Chapter 94 Cervical Facet Dislocations
A Ventral Surgical Strategy for Decompression, Reduction, and Stabilization
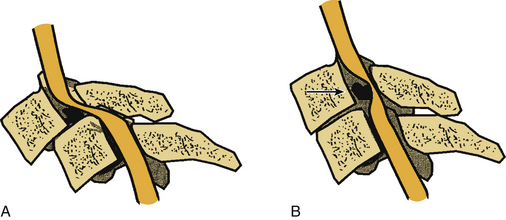
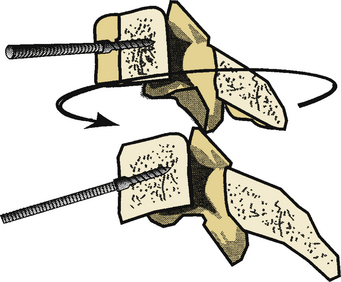
Much controversy surrounds the management of subaxial cervical subluxations resulting from facet fracture-dislocation.1–11 An initial attempt at closed reduction using skeletal traction is not without risk.12–18 The most serious complication of cervical traction and closed reduction is the retropulsion of disc fragments into the spinal canal and resultant spinal cord compression (Fig. 94-1). Several reports of neurologic deterioration after closed reduction in the setting of concurrent disc herniation have been described.19–23 In addition, late instability is relatively common in patients treated with closed reduction alone, because of the concomitant presence of significant ligamentous disruption associated with these injuries.
The surgical technique for the open reduction of unstable cervical dislocations varies from surgeon to surgeon. Most reports have described dorsal reduction techniques.20,21,24–29 However, the ventral surgical approach for reduction has its advocates.30 Several small series have been published that describe the technique of ventral reduction of locked facets.19,31–35 Because of the popularization of dorsal fixation techniques (e.g., lateral mass plating and spinous process wiring), ventral reduction has not been widely used in clinical practice. However, an increasing concern has been raised regarding the danger associated with the dorsal reduction of a cervical spine dislocation in the presence of a ventral disc herniation.19,21–24 Furthermore, because of the common coexistence of significant dorsal bony and soft tissue disruption, a three-vertebral segment (two-motion segment) dorsal fixation is commonly required to stabilize a two-vertebral segment (one-motion segment) instability. In addition, in dorsal reduction of locked facets, it is commonly necessary to remove a significant portion of the involved facet(s), thus often mandating a three-vertebral segment dorsal fixation procedure. Conversely, ventral reduction may be followed by arthrodesis of only a single-motion segment, thus sparing additional motion segments from arthrodesis.
Kwon et al.36 concluded that both ventral stabilization and dorsal stabilization for unilateral cervical facet injuries were valid treatment options. In this randomized study of 42 patients with unilateral cervical facet injuries, patients on whom a ventral approach was used had a lower rate of wound infection, had a higher rate of radiographically demonstrated union, and healed in a more lordotic sagittal alignment. However, they also more frequently had signs of dysphagia and voice changes in the early postoperative period in comparison to the group treated with dorsal stabilization. Patients undergoing a ventral approach should be informed of these (and all other) risks.
Surgical Technique
Discectomy
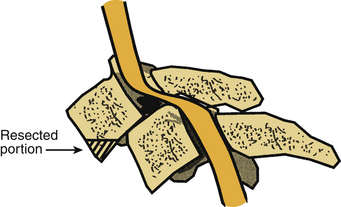
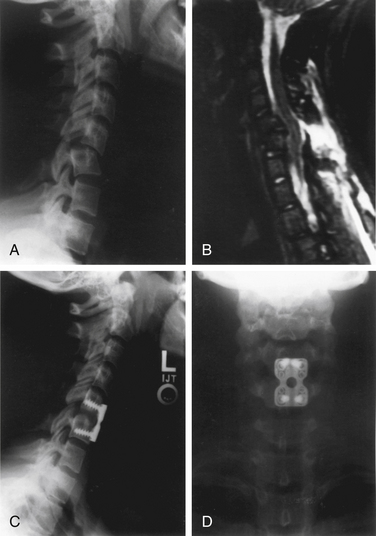
The standard ventromedial approach is used through a transverse skin incision. After radiographic confirmation of the operative level, a discectomy is performed. A special consideration in the case of facet dislocation is the ventral translation (ventrolisthesis) of the rostral vertebral body on its caudal counterpart. This is often associated with some degree of kyphotic angulation and a resultant obscuration of the disc space, necessitating removal of the ventral aspect of the caudal end plate of the rostral vertebral body with a high-speed air drill (Fig. 94-2). Care must be taken not to remove so much of the vertebral body as to preclude ventral screw-plate fixation. After exposure of the disc space, a standard discectomy is performed. The posterior longitudinal ligament is always removed, thus exposing the dura mater and ensuring adequate decompression.
Reduction
Interbody Spreader Technique
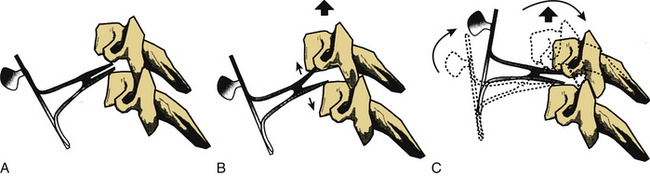
A Cloward interbody spreader, or an equivalent device, is inserted into the disc interspace at a 30- to 40-degree angle (Fig. 94-3A). Failure to place this device at an angle results in achieving only distraction force application (as simple distraction with tongs achieves). This does not result in the application of a bending moment, which is required for reduction with this technique.
While distraction is gradually applied with the disc interspace spreader (applied in the midvertebral body region) (Fig. 94-3B), the spreader is rotated rostrally. This applies a bending moment to the dislocated vertebral body while the facet dislocation is reduced by distraction. If the locked facets are disengaged, the vertebrae should realign. Distraction is then relaxed in the aligned position, and the spreader is removed (Fig. 94-3C).
Vertebral Body Post Technique
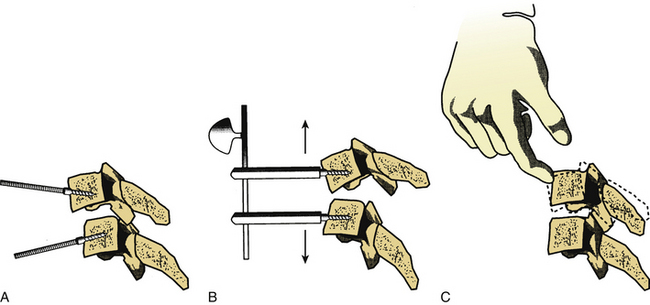
The vertebral body post technique usually involves placing the posts at an angle with respect to each other (Fig. 94-4A). This facilitates the application of a bending moment that unlocks the facets before the application of distraction forces (Fig. 94-4B). Distraction should then allow for complete disengagement of the locked facets. Manual reduction via the placement of the dorsally directed pressure on the rostral vertebral body encourages reduction if the facets have been adequately disengaged (Fig. 94-4C). Relaxation of the distraction forces then allows reengagement of the facets in a normal position. The placement of dorsally directed pressure on the rostral vertebral body, as described previously, may also be applied with the interbody spreader technique.
As an aside, unilateral facet dislocation reduction through a ventral approach may be achieved in a similar manner with the application of torque about the long axis of the spine, thus facilitating the reduction of the rotatory component of the deformity (Fig. 94-5). This tends to reduce the rotational component of the dislocation.
Ventral Decompression before Reduction
The incidence of extruded cervical disc herniation associated with cervical spine injury has been reported to be 0.7% to 42%.19–21,23,37 Reduction of the dislocation with the potential for retropulsion of disc material into the reduced and realigned spinal canal may result in significant spinal cord encroachment.
Several authors have recommended a ventral decompression before reduction when they suspect the potential for reduction-induced spinal cord encroachment.19–21,23,38 This relatively uncommon event may occur with either open or closed reduction strategies and is avoided by the removal of the potentially offending disc before reduction (see Fig. 94-1). Although magnetic resonance imaging (MRI) is useful in predicting this event, it probably is not universally accurate. In fact, MRI may demonstrate the absence of intracanalicular disc fragments. Nevertheless, disc material could be retropulsed through a disrupted anulus into the spinal canal during reduction.20
Reduction Feasibility
Previous reports have addressed the ventral reduction of cervical spine dislocations.18,19,31–34 The only relatively large series of ventral reductions of locked facets was by de Oliviera,32 who reported ventral reduction in 15 cases. He reported no failure with this interbody spreader technique. An understanding of the case-specific anatomy and fundamental biomechanical principles allows ventral reduction to be much more successful than was generally thought. The key is facet joint disengagement before an attempt at reduction. This requires the application of a bending moment to the unstable motion segment, followed by distraction, reduction, and finally relaxation of the distraction.
Failure of Ventral Reduction
The failure of attempts at ventral deformity reduction is a reality. Therefore, it behooves the spine surgeon to appropriately counsel the patient and family preoperatively regarding the possible need for a combined ventral and dorsal (and possibly an additional ventral) approach. Although the latter might seem to be an excessive amount of surgical intervention, it provides the greatest chance for preservation and improvement of neurologic function. Significant comminution of the facets appears to be a risk factor for failure of ventral reduction. Therefore, in patients with this risk factor, consideration should be given to a dorsal reduction and arthrodesis if a disc herniation is not present.
Stability Acquisition Using a Ventral Approach
Some authors have addressed the concern for stability acquisition in the circumferentially unstable spine (severe three-column injury)39 via an isolated ventral approach.40 Most of these concerns have been directed at dislocations involving two or more motion segments (one or more vertebral body fractures) or after the use of dynamic fixation systems (nonfixed moment arms). However, with one-motion segment circumferential instability, the short bending moment applied by the implant (short implant) by way of the spine allows for greater stability acquisition potential.
Summary
A ventral approach to cervical dislocation and instability may be appropriate in more cases than was previously thought. The ventral approach facilitates (1) ventral decompression before reduction (thus minimizing the chance for iatrogenic neurologic injury), (2) single-motion segment fixation (in contrast to two-motion segment fixation using a dorsal approach), and (3) stability acquisition through the application of effective ventral fixation techniques (Fig. 94-6).
Benzel E., Kesterson L. Posterior cervical interspinous compression wiring and fusion for mid to low cervical spinal injuries. J Neurosurg. 1989;70:893-899.
Eismont F.J., Arena M.J., Green B.A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. J Bone Joint Surg [Am]. 1991;73:1555-1560.
Hadley M.N., Fitzpatrick B.C., Sonntag V.K.H., Browner C.M. Facet fracture dislocation injuries of the cervical spine. Neurosurgery. 1992;30:661-666.
Kwon B.K., Fisher C.G., Boyd M.C., et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
Ordonez B.J., Benzel E.C., Naderi S., Weller S.J. Cervical facet dislocation: techniques for ventral reduction and stabilization. J Neurosurg. 2000;92(Suppl 1):18-23.
1. Argenson C., Lovet J., Sanouiller J.L., de Peretti F. Traumatic rotatory displacement of the lower cervical spine. Spine (Phila Pa 1976). 1988;13:767-773.
2. Benzel E., Kesterson L. Posterior cervical interspinous compression wiring and fusion for mid to low cervical spinal injuries. J Neurosurg. 1989;70:893-899.
3. Braakman R., Vinken P.J. Old luxations of the lower cervical spine. J Bone Joint Surg [Br]. 1968;50:52-60.
4. Cotler H.B., Miller L.S., DeLucia F.A., et al. Closed reduction of cervical spine dislocations. Clin Orthop. 1987;214:185-199.
5. Evans D.K. Reduction of cervical dislocations. J Bone Joint Surg [Br]. 1961;43:552-555.
6. Kleyn P.J. Dislocations of the cervical spine: closed reduction under anaesthesia. Paraplegia. 22, 1984. 271–228
7. Osti O.L., Fraser R.D., Griffiths E.R. Reduction and stabilization of cervical dislocation. J Bone Joint Surg [Br]. 1989;71:275-282.
8. Perin N., Cooper P.R. Posterior stabilization of the cervical spine using plates and screws. In: Garfin S.R., Bruce F., Northrup B.F., editors. Surgery for spinal cord injuries. New York: Lippincott-Raven; 1993:113-122.
9. Sabiston C.P., Wing P.C., Schweigel J.F., et al. Closed reduction of dislocations of the lower cervical spine. J Trauma. 1988;28:832-835.
10. Shrosbree R.D. Neurological sequelae of reduction of fracture dislocations of the cervical spine. Paraplegia. 1979;17:212-221.
11. Stauffer E.S., Kelly E.G. Fracture-dislocations of the cervical spine. J Bone Joint Surg [Am]. 1977;59:45-48.
12. Alexander E.J., Davis C.T., Forsyth H.F. Reduction and fusion of fracture dislocation of the cervical spine. J Neurosurg. 1967;27:588-591.
13. Cloward R.B. Reduction of traumatic dislocation of the cervical spine with locked facets. Technical note. J Neurosurg. 1973;38:527-531.
14. Hadley M.N., Fitzpatrick B.C., Sonntag V.K.H., Browner C.M. Facet fracture dislocation injuries of the cervical spine. Neurosurgery. 1992;30:661-666.
15. Maiman D.J., Banolat G., Larson S.J. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1982;11:471-476.
16. Sonntag V.K.H. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1981;8:150-152.
17. Star A.M., Jones A.A., Cotler J.M., et al. Immediate closed reduction of cervical spine dislocations using traction. Spine (Phila Pa 1976). 1990;15:1068-1072.
18. Wolf A., Levi L., Mirvis S., et al. Operative management of bilateral facet dislocation. J Neurosurg. 1991;75:883-890.
19. Berrington N.R., van Staden J.F., Willers J.G., van der Westhuizen J. Cervical intervertebral disc prolapse associated with traumatic facet dislocations. Surg Neurol. 1993;40:395-399.
20. Doran S.E., Papadopulos S.M., Ducker T.B., Lillehei K.O. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79:341-345.
21. Eismont F.J., Arena M.J., Green B.A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. J Bone Joint Surg [Am]. 1991;73:1555-1560.
22. Robertson P.A., Ryan M.D. Neurological deterioration after reduction of cervical subluxation: mechanical compression by disc tissue. J Bone Joint Surg [Br]. 1992;74:224-227.
23. Tribus C.B. Cervical disk herniation in association with traumatic facet dislocation. Tech Orthop. 1994;9:5-7.
24. Beyer C., Cabanela M., Berquist T. Unilateral facet dislocations and fracture dislocations of the cervical spine. J Bone Joint Surg [Br]. 1991;73:977-981.
25. Bohlman H.H. Acute fractures and dislocations of the cervical spine. J Bone Joint Surg [Am]. 1979;61:1119-1142.
26. Cooper P.R., Cohen A., Rosiello A., Koslow M. Posterior stabilization of cervical spine fractures and subluxations using plates and screws. Neurosurgery. 1988;23:300-306.
27. Rorabeck C., Rock M., Hawkins R., Bourne R. Unilateral facet dislocation of the cervical spine: an analysis of the result of treatment in 26 patients. Spine (Phila Pa 1976). 1987;12:23-27.
28. Schwarz N. Die verhakte Rotationssubluxation der Halswirbelsäule. Unfallchirurg. 1992;95:367-374.
29. Shapiro S.A. Management of unilateral locked facet of the cervical spine. Neurosurgery. 1993;33:832-837.
30. Ordonez B.J., Benzel E.C., Naderi S., Weller S.J. Cervical facet dislocation: techniques for ventral reduction and stabilization. J Neurosurg. 2000;92(Suppl 1):18-23.
31. Cloward R.B. Treatment of acute fractures and fracture-dislocations of the cervical spine by vertebra-body fusion. A report of eleven cases. J Neurosurg. 1961;18:201-209.
32. de Oliviera J.C. Anterior reduction of interlocking facets in the lower cervical spine. Spine (Phila Pa 1976). 1979;4:195-202.
33. Kostuik J.P., Connolly P.J. Anterior cervical plate fixation. In: Garfin S.R., Northrup B.F., editors. Surgery for the spinal cord injuries. New York: Lippincott-Raven; 1993:163-173.
34. Rengachary S.S., Duke D.A. Stabilization of the cervical spine with the locking plate system. In: Hitchon P.W., Traynelis V.C., Rengachary S.S., editors. Techniques in spinal fusion and stabilization. New York: Thieme; 1995:176-190.
35. Verbiest H. Anterior operative approach in cases of spinal cord compression by old irreducible displacement or fresh fracture of cervical spine. J Neurosurg. 1962;19:389-400.
36. Kwon B.K., Fisher C.G., Boyd M.C., et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7:1-12.
37. Rizzolo S.J., Piazza M.R., Cotler J.M., et al. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976). 1991;16(Suppl 6):187-189.
38. Olerud C., Jonsson H.Jr. Compression of the cervical spine cord after reduction of fracture dislocations. Acta Orthop Scand. 1991;62:599-601.
39. Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop. 1984;189:65-70.
40. Caspar W., Barbier D.D., Klara P.M. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491-502.