spinal cord compression. With these goals in mind, the patient was taken to the operating room and an anterior approach was undertaken. Extensive tissue dissection allowed for adequate exposure of C2 to C7, and distraction was applied through pins in the bodies of C3 and C6 respectively. Diskectomies were performed at the C3-C4, C4-C5, and C5-C6 levels and distraction tightened. Decompression of the nerve roots was obtained by ensuring exposure to the uncovertebral processes and removal of excess disk material laterally. Once decompression was complete, corpectomies were performed at the C4 and C5 levels by drilling away bone between the diskectomy sites. Thereafter, a single iliac crest graft was taken (measured under distraction) to reestablish anterior column support. Instrumentation was performed from C3 through C6 (Figure 26-5).
Conclusions/Diskussion
In the management of cervical kyphosis, the clinical symptomatology of the patient and the nature of the kyphotic deformity must be considered. Surgical management is appropriate in the setting of intractable pain, neurological compromise, and progressive kyphotic deformity. Unfortunately, robust physiological studies do not exist, and therefore normal sagittal alignment of the cervical spine is not well defined. However, for the surgeon to provide adequate decompression of neural tissues, the underlying kyphotic deformity must be addressed through decompression followed by reconstruction. The exact surgical approach is dependent on the nature of the pathology and one’s ability to use nonsurgical adjuncts such as traction to help realign the cervical spine, but almost invariably involves a primary anterior approach.
1. Shi R., Pryor J.D. Pathological changes of isolated spinal cord axons in response to mechanical stretch. Neuroscience. 2002;110:765-777.
2. Baptiste D.C., Fehlings M.G. Pathophysiology of cervical myelopathy. Spine J.. 2006;6:190S-197S.
3. Yoganandan N., Kumaresan S., Pintar F. Biomechanics of the cervical spine part 2: cervical spine soft tissue responses and biomechanical modeling. Clin. Biomech.. 2001;16:1-27.
4. Panjabi M., Goel V.K. Takata K: Physiologic strains in the lumbar spine ligaments: in vitro biomechanical study. Spine. 1982;7:192-203.
5. Bogduk N., Mercer S. Biomechanics of the cervical spine part 1: normal kinematics. Clin Biomech.. 2000;15:633-648.
6. Aebi M., editor. Aging spine. Heidelberg: Springer-Verlag, 2005.
7. Silva M.J., Keaveny T.M., Hayes W.C. Load sharing between the shell and the centrum in the lumbar vertebral body. Spine. 1997;22:140-150.
8. Einhorn T.A. Bone strength: the bottom line. Calcif. Tissue Int.. 1992;51:333-339.
9. Borenstein D. Inflammatory arthritides of the spine. Clin. Orthop. Relat. R. 2006;443:208-221.
10. Broom M.J., Raycroft J.F. Complications of fractures of the cervical spine in ankylosing spondylitis. Spine. 1988;13:763-766.
11. Shen F.H., et al. Rheumatoid arthritis: evaluation and surgical management of the cervical spine. Spine J.. 2004;4:689-700.
12. Ward M. Quality of life in patients with ankylosing spondylitis. Rheum Dis. Clin. North Am.. 1998;Nov 24(4):815-827.
13. Reinster J.Y. The prevalence and burden of arthritis. Rheumatology. 2002;41(suppl.1):3-6.
14. Reiter M. S. Boden: Inflammatory disorders of the cervical spine. Spine. 1998;23(24):2755-2766.
15. Hardacker J.W., et al. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine. 1997;22(13):1472-1479.
16. White A., Panjabi M. The role of stabilization in the treatment of cervical spine injuries. Spine. 1984;9:512-522.
17. Iwasaki M., et al. Cervical kyphosis: predictive factors for progression of kyphosis and myelopathy. Spine. 2002;27(13):1419-1425.
18. Steinmetz M.P., et al. Cervical deformity correction. Neurosurgery. 60(1), 2007. S1-90-97
19. O’Shaughnessy, et al. Surgical treatment of fixed cervical kyphosis with myelopathy. Spine. 2008;33(7):771-778.