Chapter 38 Cerebellopontine Angle Tumors
• Comprehensive knowledge of the complex anatomy of the cerebellopontine (CP) angle is a prerequisite for achieving good surgical results. The crucial neurovascular structures should be identified as early as possible during surgery, which enables their preservation and guides subsequent operative steps. Whatever the tumor size and extension, the anatomical relationships of the cranial nerves in the area of the fundus of the internal auditory canal and in the brainstem exit/entry zone are constant.
• Most of the CP angle tumors are benign and their complete removal leads to excellent long-term outcomes. The only exception to complete tumor removal is the attempt to preserve function, such as in surgery for vestibular schwannoma in the only hearing ear.
• The major principles of CP angle tumor removal include the following: important neural structures, such as the cochlear and facial nerves, should be identified early; the tumor should be initially debulked; the dissection from the surrounding structures should be performed only after sufficient internal decompression is achieved; the dissection should always be performed in the arachnoid plane; bipolar coagulation, especially in the vicinity of a cranial nerve, should be avoided.
• Our preferred approach is the retrosigmoid approach. It is safe, relatively simple, and provides a panoramic view of the CP angle and petroclival area. Importantly, it is related to a very low procedure-related morbidity rate. The additional removal of the suprameatal tubercle provides access to tumors with extensions into Meckel’s cave, into the petroclival area, and even into the posterior cavernous sinus.
History of Cerebellopontine Angle Surgery
Tumors of the cerebellopontine (CP) angle are usually benign and their complete removal leads to the healing of the patient. However, because of the very complex anatomical structure of the area and the severity of the neurological dysfunction in case of iatrogenic damage, surgery in the CP angle has always been a challenge. The first successful complete removal of a CP angle tumor was performed in 1894 by Sir Charles Balance. The tumor was approached via a right posterior fossa craniectomy and removed with the finger inserted in an unsterile fashion between the pons and the tumor. Although the patient had facial anesthesia and complete facial palsy, he recovered from surgery and was alive for at least 18 years.1 The pathological nature of this tumor is a matter of controversy and the credit for the first removal of a vestibular schwannoma (VS) probably belongs to Thomas Annandale of Edinburgh. In 1895 he removed a tumor “the size of a pigeon’s egg” via a unilateral suboccipital craniotomy. Later, major contributions to the surgery of CP angle tumors were made by V. Horsley, von Eiselsberg, and F. Krause. Krause used for the first time faradic stimulation to differentiate the facial from the audiovestibular nerve.2 H. Cushing was the first to reduce the complication and mortality rates of VS surgery to an acceptable level by performing intracapsular tumor removal. Expectedly, the tumor recurrence rate in his series was very high. W. Dandy introduced the currently widely accepted concept of VS management. He argued that benign tumors should be removed completely in order to prevent recurrence at a later stage, even at the expense of a somewhat higher perioperative mortality rate. In the following decades, morbidity and mortality rates progressively improved with increased experience and knowledge of the normal and pathological anatomy of the CP angle, earlier detection of such tumors with the introduction of computed tomography (CT) and magnetic resonance imaging (MRI), routine use of intraoperative electrophysiological monitoring, and more reliable and safe anesthetic and operative techniques. Initial efforts at preservation of facial nerve function have expanded to preservation of hearing with increasing success. As a result of these efforts, modern CP angle surgery has been refined to a routine, safe, and low morbidity procedure.
Cerebellopontine Angle Anatomy
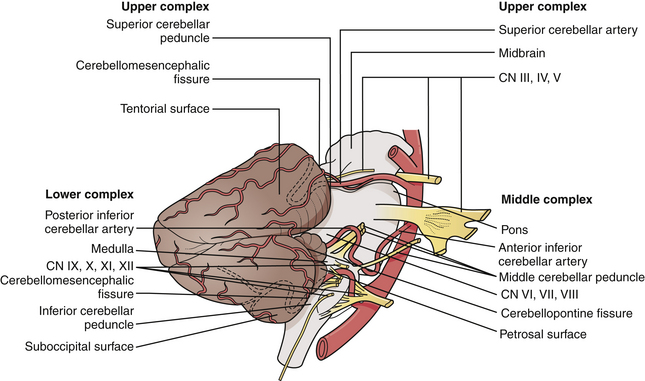
The CP angle is a triangular space located posterior to the pyramid, inferior to the tentorium, lateral to the pons, and ventral to the cerebellum.3 It is defined by the superior and inferior limbs of the CP fissure (Fig. 38.1).
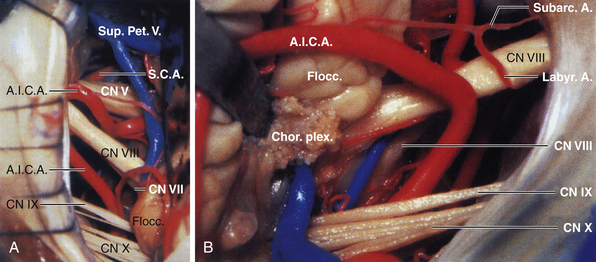
The CP angle cistern is located between the anterolateral surface of the pons and cerebellum and the posterior surface of the petrous bone and contains the trigeminal, abducent, facial, and vestibulocochlear nerves, the superior cerebellar and anterior inferior cerebellar arteries, a variable number of draining veins, the flocculus of the cerebellum, and the choroid plexus that protrudes through the foramen of Luschka. The facial nerve exits from the brainstem in the lateral part of the pontomedullary sulcus, 1 to 2 mm anterior to the entry zone of the vestibulocochlear nerve. The ninth, tenth, and eleventh cranial nerves are located in the lower part of the CP angle (Fig. 38.2A and B).
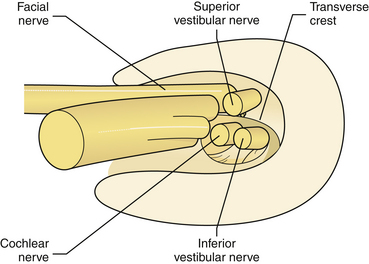
Five nerves pass through the internal auditory canal (IAC): the facial, the vestibular (superior and inferior), the cochlear, and the nervus intermedius, accompanied by the labyrinthine artery and occasionally by branches of the anterior inferior cerebellar artery (AICA) or a loop of the AICA itself.4
In the area of the fundus of the IAC, the nerves have constant location: the facial nerve occupies the anterosuperior quadrant, the cochlear nerve occupies the anteroinferior quadrant, the superior vestibular nerve is in the posterosuperior quadrant, and the inferior vestibular nerve is in the posteroinferior quadrant (Fig. 38.3). Knowledge of these anatomical relationships is of utmost importance for the surgeon because early identification of the main neurovascular structures is a prerequisite for their preservation.
Tumors of the Cerebellopontine Angle
Tumors of the CP angle account for 5% to 10% of all intracranial neoplasms.5 VSs are the most common CP angle tumor and account for 80% to 94% of them, followed by meningiomas (3-10% of CP angle tumors) and the epidermoids (2-4%). Much rarer primary tumors are schwannomas of other cranial nerves: of the trigeminal nerve, of the facial nerve, or of the caudal cranial nerves; paragangliomas, chordomas, chordosarcomas, arachnoid or neurenteric cysts, dermoid tumors, and metastases.6,7 The CP angle could be secondarily involved by tumors extending from the brainstem or fourth ventricle: gliomas, ependymomas, choroid plexus papillomas, medulloblastomas, or lymphomas. Bilateral CP angle tumors are characteristic for neurofibromatosis 2 (NF2) and are typically VSs. Rare bilateral tumors not associated with NF2 are facial nerve schwannomas, plexus papillomas, endolymphatic sac tumors, metastases, or osteomas.8
Imaging
The precise radiological diagnosis of CP angle tumors requires a systematic approach and analysis of the lesions: site of origin, location, shape and margins, density, signal intensity, and contrast enhancement characteristics.6,9 The enhancing CP angle tumors are most frequently vestibular and nonvestibular schwannomas, meningiomas, metastases and paragangliomas, chondrosarcomas, and chordomas.7 Nonenhancing extra-axial CP angle lesions may be cystic, such as the epidermoid cysts, the arachnoid cysts, and the neurenteric cyst or may contain fat (dermoid cyst, lipoma). Intrinsic brain tumors with a significant exophytic extension into the CP angle (lymphoma, hemangioblastoma, choroid plexus papilloma, ependymoma, glioma, medulloblastoma, dysembryoplastic neuroepithelial tumor) may be difficult to differentiate from an extra-axial lesion based only on their radiological characteristics.6
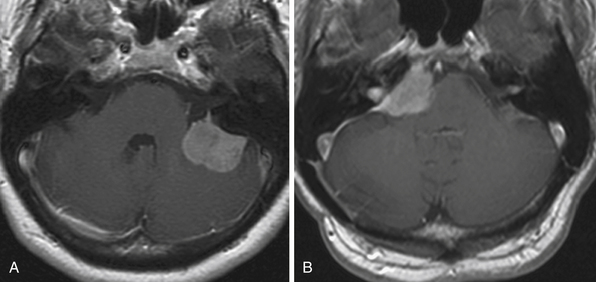
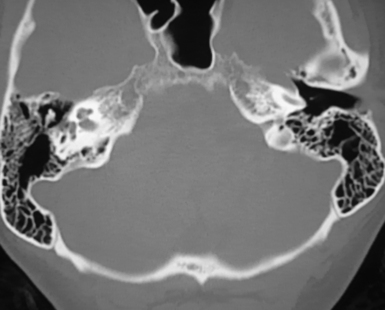
Bone window thin slice CT shows the bony changes of the pyramid and of the IAC and is essential for surgical planning. Erosion or dilatation of the IAC is seen in 70% to 90% of the patients with VS. Nevertheless, the diagnostic tool of choice for all CP angle tumors is MRI.7,10,11 On T1-weighted sequences VSs are isointense to slightly hypointense and on T2-weighted sequences they are hyperintense. They enhance intensely and homogeneously after contrast application, with the exception of cystic portions of the tumors. Intrameatal VSs are best visualized with gadolinium enhancement. Meningiomas are most frequently isointense to slightly hypointense to brain parenchyma on T1-weighted MRI studies. On T2-weighted MRI studies they have higher intensity than that of VS and show a homogeneous contrast enhancement. The radiological differential diagnosis between VS and CP angle meningioma is based on several criteria. Meningiomas are centered usually away from the IAC and have broad contact with the petrous bone or the tentorium (Fig. 38.4A and B). The angle between the tumor and the pyramid is obtuse. The IAC is not widened and the tumor very rarely extends into the IAC. Although secondary invasion of the IAC might be observed in 10% to 20%,12 primarily IAC meningiomas are exceedingly rare.6,13 Calcification and cystic changes are frequent findings. A tail of enhancement along the dura (the dural “tail” sign), although not pathognomonic, is visible in 60% to 72% of meningiomas. VSs are centered at the widened IAC. They form an acute angle with the posterior surface of the petrous bone and almost always extend into the IAC (Fig. 38.5). In VS, calcifications are extremely rarely found.
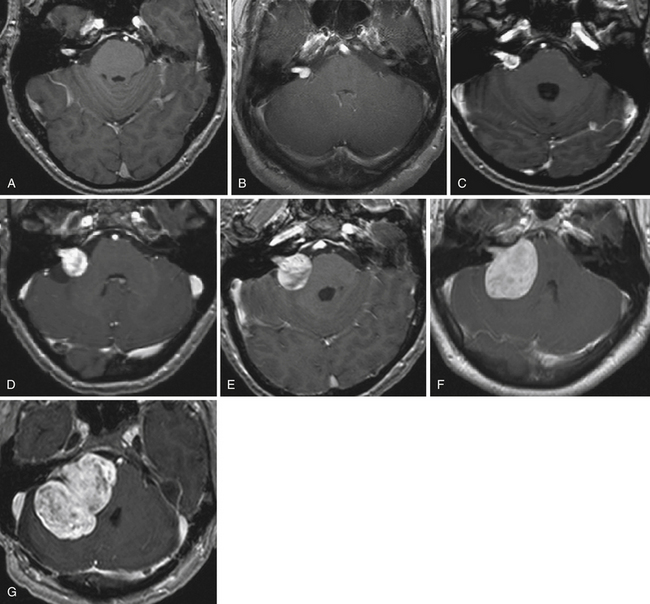
FIGURE 38.5 A to G, Stages of vestibular schwannoma growth: from grade T1 to grade T5 (T1-weighted contrast-enhanced coronal images). A, Grade T1, purely intrameatal. B, Grade T2, intraextrameatal. C, Grade T3a, filling the CPA cistern. D, Grade T3b, reaching the brainstem. E, Grade T4a, compressing the brainstem. F, Grade T4b, severe compression and dislocation of the brainstem and fourth ventricle. G, Grade T5, giant tumors with extension over the midline. See Table 38.2 for corresponding classification.
Epidermoids are hypodense on CT and in up to 25% rim calcification is observed. On T1- and T2-weighted MRI they are usually isointense to cerebrospinal fluid (CSF).6,11 The signal intensity is related to the contents of the cyst: if cholesterol predominates, the cysts are hyperintense on T1-weighted images and hypointense on T2-weighted images. Fluid-attenuated inversion recovery imaging, diffusion-weighted imaging, and CISS spin-echo MRIs are more precise imaging modalities. Because of their similar characteristics it might be difficult to differentiate epidermoid cysts from arachnoid cysts. Two of the main differences between them are the smaller mass effect caused by the arachnoid cysts and their more homogeneous signal intensity on T2-weighted images.
Surgical Approaches to the Cerebellopontine Angle
The approaches to the CP angle are either posterior (through the posterior cranial fossa) or lateral (through the petrous bone). The most popular approach is retrosigmoid suboccipital, introduced by Fedor Krause (1903) and later modified and refined by many surgeons.14 The lateral approaches involve removal of a part of the petrous bone either via a subtemporal route (e.g., the middle fossa approach, the extended middle fossa approach, or the Kawase approach) or via the mastoid (the presigmoid approach, the retrolabyrinthine petrosectomy, the translabyrinthine approach (Rudolf Panse, 1904), and the transcochlear approach).4,14
Several factors have to be considered when selecting the surgical approach: tumor type, size, and origin; extension in the CP angle or in the IAC; patient’s age and general and neurological status, especially hearing level; and surgeon’s experience and institutional tradition. The approach should adhere to the following principles: it should provide sufficient exposure of the tumor; it should not be related to significant morbidity; the neural structures should not be at increased risk; any injury to the venous outflow system should be avoided. Most of the CP angle tumors are benign and their complete removal leads to healing of the patient. The preservation and even the recovery of neurological functions and of the patient’s quality of life should always be the first priority. The only exception to complete tumor removal is the attempt to preserve function, such as in surgery for VS in the only hearing ear. Excellent results have been achieved with different operative approaches, which depend more on the individual surgeon’s experience than on the advantages or disadvantages of each particular approach. Still, an ever growing amount of evidence suggests that the goals of CP angle surgery are best achieved with the retrosigmoid suboccipital approach (RSA).3,14–16 It is safe and relatively simple and provides a panoramic view of the whole CP angle and petroclival area. Importantly, it is associated with a very low procedure-related morbidity rate. The additional removal of the suprameatal tubercle—the Samii technique, developed and introduced by the senior author in 1982—provides access to tumor extensions into Meckel’s cave, the petroclival area, and even the posterior cavernous sinus.
Retrosigmoid Approach
A drawback of this patient position is the risk of venous air embolism, paradoxical air embolism, tension pneumocephalus, or circulatory instability. However, in experienced hands these effects are not related to any lasting morbidity.17 Transesophageal echocardiography is the most specific and sensitive method in detection of air embolism but the combined monitoring of end-tidal carbon dioxide and precordial Doppler echocardiography yield similar results. If immediate measures are carried out at the first sign of venous air embolism, the related morbidity is insignificant.
Continuous neurophysiological monitoring should be performed throughout the surgery from the time of positioning of the patient to the skin closure. It includes monitoring of somatosensory evoked potentials (important during patient positioning in order to prevent spinal cord compression); electromyography of the facial nerve; and monitoring of the brainstem auditory evoked potentials in the case of preoperatively available hearing.18,19 Monitoring of the oculomotor, trochlear, abducens, and caudal cranial nerves is performed if needed according to the particular tumor extension and clinical presentation.
A slightly curved skin incision approximately 2 cm medial to the mastoid process is performed and the underlying muscles are incised in line with the skin. We make the bur hole approximately 2 to 2.5 cm below the superior nuchal line, two thirds behind and one third in front of the occipitomastoid suture. The asterion is not an absolutely reliable anatomical landmark and is variable both in the cranial-caudal plane and in the anterior-posterior plane.20 The sigmoid sinus descends along an axis defined by the mastoid tip and the squamosal-parietomastoid suture junction or over the mastoid groove. The course of the transverse sinus is more variable and the superior nuchal line gives a rough orientation of its location. The issue of whether to make a craniectomy or craniotomy is a matter of individual preference but we avoid making one-piece craniotomy due to the related high risk of injury to the underlying sinuses and the risk of tearing the dura by the craniotome. Excessive traction to the mastoid emissary vein/veins could lead to sinus laceration and increases the risk of venous air embolism. The vein should be skeletonized with a diamond drill until it is free of any bony encasement and can be safely coagulated. The lateral and superior limits of the approach are the borders of the sigmoid and of the transverse sinuses; their edges have to be exposed. Inferiorly, enough bone should be removed in order to provide access to the lateral cerebellomedullary cistern and allow a continuous egress of the CSF or irrigation fluid throughout the surgery.
 The important neural structures, such as the cochlear and facial nerves, should be identified early.
The important neural structures, such as the cochlear and facial nerves, should be identified early.
 The tumor should be initially debulked.
The tumor should be initially debulked.
 The dissection from the surrounding structures should be performed only after sufficient internal decompression is achieved.
The dissection from the surrounding structures should be performed only after sufficient internal decompression is achieved.
 The dissection should always be performed in the arachnoid plane.
The dissection should always be performed in the arachnoid plane.
 Bipolar coagulation, especially in the vicinity of a cranial nerve, should be avoided.
Bipolar coagulation, especially in the vicinity of a cranial nerve, should be avoided.
Lateral Approaches
The main anatomical obstacle for exposure of the CP angle and of the petroclival area laterally is the petrous bone. Multiple operative techniques, including partial or complete resection of the petrous bone—the so-called transpetrous approaches—have been developed in the past decades. They differ in the approach to the petrous bone—subtemporal or transmastoid, as well as in the amount of bone removal.21 The advantages of these lateral cranial base approaches include shorter distance to the tumor and surrounding neurovascular structures, improved visualization, and minimized brain retraction.22 A major drawback is their higher approach-related morbidity rate. Our experience and the evaluation of the long-term outcome, however, prove that simpler and safer approaches lead to better outcome and do not limit the possibility to remove the tumor completely.14,16,23,24 The complete visualization of both the tumor and of all adjacent structures is not a prerequisite for better outcome.
The middle fossa approach is frequently used in cases of small intrameatal VSs: the tumor is exposed via a temporal craniotomy and removal of the bone overlying the IAC. The adequate access to a larger tumor requires more bone removal, including the resection of the petrous apex behind the horizontal segment of the petrous internal carotid artery medial to the IAC and incision of the tentorium (the extended middle fossa approach and the Kawase approach).14,22
Although the terminology used to describe the transmastoid approaches is quite variable,4 the main categories, in respect to the amount of drilling of the pyramid, are the presigmoid approach, the retrolabyrinthine petrosectomy, the translabyrinthine petrosectomy, and the transcochlear approach or complete petrosectomy. The presigmoid approach combines a supra- and infratentorial exposure with various degrees of petrosectomy. The retrolabyrinthine approach implies removal of the bone between the sigmoid sinus and the semicircular canals and allows hearing preservation. If the semicircular canals and the lateral wall of the IAC are removed, a large exposure both of the intrameatal and extrameatal tumor portions is gained (translabyrinthine approach). The transcochlear approach or complete petrosectomy allows for better visualization of the structures anterior to the IAC and petroclival space. It is used in large tumors in patients with complete hearing loss.
Vestibular Schwannomas
Clinical grading of facial nerve involvement is classified by the House and Brackmann scale (Table 38.1). During its further growth, the tumor reaches and then compresses the brainstem and the cerebellum. Depending on the degree of the tumor’s cranial and caudal extension, the fifth and the caudal cranial nerves become involved. The hydrocephalic stage begins with the obstruction of the fourth ventricle and its outlets. Each stage is characterized by specific neurological symptoms. This four-stage concept of growth presents the most frequent development pattern of VS but does not reflect entirely the high variability of these tumors and of the individual anatomy.
| Grade | Description/Deficit | Characteristics |
|---|---|---|
| I | Normal | Normal facial function |
| II | Slight | Gross: Slight weakness noted on close inspection, slight synkinesis At rest: Normal tone and symmetry Motion: |
At rest: Normal tone and symmetry
Motion:
At rest: Normal tone and symmetry
Motion:
At rest: Asymmetrical appearance
Motion:
Adapted from House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg1985;93(2):146-147.
VSs are classified either according to their maximal size or according to the degree of their extension into the CP angle. They are commonly divided into five categories: intrameatal, tumors up to 1 cm, from 1 to 2.5 cm, from 2.5 to 4 cm, or larger than 4 cm.25 Much more important than the size is the extent of the tumor in the CP angle, as well as the presence and severity of brainstem compression.18 Our classification based on the extent of tumor growth and its relation to the brainstem is presented in Table 38.2 (and Fig. 38.5A-G).
TABLE 38.2 INI or (Samii) Classification of Vestibular Schwannoma (VS) Extension
| Tumor Grade | Tumor Extension |
|---|---|
| T1 | Purely intrameatal |
| T2 | Intra-, extrameatal |
| T3a | Filling the CPA cistern |
| T3b | Reaching the brainstem |
| T4a | Compressing the brainstem |
| T4b | Severe compression and dislocation of brainstem and fourth ventricle |
| T5 | Giant tumors (maximal diameter >4 cm), extension over the midline |
∗In case the VS has been previously treated with radiosurgery, this is designated with an additional “+R”—e.g., Stage “T4a +R.”
CPA, cerebellopontine angle; INI, International Neuroscience Institute.
Treatment options of VS include observation, radiation therapy, and microsurgical removal via one of several operative approaches. The conservative approach—observation with regular follow-up MRI examinations and hearing tests—is based upon the assumption that some tumors stop growing or even undergo spontaneous regression.26 As the natural evolution of VS is still unpredictable, this strategy should be applied only in very carefully selected cases, with strict MRI follow-up (at 6- to 12-month intervals). This management may be applied in case of older or somatically unstable patients with small asymptomatic tumors or tumors causing mild stable symptoms. However, long-term follow-up results indicate that the majority of the tumors enlarge further. In published studies, further tumor growth was observed in 43% to 91% of the cases followed, but tumor involution or “negative growth” is observed in 0% to 18%.27–29 Another important issue is the loss of serviceable hearing during the follow-up. Charabi and associates29 reported that from the 28 patients initially classified as candidates for hearing preservation surgery, 75% were unable to have their hearing preserved due to tumor growth and deterioration of hearing following the time delay to surgery.
The goal of radiotherapy of VS, performed either as stereotactic radiosurgery or fractionated stereotactic radiotherapy, is to achieve tumor growth control. Gamma knife radiosurgery is by far the most popular mode: delivery of a single fraction of radiation after a highly conformal dose plan using multiple isocenters. The reduction of dose of radiation in the past few years led to marked reduction in cranial nerve morbidity. The recommended current doses are in the 12- to 14-Gy range and MRI is used for dosimetry planning. Tumor control is achieved in 93% to 98%.30–32 In 1.1% to 24% of the patients late facial neuropathy appears and the rate of trigeminal dysfunction is 2% to 27%. Hearing preservation is achieved in 40% to 74%. However, in 2% to 7% of the cases tumor enlargement is observed. Importantly, initial increase in tumor volume often precedes shrinkage. Additional treatment is indicated only if sustained tumor growth is documented on serial MRI, unless brainstem compression appears, prompting earlier intervention.32 The appearance of new neurological deficit alone is also not an indication for immediate intervention because it could be a delayed sequence of radiation. As the results of radiosurgical treatment cannot be precisely predicted, a careful follow-up of all patients is mandatory. Every case in which sustained tumor growth is confirmed or the progression of symptoms could be definitely related to tumor enlargement should be subjected to microsurgical removal, before the VS achieves large size. Our continuously increasing experience with surgery of previously irradiated VS shows that it is complicated by the development of postradiation changes. Frequently, the planes of dissection between the tumor and brainstem or cranial nerves are obliterated following radiotherapy, making the likelihood of functional preservation of involved cranial nerves substantially lower.
The only management option that leads to a definitive healing of the patient is complete surgical extirpation of the tumor. The modern VS surgery is related to a low risk of new morbidity and allows for functional preservation of cranial nerve function in exceedingly higher numbers. Complete tumor removal is achieved in 80% to 99% and the recurrence rates are 0.5% to 5%.15,18,33–36 The preservation of the anatomical integrity of the facial nerve is a rule today: it is achieved in 93% to 99% of the cases in the large published series.33,35–37 The main predictor of facial nerve outcome is the tumor size. In our series of VS with extension classes T1 to T3b, the rate of facial nerve preservation was 100%.33 Excellent or good postoperative facial nerve function (corresponding to House-Brackmann grades I to II) in the large series is achieved in 52% to 93%. In a recent study of 50 patients with giant VS—with maximal extrameatal diameter of 4.4 cm—total removal was possible in 97.6% of the patients. The anatomical integrity of the facial nerve was preserved in 92% in the first follow-up and at last follow-up 75% of the patients had excellent or good facial nerve function, and 19% had fair function.38 The rate of hearing preservation ranges from 14% to 80%,39,40 depending on the size of the VS. Although it has been suggested that in tumors larger than 3 cm hearing preservation is not possible and therefore the translabyrinthine approach should be used,36,41,42 we believe that an attempt for hearing preservation is worthwhile in every patient with useful preoperative hearing and good brainstem auditory evoked responses. Following this concept, we were able to achieve hearing preservation in 29% of the patients with VS extending to and compressing the brainstem (class T4a).33
The three most frequently used operative approaches are the (a) middle fossa, (b) the translabyrinthine, and (c) the retrosigmoid suboccipital approaches. The middle fossa approach is a hearing preserving technique that allows direct access to the lateral end of the IAC.39,43–46 Thus, the most lateral part of the tumor could be safely resected, reducing thereby the risk of incomplete removal. The approach is related to low risk of CSF leaks. However, it is applicable to small tumors, necessitates temporal lobe retraction, endangers the vein of Labbé, and offers a restricted access to the CP angle. Using the extended middle fossa approach, VS extending up to 2 cm in the CP angle can be removed.34,47
The benefits of the translabyrinthine approach include avoidance of cerebellar retraction, shorter distance to the tumor, and early identification of the facial nerve at the lateral end of the IAC.5,25,35,36,48 Drawbacks are sacrifice to hearing, restricted access to the CP angle, difficult dissection and hemostasis close to the brainstem, as well as poor visualization and access to the caudal cranial nerves.
The retrosigmoid approach allows for hearing preservation even in large VSs.3,18,33,39 The approach offers excellent visualization of the whole CP angle and increased safety during dissection from brainstem and lower cranial nerves.3,5 The facial and cochlear cranial nerves can be identified both in their proximal (close to the brainstem) and lateral part (in the IAC), increasing the chances for their preservation. Potential drawbacks of the approach are the need of cerebellar retraction, the difficulty in visualizing the most lateral part of the IAC without endangering the integrity of the inner ear, as well as the relatively higher rate of postoperative headache. However, a cranioplasty can be performed during closure which may improve the postoperative headache and pain issues (Fig. 38.6). With current neuroanesthesia and modifications of the original retrosigmoid approach and closure, these disadvantages are rather theoretical.33
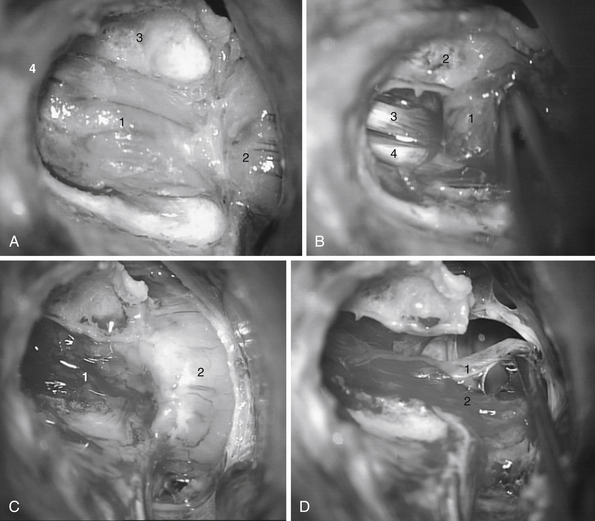
The initial steps of the exposure have been described earlier in the chapter. The intrameatal tumor portion is exposed initially. The dura is stripped off from the posterior lip of the porus and the posterior and superior walls of the internal auditory canal (IAC) are drilled using decreasing sizes of diamond drills under constant irrigation.
The extent of IAC opening is tailored to the extent of lateral tumor extension (Fig. 38.7A-G). The meatal dura is then incised and the intrameatal tumor portion is carefully mobilized with a microhook or microdissector. The facial and vestibulocochlear nerves are identified and the tumor is removed piecemeal. Then the extrameatal tumor is debulked with the Cavitron ultrasonic aspirator or a platelet-shaped knife. The dissection of the capsule from the surrounding neural structures should begin only after adequate internal decompression is achieved. It is performed by strictly gripping the tumor capsule and dissecting in the level of the arachnoid plane under continuous saline irrigation. Bipolar coagulation is reduced to a minimum and applied only at the end of surgery for final hemostasis. Once complete tumor removal is achieved, the continuity of the facial nerve can be confirmed by its electrical stimulation. In case of nerve discontinuity, immediate nerve reconstruction is performed at the same operation. The opened air cells in the region of the IAC are occluded by placing pieces of fat tissue fixed with fibrin glue.
Complications
Cerebrospinal fluid leaks are one of the most frequent complications and have been reported to occur with a rate of 3% to 26.7%.49,50 The most common factors associated with such leaks are inadequate dura and wound closure or healing, wound infection, increased intracranial pressure, and opened air petrous air cells that have not been occluded. In our experience the CSF leak is most frequently through the opened air cells during the IAC drilling. The prevention of CSF leaks relies on a watertight dural closure and meticulous sealing of opened air cells. Since we started to use multiple small fat pieces sealed with fibrin glue for plugging of the IAC the leak rate could be further reduced to 2.2% in our recent series.51 The fat can be harvested from the appropriate subcutaneous layer at the incision site. Further important steps are avoiding raising the intracranial pressure unwillingly during the early postoperative period; early detection of CSF leaks; and adequate treatment. If a CSF leak develops we insert immediately a lumbar drainage and keep it for at least 7 days. If the leak persists despite the drainage or reappears after its removal, surgical revision is required.
From 3% to 15% of the patients with VS have hydrocephalus as a consequence of tumor-induced obstruction at the level of the fourth ventricle and its outlets or due to inadequate resorption of CSF.52,53 Its optimal management is primarily tumor removal and treatment of the hydrocephalus only if it remains symptomatic thereafter. The insertion of a ventriculoperitoneal (VP) shunt can be avoided in most cases; in our series only 3.8% (5/53) of all patients with hydrocephalus required ultimately a VP shunt. In patients presenting with severe hydrocephalus-related symptoms an external ventricular drainage (EVD) should be inserted before VS surgery. In case of less severe symptoms, the VS is removed initially. The patients should be observed closely after surgery, both radiologically and clinically: if clinical deterioration is seen, correlating with a persisting or increasing widening of the ventricles, an EVD should be inserted and kept at 10 to 12 cm H2O above the level of the external auditory canal for several days. Then it should be elevated progressively, provided the patients showed no signs of intracranial hypertension—the process of gradual weaning from the EVD lasts up to 3 weeks. Only if the weaning fails is a VP shunt placement necessary. If hydrocephalus develops after the VS surgery, it can be managed similarly with a temporary EVD.
The incidence of postoperative symptomatic intracranial hemorrhage is reported to be between 1% and 3%.15,33,36 This potentially dangerous complication could be prevented by performing a meticulous hemostasis before dural closure. Hidden sources of bleeding should be actively searched for. The compressing of the jugular veins before and after removing the retractor allows for detection of any venous bleeding in the CP angle or from torn supracerebellar bridging veins.
In the past high rates of postoperative occipital headache have been reported and have been attributed to the retrosigmoid approach. Different factors have been implicated: dural adhesions to nuchal muscles or subcutaneous tissues, dural tension in cases of direct dural closure, intradural drilling, and the use of fibrin glue. The reconstruction of the occipital bone with methyl methacrylate (see Fig. 38.3) offers the possibility of achieving good cosmetic result and prevents scar tissue formation between the dura and neck muscles, thus preventing the development of such headaches. The occcurrence of pseudomeningocele is related mainly to the method used for dura and bone reconstruction. Using the above-mentioned techniques we never have experienced such complications.
Meningiomas
Meningiomas located in the CP angle lateral to the trigeminal nerve, regardless of the site of their dural attachment, are defined as CP angle meningiomas, and those located medial to the trigeminal nerve are defined as petroclival meningiomas.54 They are the second most common tumor of the CP angle and have similar epidemiological and biological features to other meningiomas:55 they are slow growing benign lesions that occur most frequently in women, usually in 68% to 92%, in their fifth to sixth decades of life.
CP angle meningiomas arise from groups of arachnoid cells located in high concentrations around the IAC, the lower border of superior petrosal sinus, the lateral border of the inferior petrosal sinus, around the cranial nerve foramina, and in the region of the geniculate ganglion. They are a rather heterogeneous group and have variable attachment sites and extension patterns. Their relation to the surrounding structure and the dislocation of cranial nerves cannot be predicted. In relation to the IAC they are classified as premeatal and retromeatal meningiomas.54,56 These two types present with distinct clinical features, require different treatment strategy, and have different prognoses. The more medially located the tumor, the greater is the surgical challange and the poorer is the outcome. CP angle meningiomas are further subclassified into premeatal, postmeatal, suprameatal, and inframeatal groups, and those centered at the IAC; however, this subdivision has no major practical significance.5,16,57
MRI allows for reliable preoperative differentiation from VS and provides information on their precise location in the CP angle, as well as on their relation to the cochlear and facial nerves. In contrast to VS, in which the differences among patients are a function mainly of tumor size and extent of extrameatal growth, the variety of clinical presentations of CP angle meningiomas is greater. It depends on the size, site of dural attachment, and location of the lesion. The initial complaints are most frequently hearing loss, vertigo, headache, or trigeminal symptoms.5,16,58 Auditory or vestibular dysfunction is not always the major presenting symptom. At the time of diagnosis hearing loss is observed in 30% to 73% of the cases. Trigeminal nerve signs are found in 13% to 49% of the patients, and cerebellar signs and symptoms are found in in 25% to 52%.12,59 Tinnitus is noted by 10% to 12% of the patients. Signs of increased intracranial pressure have been reported in 16% to 29% and hydrocephalus in 20% to 31% of the patients in different series. Three percent of the cases of trigeminal neuralgia are due to tumor compression at the root entry zone of the trigeminal nerve and the tumors causing such compression most frequently are meningiomas. Premeatal and retromeatal meningiomas have typical clinical development and symptomatology. Premeatal tumors are diagnosed earlier and consequently are smaller. Their clinical presentation is with trigeminal signs and facial and cochlear nerve signs, whereas retromeatal meningiomas present with cerebellar signs (see Fig. 38.4A and B).
Treatment strategies for CP angle meningiomas are similar to those for VS: observation, surgery, radiotherapy/radiosurgery, or combinations thereof. Total surgical removal is the optimal treatment option but should not be achieved at the expense of new neurological dysfunctions or worsening of quality of life. Different surgical approaches have been successfully used for resection of CP angle meningiomas: the retrosigmoid, the translabyrinthine, the transpetrosal with its multiple modifications, as well as the approaches through the middle cranial fossa.5,55,59 Still, the principles regarding tumor removal are similar: adequate exposure, interruption of the blood supply along the dural attachment, internal decompression, and cautious dissection of the tumor capsule from the brainstem and cranial nerves at the arachnoid plane. The experience of the senior author has shown that every CP meningioma can be adequately accessed via a retrosigmoid craniotomy. If the tumor is located retromeatally, the pure retrosigmoid approach (RSA) is sufficient; in meningiomas originating anterior to the IAC with propagation into Meckel’s cave, petroclival area, or the posterior cavernous sinus, the suprameatal extension of the retrosigmoid approach is required.14
The hearing-destructive approaches, such as the transpetrosal and translabyrinthine, have been proposed for patients with severe hearing deficit. Attempts at hearing preservation are proposed to be taken only in retromeatal tumors. On the other hand, hearing loss is usually attributed to compression of the cochlear nerve and hearing restoration has been reported even after removal of large meningiomas.57 We believe that every attempt should be made to preserve or increase the chances of recovery of neurological functions. The versatility and safety of the retrosigmoid approach makes it the most widely used. It allows removal of both small and large tumors, as well as hearing preservation. With the retrosigmoid approach hearing is preserved in 82% to 90.8% of the patients.16,55,57
The outcome of surgery depends mainly on the location and consistency of the tumor, and to a lesser extent on its size. Thus, in the premeatal CP angle meningiomas the preservation of facial and auditory function is less likely than in the retromeatal tumors. The mortality rate in the large series is between 0% and 9%.12,16,54,59 The percentage of total removal of pure CP meningiomas in experienced hands is 82% to 90% and is limited primarily by the tumor infiltration of the brainstem, cranial nerves, and vessels and the extent of skull base involvement.12,16,54,59 In the 10% to 20% of the cases in which the pia mater of brainstem or a cranial nerve is infiltrated, part of the capsule should be left to avoid neural damage. Such remnants should be controlled with MRI studies, performed 3 to 6 months after surgery. If they show a growth tendency, radiosurgery/radiotherapy should be considered. Compared to VS, CP angle meningiomas have higher tendency toward recurrence, with a recurrence rate between 0% and 9.5%.
Radiotherapy or radiosurgery has been proposed as a primary treatment option for small meningiomas.60,61 Surgery may be still required in case of treatment failure or in case a secondary trigeminal neuralgia after the irradiation of a petroclival or Meckel’s cave meningioma develops. In case of less than total tumor removal or recurrence, postoperative radiation therapy or radiosurgery has been known to prolong the interval to recurrence and to improve the survival.
Epidermoids
Epidermoids or epidermoid cysts are the third most common CP angle tumor.61–63 They are slow growing lesions that extend along the basal cisterns and cause gradual displacement of brainstem and other neural structures. Epidermoids might expand through the tentorial incisura into the middle cranial fossa, grow toward the contralateral CP angle, or extend toward the foramen magnum. These tumors are sometimes densely adherent to the neurovascular structures.
Patients with epidermoids usually present between the third and fifth decades of life with a long-standing history of tinnitus and hearing loss.63 They cause relatively more frequently trigeminal neuralgia or hemifacial spasm when compared to VS and meningiomas and lead to facial nerve signs much earlier than VS.
The treatment of choice of epidermoids is surgical and the preferred approach is the retrosigmoid.61,63,64 The endoscope-assisted microsurgical technique has proved to be extremely useful, allowing the surgeon not only to detect hidden tumor parts but also to remove them under endoscopic control. Because of the risk of additional neurological deficits, small remnants of the capsule that are firmly attached to important structures should not be removed. The rates of radical removal range from 50% to 97%. In subtotal resected epidermoids, a late recurrence can develop even after 20 or 30 years, which mandates close follow-up on a long-term basis.
Brackmann D.E., Cullen R.D., Fisher L.M. Facial nerve function after translabyrinthine vestibular schwannoma surgery. Otolaryngol Head Neck Surg. 2007;136:773-777.
Lunsford L.D., Niranjan A., Flickinger J.C., et al. Radiosurgery of vestibular schwannomas: summary of experience in 829 cases. J Neurosurg. 2005;102(Suppl):195-199.
Rhoton A.L.Jr. The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery. 2000;47:S93-129.
Samii M., Gerganov V., Samii A. Improved preservation of hearing and facial nerve function in vestibular schwannoma surgery via the retrosigmoid approach in a series of 200 patients. J Neurosurg. 2006;105:527-535.
Samii M., Matthies C. Management of 1000 vestibular schwannomas (acoustic neuromas): surgical management and results with an emphasis on complications and how to avoid them. Neurosurgery. 1997;40(1):11-21.
Slattery W.H.III, Brackmann D.E., Hitselberger W. Middle fossa approach for hearing preservation with acoustic neuromas. Am J Otol. 1997;18(5):596-601.
Yasargil M.G., Abernathey C.D., Sarioglu A.C. Microsurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989;24(4):561-567.
Please go to expertconsult.com to view the complete list of references.
1. Pellet W. History of vestibular schwannoma surgery. Prog Neurol Surg. 2008;21:6-23.
2. Koerbel A., Gharabaghi A., Safavi-Abbasi S., et al. Evolution of vestibular schwannoma surgery: the long journey to current success. Neurosurg Focus. 2005;18:e10.
3. Rhoton A.L.Jr. The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery. 2000;47:S93-129.
4. Nanda A.V.P. Temporal bone and acoustic neuroma. Semin Neurosurg. 2000;11:325-338.
5. De Monte F. Neoplasms and the cranial nerves of the posterior fossa. In: Barrow D.L., editor. Surgery of the Cranial Nerves of the Posterior Fossa. Park Ridge, IL: American Association of Neurological Surgeons; 1993:253-254.
6. Bonneville F., Savatovsky J., Chiras J. Imaging of cerebellopontine angle lesions: an update. Part 2: intra-axial lesions, skull base lesions that may invade the CPA region, and non-enhancing extra-axial lesions. Eur Radiol. 2007;17:2908-2920.
7. Bonneville F., Savatovsky J., Chiras J. Imaging of cerebellopontine angle lesions: an update. Part 1: enhancing extra-axial lesions. Eur Radiol. 2007;17:2472-2482.
8. Brackmann D.E., Bartels L.J. Rare tumors of the cerebellopontine angle. Otolaryngol Head Neck Surg. 1980;88:555-559.
9. Lakshmi M., Glastonbury C.M. Imaging of the cerebellopontine angle. Neuroimaging Clin North Am. 2009;19:393-406.
10. Wilms G., Plets C., Goossens L., et al. Differentiation of acoustic neurinoma and meningioma occurring together in the cerebellopontine angle. Neurosurgery. 1992;30(3):443-445.
11. Zamani A.A. Cerebellopontine angle tumors: role of magnetic resonance imaging. Top Magn Reson Imaging. 2000;11:98-107.
12. Voss N.F., Vrionis F.D., Heilman C.B., Robertson J.H. Meningiomas of the cerebellopontine angle. Surg Neurol. 2000;53:439-446.
13. Roser F., Nakamura M., Dormiani M., et al. Meningiomas of the cerebellopontine angle with extension into the internal auditory canal. J Neurosurg. 2005;102(1):17-23.
14. Samii M., Gerganov V.M. Surgery of extraaxial tumors of the skull base. Neurosurgery. 2008;62:1153-1168.
15. Tonn J.C., Schlake H.P., Goldbrunner R., et al. Acoustic neuroma surgery as an interdisciplinary approach: a neurosurgical series of 508 patients. J Neurol Neurosurg Psychiatry. 2000;69:161-166.
16. Bassiouni H., Hunold A., Asgari S., Stolke D. Meningiomas of the posterior petrous bone: functional outcome after microsurgery. J Neurosurg. 2004;100(6):1014-1024.
17. Von Goesseln H.H., Sur D., Bini W., et al. The lounging position for posterior fossa surgery: anesthesiological considerations regarding air embolism. Childs Nerv Syst. 1991;7(7):368-374.
18. Samii M., Matthies C. Management of 1000 vestibular schwannomas (acoustic neuromas): surgical management and results with an emphasis on complications and how to avoid them. Neurosurgery. 1997;40(1):11-21.
19. Samii M., Matthies C. Management of 1000 vestibular schwannomas (acoustic neuromas): hearing function in 1000 tumor resections. Neurosurgery. 1997;40(2):248-262.
20. Bozbuga M., Boran B.O., Sahinoglu K. Surface anatomy of the posterolateral cranium regarding the localization of the initial burr-hole for a retrosigmoid approach. Neurosurg Rev. 2006;29(1):61-63.
21. Rhoton A.L.Jr., Tedeschi H. Lateral approaches to the cerebellopontine angle and petroclival region (honored guest lecture). Clin Neurosurg. 1994;41:517-545.
22. Erkmen K., Pravdenkova S., Al-Mefty O. Surgical management of petroclival meningiomas: factors determining the choice of approach. Neurosurg Focus. 2005;19(2):E7.
23. Ciric I., Rosenblatt S., Wiet R., et al. Suboccipital retrosigmoid approach for removal of vestibular schwannomas: facial nerve function and hearing preservation. Neurosurgery. 2005;56(3):560-570.
24. Ojemann R.G. Retrosigmoid approach to acoustic neuroma (vestibular schwannoma). Neurosurgery. 2001;48:553-558.
25. Brackmann D.E., Green J.D. Translabyrinthine approach for acoustic tumor removal. Otolaryngol Clin North Am. 1992;25(2):311-329.
26. Bakkouri W.E., Kania R.E., Guichard J.P., et al. Conservative management of 386 cases of unilateral vestibular schwannoma: tumor growth and consequences for treatment. J Neurosurg. 2009;110:662-669.
27. Smouha E.E., Yoo M., Mohr K., Davis R.P. Conservative management of acoustic neuroma: a meta-analysis and proposed treatment algorithm. Laryngoscope. 2005;115:450-454.
28. Rosenberg S. Natural history of vestibular schwannomas. Laryngoscope. 2000;110(4):497-508.
29. Charabi S., Thomsen J., Mantoni M., et al. Acoustic neuroma (vestibular schwannoma): growth and surgical and nonsurgical consequences of the wait-and-see policy. Otolaryngol Head Neck Surg. 1995;113:5-14.
30. Lunsford L.D., Niranjan A., Flickinger J.C., et al. Radiosurgery of vestibular schwannomas: summary of experience in 829 cases. J Neurosurg. 2005;102(Suppl):195-199.
31. Battista R.A. Gamma knife radiosurgery for vestibular schwannoma. Otolaryngol Clin North Am. 2009;42:635-654.
32. Prasad D., Steiner M., Steiner L. Gamma surgery for vestibular schwannoma. J Neurosurg. 2000;92:745-759.
33. Samii M., Gerganov V., Samii A. Improved preservation of hearing and facial nerve function in vestibular schwannoma surgery via the retrosigmoid approach in a series of 200 patients. J Neurosurg. 2006;105:527-535.
34. Gjuric M., Wigand M.E., Wolf S.R. Enlarged middle fossa vestibular schwannoma surgery: experience with 735 cases. Otol Neurotol. 2001;22:223-230.
35. Brackmann D.E., Cullen R.D., Fisher L.M. Facial nerve function after translabyrinthine vestibular schwannoma surgery. Otolaryngol Head Neck Surg. 2007;136:773-777.
36. Lanman T.H., Brackmann D.E., Hitselberger W.E., Subin B. Report of 190 consecutive cases of large acoustic tumors (vestibular schwannoma) removed via the translabyrinthine approach. J Neurosurg. 1999;90:617-623.
37. Gormley W.B., Wright D.C., Kamerer D., et al. Acoustic neuroma: results of current surgical management. Neurosurgery. 1997:50-60.
38. Samii M., Gerganov V.M., Samii A. Functional outcome after complete surgical removal of giant vestibular schwannomas. J Neurosurg. 2010;112(4):860-867.
39. Irving R.M., Jackler R.K., Pitts L.H. Hearing preservation in patients undergoing vestibular schwannoma surgery: comparison of middle fossa and retrosigmoid approaches. J Neurosurg. 1998;88:840-845.
40. Nadol J.B.Jr., Chiong C.M., Ojemann R.G., et al. Preservation of hearing and facial nerve function in resection of acoustic neuroma. Laryngoscope. 1992;102:1153-1158.
41. Brackmann D.E., Owens R.M., Friedman R.A., et al. Prognostic factors for hearing preservation in vestibular schwannoma surgery. Am J Otol. 2000;21:417-424.
42. Yates P.D., Satar B., Pitts L.H., et al. Is it worthwhile to attempt hearing preservation in larger acoustic neuromas? Otol Neurotol. 2003;24(3):460-464.
43. Arts H.A., Telian S.A., El-Kashlan H., Thompson B.G. Hearing preservation and facial nerve outcomes in vestibular schwannoma surgery: results using the middle cranial fossa approach. Otol Neurotol. 2006;27:234-241.
44. Colletti V., Fiorino F. Middle fossa versus retrosigmoid-transmeatal approach in vestibular schwannoma surgery: a prospective study. Otol Neurotol. 2003;24:927-934.
45. Slattery W.H.3rd, Francis S., House K.C. Perioperative morbidity of acoustic neuroma surgery. Otol Neurotol. 2001;22:895-902.
46. Slattery W.H.III, Brackmann D.E., Hitselberger W. Middle fossa approach for hearing preservation with acoustic neuromas. Am J Otol. 1997;18(5):596-601.
47. Kanzaki J., Ogawa K., Shiobara R., et al. Hearing preservation by the extended and nonextended middle cranial fossa approach for acoustic neuroma. Skull Base Surg. 1994;4:76-81.
48. Day J.D., Chen D.A., Arriaga M. Translabyrinthine approach for acoustic neuroma. Neurosurgery. 2004;54:391-395.
49. Hoffman R.A. Cerebrospinal fluid leak following acoustic neuroma removal. Laryngoscope. 1994;104:40-58.
50. Rodgers G.K., Luxford W.M. Factors affecting the development of cerebrospinal fluid leak and meningitis after translabyrinthine acoustic tumor surgery. Laryngoscope. 1993;103(9):959-962.
51. Ludemann W.O., Stieglitz L.H., Gerganov V., et al. Fat implant is superior to muscle implant in vestibular schwannoma surgery for the prevention of cerebrospinal fluid fistulae. Neurosurgery. 2008;63:ONS38-ONS42.
52. Pirouzmand F., Tator C.H., Rutka J. Management of hydrocephalus associated with vestibular schwannoma and other cerebellopontine angle tumors. Neurosurgery. 2001;48:1246-1253.
53. Rogg J.M., Ahn S.H., Tung G.A., et al. Prevalence of hydrocephalus in 157 patients with vestibular schwannoma. Neuroradiology. 2005;47:344-351.
54. Samii M., Ammivati M. Cerebellopontine angle meningiomas (posterior pyramid meningiomas). In: Al-Mefty O., editor. Meningiomas. New York: Raven Press; 1991:503-515.
55. Matthies C., Carvalho G., Tatagiba M., et al. Meningiomas of the cerebellopontine angle. Acta Neurochir Suppl. 1996;65:86-91.
56. Schaller B., Merlo A., Gratzl O., et al. Premeatal and retromeatal cerebellopontine angle meningioma. Two distinct clinical entities. Acta Neurochir Wien. 1999;141(5):465-471.
57. Nakamura M., Roser F., Dormiani M., et al. Facial and cochlear nerve function after surgery of cerebellopontine angle meningiomas. Neurosurgery. 2005;57:77-90.
58. Mallucci C.L., Ward V., Carney A.S., et al. Clinical features and outcomes in patients with non-acoustic cerebellopontine angle tumours. J Neurol Neurosurg Psychiatry. 1999;66:768-771.
59. Thomas N.W., King T.T. Meningiomas of the cerebellopontine angle. A report of 41 cases. Br J Neurosurg. 1996;10:59-68.
60. Stafford S.L., Pollock B.E., Foote R.L., et al. Meningioma radiosurgery: tumor control, outcomes, and complications among 190 consecutive patients. Neurosurgery. 2001;49(5):1029-1038.
61. Safavi-Abbasi S., Di Rocco F., Bambakidis N., et al. Has management of epidermoid tumors of the cerebellopontine angle improved? A surgical synopsis of the past and present. Skull Base. 2008;18:85-98.
62. Schiefer T.K., Link M.J. Epidermoids of the cerebellopontine angle: a 20-year experience. Surg Neurol. 2008;70:584-590.
63. Samii M., Tatagiba M., Piquer J., Carvalho G.A. Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg. 1996;84:14-19.
64. Yasargil M.G., Abernathey C.D., Sarioglu A.C. Microsurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989;24(4):561-567.