47 Celiac Plexus Block
Placement
Anatomy
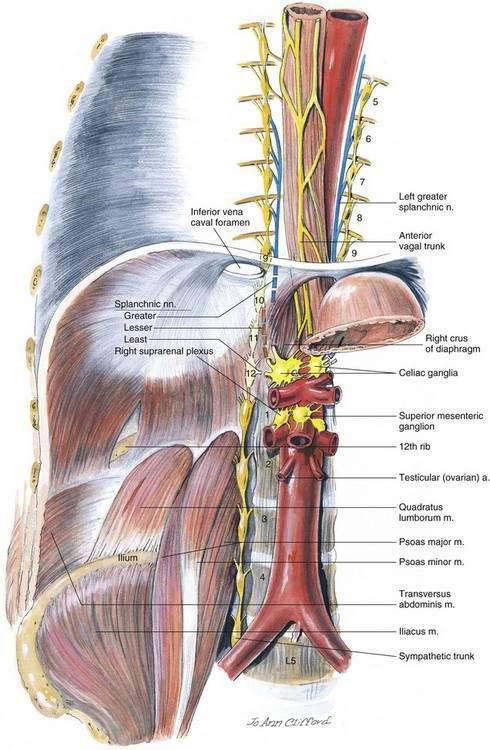
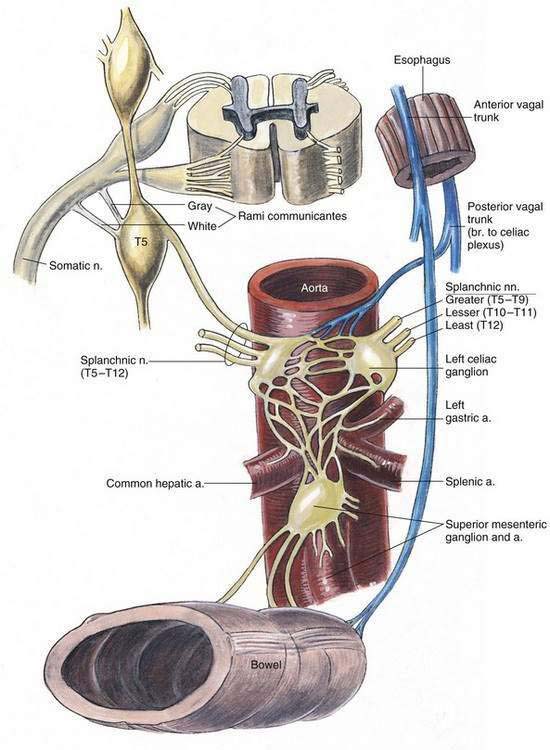
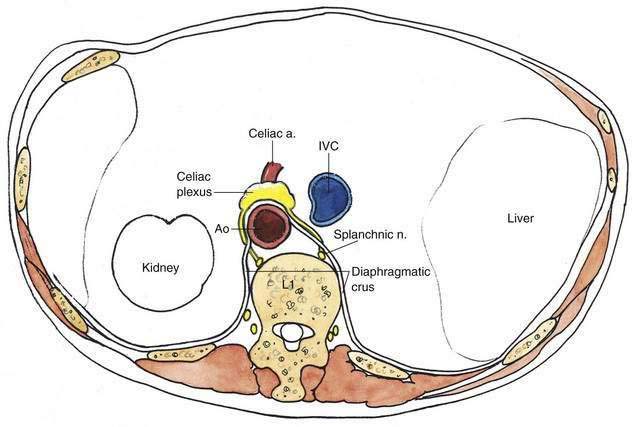
The celiac plexus has also been called the solar plexus, the celiac ganglion, and the splanchnic plexus (Fig. 47-1). It is the largest of the three great plexuses of the sympathetic nervous system in the chest and abdomen: the cardiac plexus innervates the thoracic structures, the celiac plexus innervates the abdominal organs, and the hypogastric plexus supplies the pelvic organs. All three of these plexuses contain visceral afferent and efferent fibers. In addition, they contain some parasympathetic fibers that pass through after originating in cranial or sacral areas of the parasympathetic nervous system.
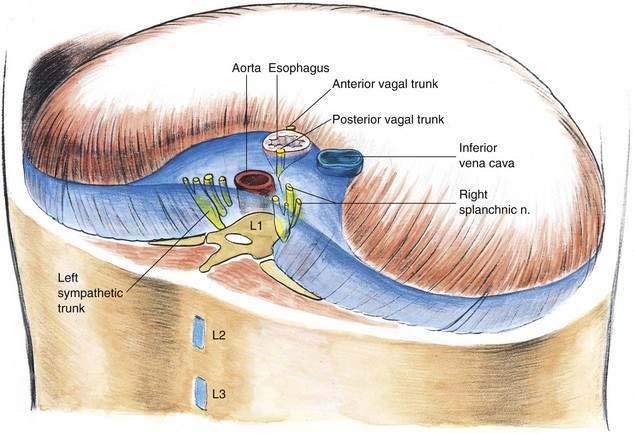
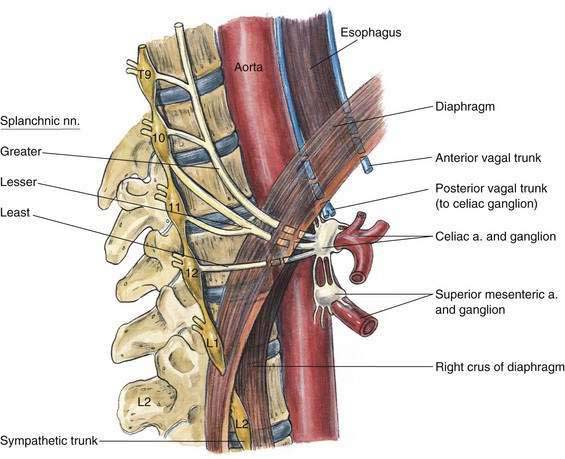
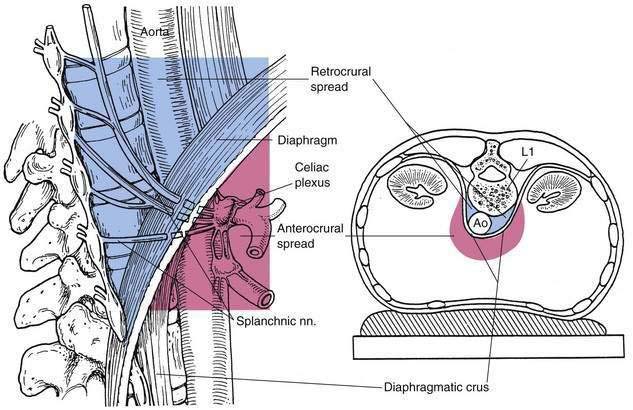
The celiac plexus innervates most of the abdominal viscera, including the stomach, liver, biliary tract, pancreas, spleen, kidneys, adrenals, omentum, small bowel, and large bowel to the level of the splenic flexure. The celiac plexus receives its primary innervation from the greater, lesser, and least splanchnic nerves, which arise from T5 through T12. The splanchnic nerves innervate the celiac plexus after traversing the posterior mediastinum and entering the abdomen through the crura of the diaphragm, a variable distance above L1 (Figs. 47-2 and 47-3). The splanchnic nerves are preganglionic, and after they synapse in the celiac ganglion proper (or associated ganglia), their postganglionic fibers radiate to the abdominal viscera (Fig. 47-4). Autopsy examination has shown that the number of ganglia making up the celiac plexus ranges from one to five, with the size of ganglia ranging from 0.5 to 4.5 cm in diameter.
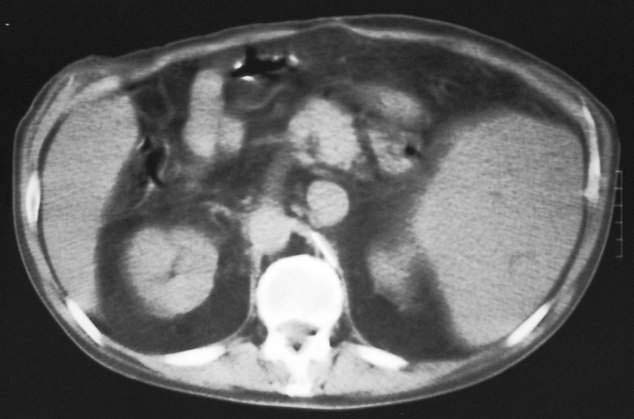
The celiac plexus is found anterolateral to the celiac artery. In addition, the vena cava is often anterolateral on the right, the aorta is posterior to the plexus in the midline, the kidneys are lateral, and the pancreas lies anteriorly (Figs. 47-5 and 47-6).
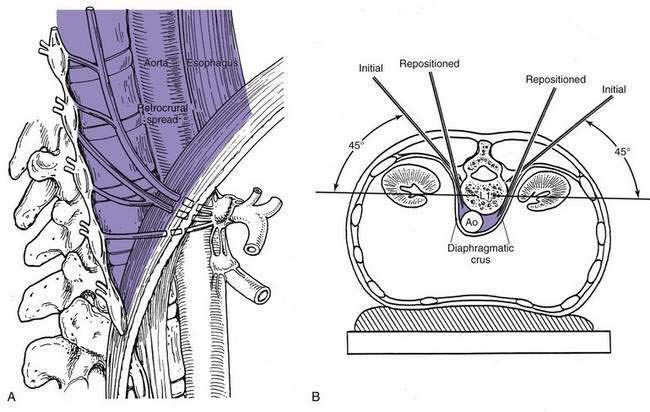
One point of anatomic clarification that is essential for understanding the celiac plexus block is that there are two basic methods of carrying out the block. In the longest-used method, the needles are inserted to perform a deep splanchnic block. This results in spread of the solution (blue, as illustrated in Fig. 47-7) cephalad and posterior to the diaphragmatic crura. The second method involves placing the needle through one crus of the diaphragm from a posterior approach, or through the anterior abdominal wall, to end up with the needle placed anterior to the aorta in the region of the celiac plexus. As illustrated in Figure 47-7, this results in spread of solution (pink) in the vicinity of the celiac artery, anterior to the diaphragmatic crura.
Needle Puncture: Method
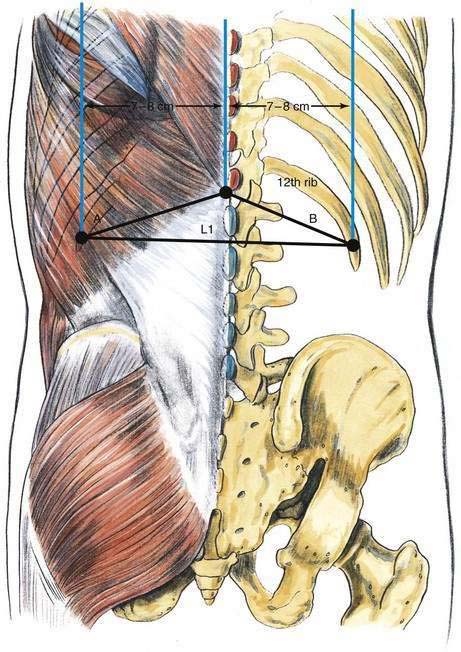
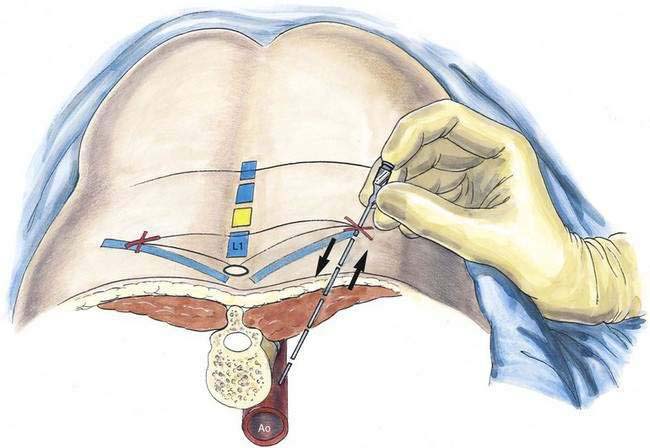
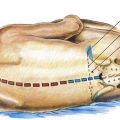
The lumbar vertebral spinous processes, as well as the 12th thoracic vertebral spinous process, should be identified and marked. Parallel lines should then be drawn 7 to 8 cm off the midline, as shown in Figure 47-8. The 12th rib should be palpated and a mark placed where the paramedian lines cross the 12th rib bilaterally. Another mark should be placed in the midline between the 12th thoracic and 1st lumbar vertebral spinous processes. By drawing lines between the three marks, a flat isosceles triangle is created. The equal sides of this triangle (A and B) serve as directional guides for the bilaterally placed needles.
Skin wheals should then be raised on the marks immediately below the 12th rib, and a 12- to 15-cm, 20- or 22-gauge needle is inserted without the syringe attached, as shown in Figure 47-9. The needle is inserted 45 degrees off the plane of the tabletop, directed at the space between the T12 and the L1 vertebral spinous processes. This placement will allow contact with the L1 vertebral body at a depth of 7 to 9 cm. If bony contact is made at a more superficial level, it is likely that a vertebral transverse process has been contacted. In today’s practice of pain care, most patients will have their celiac block performed with fluoroscopic guidance, simplifying needle insertion.
When the vertebral body is confidently identified, the needle is withdrawn to a subcutaneous level and the angle is increased to allow the tip to pass the lateral border of the vertebral body. On the left side (the side of the aorta), once the needle passes off the vertebral body, it should be inserted an additional 1.5 to 2 cm or until the aortic wall is identified by pulsations transmitted through the length of the needle. On the right side, the needle can be inserted 2 to 3 cm after it “walks off” the vertebral body. It is helpful in inserting the needles to the proper depth to insert the left needle first because it can be advanced slowly until the operator’s sensitive fingertips (Fig. 47-10) appreciate the aortic pulsations transmitted up the needle shaft. When this aortic depth is identified, the right needle can then be inserted and readily advanced to a slightly deeper level.
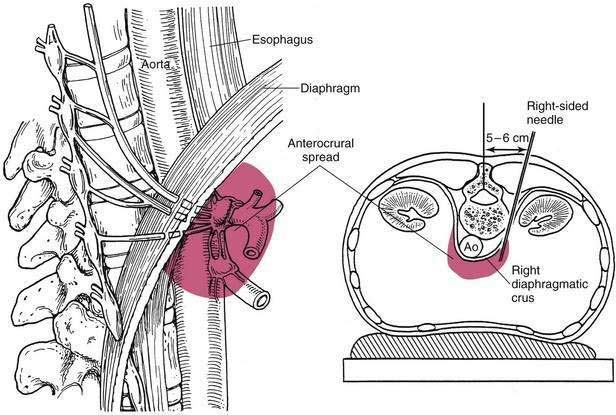
Needle Puncture: Anterocrural Method
The second basic method of celiac plexus block is the anterocrural approach, which results in the needle tip’s being placed anterior to the crus of the diaphragm on the right side, as illustrated in Figure 47-11. To carry out this block, all the foregoing steps are the same, except that the paramedian line on the right is drawn 5 to 6 cm off the midline, rather than 7 to 8 cm as in the classic retrocrural approach. The needle is inserted to strike the vertebral body. Often an angle larger than 45 degrees is necessary to contact the vertebral body initially. When the vertebral body is contacted, the needle is withdrawn and redirected until it “walks off” the anterolateral edge of the vertebral body. To place an anterocrural needle properly, radiographic assistance is necessary. Commonly, the needle must be inserted 10 to 13 cm to place its tip anterior to the crus of the diaphragm. It is helpful to use a supplementary imaging technique for the transcrural approach because passage of the needle tip through the crus of the diaphragm is difficult to appreciate by palpation unless a transaortic method similar to the method of Ischia is used. Once the needle tip is in position anterior to the crus of the diaphragm, local anesthetic solution is injected through the single right-sided needle.