Chapter 8 CEREBROSPINAL FLUID EVALUATION
General Discussion
The mean opening lumbar CSF pressure is variable, depending on the age of the child. These pressures are outlined in Table 8-1. Opening pressures may exceed 150 to 200 mm H20 when bacterial meningitis is present.
| WBC Count | Mean % PMNs | |
|---|---|---|
| Preterm | 0-25 WBCs/mm3 | 57% |
| Term | 0-22 WBCs/mm3 | 61% |
| Child | 0-7 WBCs/mm3 | 5% |
| Glucose | ||
| Preterm | 24-63 mg/dL | 1.3-3.5 mmol/L |
| Term | 34-119 mg/dL | 1.9-6.6 mmol/L |
| Child | 40-80 mg/dL | 2.2-4.4 mmol/L |
| CSF Glucose/Blood Glucose | ||
| Preterm | 55%-105% | |
| Term | 44%-128% | |
| Child | 50% | |
| Lactic Acid Dehydrogenase | ||
| Normal range | 5-30 U/L (or about 10% of serum value) | |
| Myelin Basic Protein | <4 ng/mL | |
| Opening Pressure | ||
| (Lateral recumbent) | ||
| Newborn | 8-11 cmH2O | |
| Infant/Child | <20 cmH2O | |
| Respiratory Variations | 0.5-1 cmH2O | |
| Protein | ||
| Preterm | 65-150 mg/dL | 0.65-1.5 g/L |
| Term | 20-170 mg/dL | 0.20-1.7 g/L |
| Child | 5-40 mg/dL | 0.05-0.40 g/L |
CSF, cerebrospinal fluid; PMNs, polymorphonuclear lymphocytes; WBC, white blood cell.
Modified from Oski FA: Principles and Practice of Pediatrics, 3rd ed. Philadelphia: JB Lippincott, 1999 insert page number(s).
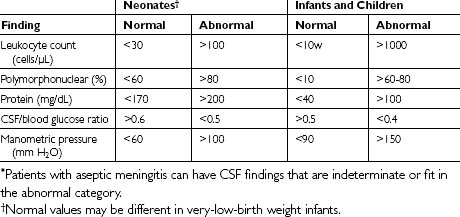
Examination of the cerebrospinal fluid of a patient with acute bacterial meningitis characteristically reveals the following: (1) a cloudy appearance, (2) an increased WBC count with a polymorphonuclear predominance, (3) a low glucose concentration in relation to the serum glucose concentration, (4) an elevated protein concentration, (5) a smear and culture positive for the causative microorganism, and (6) a high monometric pressure. Table 8-2 shows the CSF findings in patients with bacterial meningitis.
Table 8-2 Normal and Characteristic Abnormal Cerebrospinal (CSF) Findings in Pediatric Age Groups with or without Bacterial Meningitis*
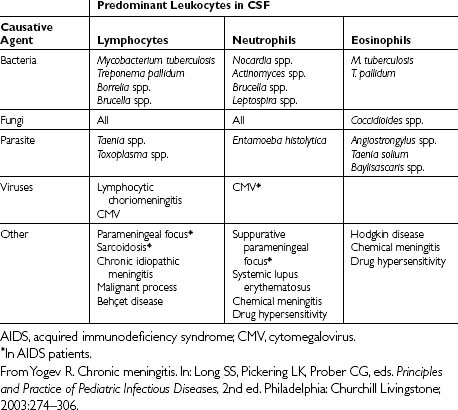
Most infectious causes of chronic meningitis elicit similar CSF abnormalities: a mildly elevated protein concentration, a normal glucose level, and fewer than 500 WBCs/mm3 with lymphocyte predominance. Table 8-3 outlines distinctive patterns of leukocyte predominance that may aid diagnosis.
Suggested Work-up
| CSF evaluation: |
Additional Work-up
| CSF opening pressure | See preceding text |
| CSF latex agglutination | See preceding text |
| CSF PCR: |
1. Prober C.G. Central nervous system infections. In: Behrman R.E., Kliegman R.M., Jenson H.B., editors. Nelson Textbook of Pediatrics. 17th ed. Philadelphia: WB Saunders; 2004:1980–1981.
2. Robertson J., Shilkofski N., editors. Johns Hopkins: The Harriet Lane Handbook: A Manual for Pediatric House Officers, 17th ed., Philadelphia: Mosby, 2005.
3. Sáez-Llorens X., McCracken G.H. Meningitis. In: Gershon A.A., Hotez P.J., Katz S.L., editors. Krugman’s Infectious Diseases of Children. 11th ed. Philadelphia: Mosby; 2004:377-379. 864–8
4. Seehusen D.A., Reeves M.M., Fomin D.A. Cerebrospinal fluid analysis. Am Fam Physician. 2003;68:1103–1108.
5. Yogev R. Chronic meningitis. In: Long S.S., Pickering L.K., Prober C.G., editors. Principlesand Practice of Pediatric Infectious Disease. 2nd ed. Philadelphia: Churchill Livingstone; 2003:274–306.