Catheter Ablation for Ventricular Tachycardia in Patients With Structural Heart Disease
Catheter ablation has an important role in reducing or preventing episodes of ventricular tachycardia (VT). The optimal ablation approach and its efficacy are determined by the characteristics of the arrhythmia and the anatomy and location of the arrhythmia substrate, which can often be anticipated from the electrocardiographic characteristics of the arrhythmia and any underlying heart disease. Most VTs that are considered for ablation are monomorphic, with the same QRS complex from beat to beat indicating repetitive ventricular activation from a structural substrate or a focus that can be targeted for ablation. In patients with heart disease, more than one morphology of sustained monomorphic VT is often inducible. VT that has the same electrocardiogram (ECG) QRS morphology and cycle length as one that has been observed to occur spontaneously is designated a “clinical VT.”1 Often the ECG morphology of VT is not known a priori, because the arrhythmia is clinically terminated by an implantable cardioverter defibrillator (ICD), and only the cycle length and intracardiac electrograms are known. VTs that are then induced and are similar in cycle length and morphology in available ECG leads or recordings are designated “presumed clinical VTs.”1 Inducible VTs that have not been documented to occur spontaneously are designated as having uncertain clinical significance or “undocumented VT.” Ablation can be used to control recurrent polymorphic VT or VF in selected patients when the triggering foci or substrate for the arrhythmia can be identified.2,3
Preparation and Consideration of Risks
Mortality is rare in patients without structural heart disease, but perforation, tamponade, coronary injury, and AV block can occur. In patients with structural heart disease, procedure-related mortality is approximately 2%, with most deaths being related to uncontrollable VT with hemodynamic deterioration in patients with severe disease when the procedure fails.1,4 Preprocedure planning is important to minimize risks. Underlying heart disease should be defined. The potential for myocardial ischemia should be assessed. Although ischemia is not usually the cause of monomorphic VT, it can contribute to hemodynamic instability and increase the risk of the procedure if not addressed. It is important to consider fluid balance, electrolyte abnormalities, anemia, and metabolic abnormalities, such as hyperthyroidism, that might contribute to hemodynamic deterioration or development of uncontrollable arrhythmias during the procedure. The use of external irrigation ablation catheters administers intravascular volume that requires attention to fluid balance and diuresis to avoid development of pulmonary edema or aggravation of heart failure if extensive ablation is needed.
Cerebral or systemic embolism is reported in 0.0% to 2.7% of patients.4,5 If endocardial left ventricular mapping is planned, then echocardiography should be performed. A mobile left ventricular (LV) thrombus is a contraindication to LV mapping. If laminated thrombus is suspected, a period anticoagulation therapy with warfarin may be considered with the hope of stabilizing potentially friable thrombus, although the efficacy of this approach is not known. During LV mapping and ablation, systemic anticoagulation is achieved with heparin. After ablation, continued anticoagulation with aspirin or warfarin is recommended depending on the extent of ablation performed.
LV access is usually achieved with a retrograde aortic approach across the aortic valve. Damage to the valve or coronary artery ostia is possible, but rare. Significant vascular access complications, including significant bleeding, arterial dissection, and femoral AV fistulas, occur in 2.1% of patients.4,5 A transseptal approach via the left atrium allows access to the LV through the mitral valve for patients with peripheral vascular disease or a mechanical aortic valve or when insertion of multiple mapping catheters is desired.
Approach to Mapping and Ablation
QRS Morphology During Ventricular Tachycardia and Pacemapping
In nonischemic cardiomyopathy, an epicardial origin is suggested by a VT QRS with a relatively long QRS duration and slow QRS upstroke, producing a pseudo–delta waves; these findings could be due to delayed activation of the endocardial Purkinje system compared with endocardial VTs.6,7 A QS complex with the absence of initial R waves in leads reflecting the region of initial activation in VT, such as lead I in the presence of posterobasal scar and the inferior leads in the presence of inferior wall scar, often indicates an epicardial VT origin.7,8 In patients with prior myocardial infarction, the VT QRS morphology does not reliably identify which VTs require epicardial ablation.9
Initial Assessment of Induced Ventricular Tachycardia
Recordings from the His bundle region and RV apex are usually obtained. A His bundle potential before each QRS onset suggests the possibility of bundle branch reentry (see Chapter 83), although one-to-one passive conduction into the Purkinje system is also possible. Pacing is often performed from the RV apex to entrain or terminate VT. Entrainment from the RV apex with a postpacing interval of 30 ms or less further suggests bundle branch reentry or a VT circuit close to the apex.10 Activation recorded from the RV catheters provides some limited mapping data. Relatively early ventricular activation at the basal septum (His bundle region) or apical septum indicates a septal origin of VT. Further mapping is based on whether VT is likely focal or scar-related reentry.
Focal-Origin Ventricular Tachycardia
Focal-origin VTs should be suspected in patients without structural heart disease, who have typical QRS morphologies for outflow tract (see Chapter 81) or papillary muscle VT sites (see Chapter 80), and for repetitive monomorphic and nonsustained VTs and PVCs. A focal origin is confirmed by activation mapping that shows spread away in all directions from the focus. Automaticity or small reentry circuits are possible mechanisms. The VT origin is identified as the site of earliest ventricular activation relative to the QRS onset. Pacing at the site of origin will produce a QRS morphology replicating that produced by the arrhythmia focus, provided that pacing captures the small area at the focus and not the surrounding myocardium, but is not as accurate as activation mapping and is sometimes misleading.1 Focal VTs are often found along the valve annuli (pulmonic, aortic, mitral, and tricuspid). The complex anatomy in some of these locations can render the QRS morphology and pacemapping particularly unreliable for guiding ablation.11 VT that originates in sleeves of myocardium extending along the aorta or pulmonary artery must be identified from sites of earliest activation before the QRS onset during the arrhythmia (see Chapter 81).
Inability to induce the VT is a common problem that limits mapping. Immediately on arrival in the electrophysiology laboratory, attention should be directed to recording a 12-lead ECG of any spontaneous arrhythmia that can provide a template to guide pacemapping if the arrhythmia is not inducible after placement of catheters. Minimizing sedation and avoiding excess administration of local lidocaine anesthesia, which can be absorbed and result in systemic levels, are important considerations. Administration of β-agonists, such as isoproterenol, or epinephrine boluses may be effective. The arrhythmia can emerge as heart rate slows during washout from the effect of a β-agonist. There are also anatomical obstacles. The VT focus can be located deep within the myocardium, or at the summit of the LV, where it is not approachable with standard ablation.12 Epicardial foci may be under a coronary artery (see Chapter 127) where ablation risks damaging the artery.13 Electroanatomical mapping systems, imaging with intracardiac ultrasound, angiography, and incorporation of preprocedure cardiac computed tomography or magnetic resonance imaging (MRI) can be helpful in clarifying anatomic complexities.14,15
Ablation of focal PVCs that trigger polymorphic VT and ventricular fibrillation can be used to control frequent episodes of these arrhythmias (see Chapter 97). Arrhythmia in this case can occur in the absence of structural heart disease, in areas of infarction, or associated with a myopathic processes.16–18 The origin is most often found in the Purkinje system or RV outflow tract.
Scar-Related Reentry
Scar-related reentry is the most common cause of sustained monomorphic VT in structural heart disease.1 Scars can be due to prior myocardial infarction, cardiomyopathies, or surgical incisions. The location of the scar as indicated by wall motion abnormalities, or delayed gadolinium enhancement on MRI suggests the region likely to contain the VT substrate.19–22 Regions of dense fibrosis that create conduction block combined with surviving myocytes bundles with interstitial fibrosis and diminished coupling produces circuitous conduction paths for slow conduction that is the substrate for reentry. Stable circuits can be modeled as having an isthmus or channel composed of a small mass of tissue that does not contribute to the surface ECG (Figures 124-1, 124-2). The QRS onset occurs when the excitation wavefront emerges from an exit along the border of the scar and spreads across the ventricles. Reentry circuit configurations and locations are variable. Scars related to VT often border a valve annulus that forms a border segment for part of the circuit.23–25 Slow, stable VTs are often due to relatively large macroreentry circuits spanning several centimeters.26 Multiple VTs with different QRS morphologies can be due to multiple exits from the same region of scar, or changes in activation remote from the circuit because of functional regions of block.26–29 Ablation at one region could abolish more than one VT.25,29–31 Multiple reentry circuits from widely separated areas also occur. The location of the scar that provides the arrhythmia substrate is a major determinant of the mapping approach and likely success of ablation. The substrate and reentry circuits locations can be subendocardial, subepicardial, or intramural, and vary with the type of heart disease, being most commonly endocardial in prior infarcts, epicardial in arrhythmogenic RV cardiomyopathy, and variable in other cardiomyopathies.
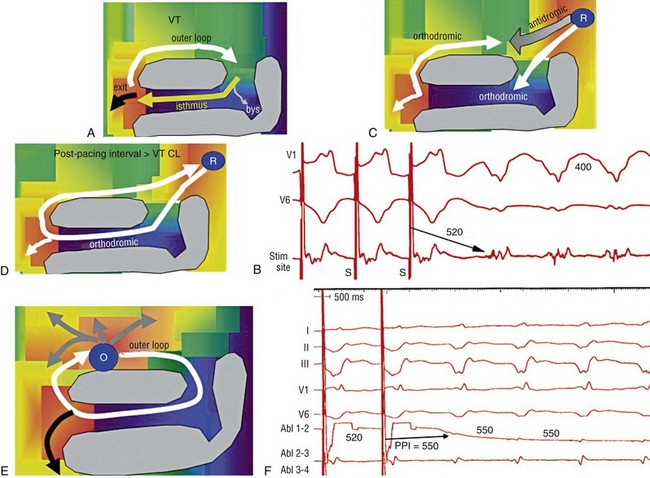
Figure 124-1 Entrainment of reentrant ventricular tachycardia (VT). A, C, D, and E show schematics of a theoretic reentry circuit with areas of dense scar (gray) defining the circuit. Activation sequence is indicated by arrows and colors proceeding from red to yellow to green to blue to purple. A, The VT circuit with an isthmus (yellow arrow), outer loop along the border of the scar (white arrow), and bystander region (bys; gray arrow). The QRS onset would occur when the wavefront emerged from the exit region. B, Entrainment from a remote bystander site and the findings are shown schematically in the VT circuits in C and D. VT with a cycle length of 400 ms is present. The last three stimuli of a pacing train accelerate the QRS complexes and electrograms to the pacing cycle length with a change in QRS morphology compared to VT. The postpacing interval (PPI) is 520 ms, exceeding the VT cycle length by 120 ms. C, The stimulated wavefronts divide into antidromic wavefronts (gray arrow), which alters the ventricular activation sequence compared with tachycardia changing the QRS morphology. The stimulated orthodromic wave front resets the tachycardia circuit. D, After the last stimulus, the stimulated orthodromic wavefront propagates through the circuit and back to the pacing site, such that the PPI is equal to the tachycardia cycle length plus the conduction time from the pacing site to the circuit and from the circuit back to the pacing site. In E and F, the effects of pacing at an outer loop site along the border of the scar. F, Pacing accelerates the QRS complexes and electrograms. The PPI of 550 ms matches the VT cycle length, indicating that the site is in the circuit as shown schematically by the white arrow in E. Subtle QRS fusion is evident in the change in QRS morphology in lead I during pacing. Absence of any delay between stimulus and QRS also indicates that the site is not in an isthmus.
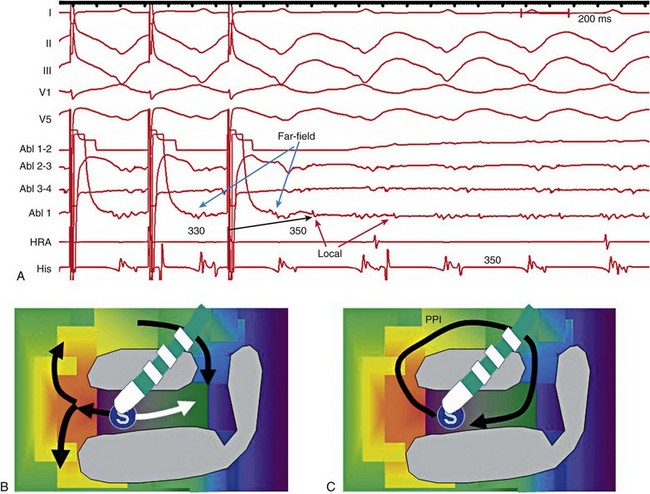
Figure 124-2 Entrainment from an epicardial isthmus site (A) from the patient shown in Figure 124-1 and schematics (B and C) are shown. From the top of A are surface electrocardiogram (ECG) and cardiac recordings from the epicardial ablation catheter (Abl) with bipolar records from distal (1-2), mid (2-3), and proximal (3-4) electrodes and a high-pass–filtered unipolar recording from electrode 1 (Abl 1), high right atrium (HRA), and His bundle region (His). Ventricular tachycardia (VT) with a cycle length of 350 ms is present. Unipolar pacing at 330 ms from the distal electrode of the ablation catheter accelerates the QRS complexes and electrograms to the pacing rate. Measurement of the postpacing interval (PPI) requires assessment of which electrogram most likely indicates the local potential. During pacing, a broad fractionated potential is visible, indicating that this is a far-field potential (blue arrows). The potential that is not visible during pacing is the likely local potential (red arrow). The PPI measured to the local potential is 350 ms, matching the VT cycle length. The QRS during pacing is identical to that of VT (also confirmed in the 12-lead ECG that is not shown). These findings are consistent with pacing from an isthmus in the reentry circuit as shown schematically in B and C. Stimulated orthodromic wave fronts are indicated by black arrows. The stimulated antidromic wave front is the white arrow in B.
Substrate Mapping During Sinus or Paced Rhythm
Voltage Maps
Areas of scar can often be identified during stable sinus rhythm, along with potential exits and channels, facilitating ablation in patients with multiple and unstable VTs.27,28,32,33 Electroanatomical mapping systems recreate the geometry of the ventricles from point by point mapping, intracardiac ultrasound images, or registration of pre-acquired computed tomography or MRI images and allow electrophysiological features to be displayed in relation to the anatomy (see Chapter 60. EP Mapping and Navigation19,21,34 Scar associated with myocyte loss and fibrosis are characterized by low amplitude electrograms. Voltage maps are plots of peak to peak electrogram amplitude (Figure 124-3).28,33 In normal ventricular myocardium > 95% of sites have a bipolar electrogram amplitude exceeding 1.5 mV (recorded with an ablation catheter with large tip electrode, 1 mm interelectrode spacing and filtered at 10 to 400 Hz). Recent studies correlating voltage maps with regions of delayed gadolinium enhancement in MRIs of infarct regions have found that areas with bipolar electrograms less than 1.5 mV in amplitude are associated with fibrosis typically occupying at least 75% of the ventricular wall,19,35 and that less extensive fibrosis is present at surrounding regions. Bipolar electrogram amplitude thresholds for 95% of normal sites are slightly lower for the right ventricle (< 1.44 mV).28 During epicardial mapping, bipolar electrogram amplitude exceeds 1 mV at 95% of normal sites; however, lower-amplitude signals are recorded normally over a thick region of fat along the AV groove and coronary arteries.36,37 Electrograms recorded over fat do not display fractionation or long durations; therefore, these features are often useful in distinguishing clearly abnormal regions from normal myocardium with overlying fat.
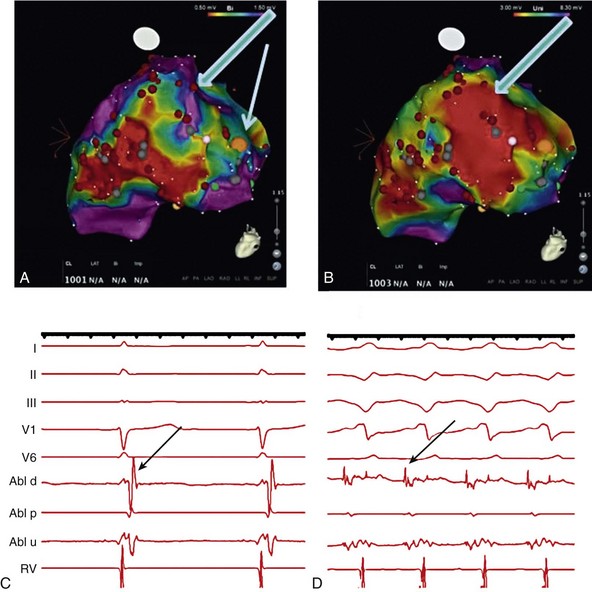
Figure 124-3 Electroanatomic voltage mapping in a patient with prior posterolateral infarction viewed from an inferolateral angulation. A, A bipolar voltage map where purple (normal) areas are indicated by an electrogram amplitude of 1.5 mV or greater. B, A unipolar voltage map where purple (normal) areas are indicated by an electrogram amplitude of 8.3 mV or greater. Note the larger area subtended by abnormal voltage in the unipolar map (heavy blue arrow); this likely indicates intramural or epicardial scar beyond that appreciated on the bipolar voltage map. C and D, Electrograms recorded from the orange dot at the inferior mitral annulus (thin blue arrow in A) in sinus rhythm and in VT, respectively. C, The terminal portion of the ablation signal (thin black arrow) is a late potential occurring after the terminal portion of the QRS, fused with the far-field electrogram. During VT (D), this electrogram is fractionated with a large presystolic component.
An endocardial region of bipolar electrograms less than 1.5 mV is specific for subendocardial scar, but it does not identify epicardial or intramural scar.19,35 Epicardial and intramural scars can potentially be identified from unipolar recordings.38 Unipolar recordings filtered at 1 to 250 Hz contain substantial far-field signal. Endocardial unipolar signals less than 8.3 mV in the LV and less than 5.5 mV in the RV have been shown to be associated with epicardial or intramural scar despite endocardial bipolar electrogram amplitude greater than 1.5 mV (see Figure 124-3).38–40 The low voltage region is likely to contain the reentry circuit but is often large, exceeding 20 cm in circumference in many patients with infarct.27
Exits and Channels
Additional analyses of electrograms, voltage, or pacemapping are used to refine selection of target sites.41,42 Exit regions are typically located along the scar border (Figure 124-4). Pacing in the exit region replicates the QRS morphology of VT.42,43 The interval between the stimulus and QRS onset is typically short, which is consistent with its location in the infarct border.
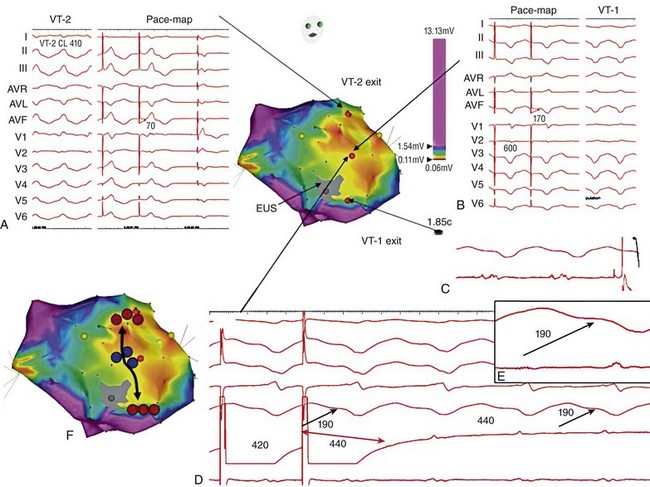
Figure 124-4 Findings from mapping in a patient with a prior anterior wall infarction are shown. The center and panel F show a voltage map viewed from the right anterior projection. Purple indicates an electrogram amplitude of 1.5 mV or greater. A gray region of electrically unexcitable scar is present. A, Ventricular tachycardia (VT)-2 that has a right bundle branch block configuration inferior axis configuration. Pacing at the superior aspect of the infarct (arrow) reproduces the VT-2 QRS morphology indicating that the exit for VT-2 is near the pacing site. B, Pacing at a site in the middle of the infarct. There is a delay of 170 ms from the pacing stimulus to the QRS, indicating slow conduction through the scar to the margin of the infarct. The paced QRS has a left bundle branch block superior axis configuration that matched VT-1, suggesting that the pacing site was in a channel used by VT-1; this is confirmed by pacing during VT-1 (D). There is entrainment with concealed fusion with a postpacing interval that matches the VT cycle length. Pacing resets tachycardia with a long stimulus to a QRS interval without changing the QRS morphology and with a postpacing interval (measured to the low-amplitude diastolic potential that is enlarged in panel of D) matches the VT cycle length. C, The exit for VT-1 was at the inferior margin of the infarct, where presystolic activity is recorded during VT. F, shows the potential channel (black arrow) with exits at the superior and inferior septal margin of the infarct, that likely used a loop along the border of the infarct. Potential ablation targets are the exits (red circles) or the channel (blue circles). (Modified with permission from Stevenson WG, Soejima K: Catheter ablation for ventricular tachycardia, Circulation 115:2750–2760, 2007.)
Potential channels within low-voltage regions can be identified from analysis of electrograms and pacemapping. In some cases, the borders of potential channels are defined by dense fibrosis that has a lower amplitude electrogram than that of the channel (Figure 124-5).44,45 Similarly, if the border is dense fibrosis, it may be electrically unexcitable, such that pacing (10 mA at 2 ms pulse width with unipolar pacing) fails to capture.25 Marking these electrically unexcitable scar (EUS) areas (gray area on the voltage map in Figure 124-4) creates a visual map of potential channels in some patients. Narrow bands of fibrosis likely elude this method of detection. Pacing provides complimentary information to analysis of electrogram amplitude. EUS cannot be detected reliably based on electrogram amplitude alone. Pacing captures at many sites with low electrogram amplitudes of less than 0.25 mV. In contrast, some EUS sites have electrogram amplitude greater than 0.5 mV because of the presence of large far-field potentials from depolarization of a substantial mass of adjacent myocardium in the border area or outside the scar (see Figure 124-5).
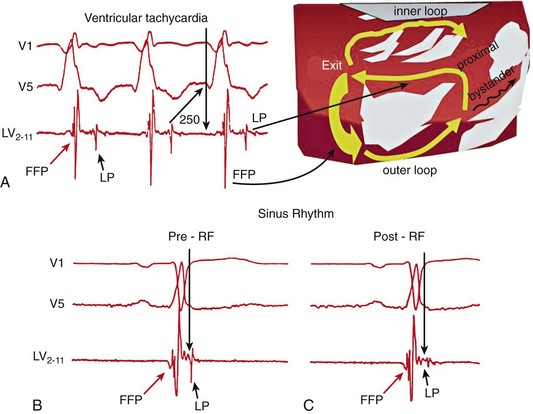
Figure 124-5 Recordings from a region of scar in patients with prior myocardial infarction and a schematic illustrating the potential reentry circuit location. A, Ventricular tachycardia (VT) is present. An isolated diastolic potential is present at the site (blue arrow). A potential is also inscribed during the QRS comlex, which is a far-field potential from depolarization of surrounding myocardium. Ablation at this site terminated VT (not shown). The recordings during sinus rhythm before (B) and after (C) sinus rhythm are shown. A late potential is present during sinus rhythm (B). Ablation markedly diminishes the late potential (C), whereas the far-field potential is intact. (Modified with permission from Harada T, Stevenson WG, Kocovic DZ, Friedman PL: Catheter ablation of ventricular tachycardia after myocardial infarction: relation of endocardial sinus rhythm late potentials to the reentry circuit, J Am Coll Cardiol 30:1015–1023, 1997.)
Electrograms from channels are often smaller than the far-field electrograms produced by depolarization of the larger mass of myocardium outside the scar (see Figure 124-2). When conduction delay into the channel is present during sinus rhythm, these low-amplitude potentials can be inscribed as a late potential occurring after the end of the QRS.46–48 When the electrogram is inscribed at the same time as the far-field signal, it can become evident and separate from the far-field signal during VT or when pacing or premature stimuli delay conduction into the channel (see Figure 124-3).47 Jaïs et al.47 termed these potentials and late potentials “local abnormal ventricular activation” (LAVA).47 Case series have shown that targeting late potentials in low-voltage regions and LAVA potentials is an effective strategy in some patients and that elimination of LAVA or late potentials predicts better outcome.46,47,49,50
Pacemapping in a channel produces a QRS that appears after a delay (S – QRS > 40 ms) because of slow conduction of the stimulated wavefront through the channel (see Figure 124-4). When the wavefront emerges from an exit region, the paced QRS morphology resembles VT, suggesting that the pacing site is in a reentry circuit isthmus.42,48 If the wave front leaves the scar by another path, such as the entrance to a channel, the paced QRS morphology might differ from VT or resemble a different VT.
Targeting these markers of potential reentry circuit channels can facilitate ablation for patients with multiple and unstable VTs. The complexity of the reentry circuit configurations and areas of slow conduction and block in diseased ventricles are such that they are not always sufficient to define a reentry circuit location. Additional mapping and entrainment during VT can be helpful to confirm that a region is in a reentry circuit and to facilitate successful ablation with fewer ablation lesions.27 Alternatively, RF lesions can be placed through presumptive exits or channels, followed by retesting for inducible VT.27,28,43 Even when VT is stable, substrate mapping can be used to identify regions for further evaluation during VT (discussed later), minimizing the time spent in VT.
Mapping During Ventricular Tachycardia
During VT, assessment of activation and entrainment are useful for targeting the reentry circuit.26,27,51,52 When VT is not stable for extensive mapping, these assessments can still be useful during brief episodes of tachycardia to confirm that a region identified during substrate mapping is involved in the tachycardia. Hemodynamic support with percutaneously placed ventricular rotary pumps, left atrial–femoral bypass, or femoral vein to femoral artery cardiopulmonary bypass, can be used to allow mapping during VT or to stabilize the condition of patient who develops VT storm.53,54 Whether these approaches improve outcomes compared to substrate guided approaches is not established. Mechanical support devices have potential complications related to vascular access and thromboembolism, and some interfere with electroanatomical mapping.
Activation Mapping and Electrograms
During VT, presystolic activation is recorded at the circuit exit, and earlier diastolic activation is recorded from more proximal isthmus sites, often in the form of an isolated potential. Sites that are proximal in the isthmus can be activated during the end of the QRS complex, without diastolic electrical activity, but can be identified by entrainment.55 Multielectrode and noncontact mapping systems acquire electrograms from multiple sites simultaneously. Detection of low-amplitude signals in isthmuses is difficult, but the exit in the border region is often identifiable.29,56–58
Entrainment Mapping
Entrainment mapping can confirm the relation of an individual site to the reentry circuit (see Figures 124-1, 124-2, 124-4).59 During entrainment, pacing at a rate faster than the tachycardia continuously resets the reentry circuit (see Figure 124-1). Entrainment is confirmed by criteria that include evidence of constant fusion between paced orthodromic and antidromic wave fronts, and progressive fusion owing to proportionately greater activation of the ventricles by paced antidromic wavefronts as the pacing rate is increased.60 The demonstration of entrainment indicates that reentry with an excitable gap in the circuit is the tachycardia mechanism.
The postpacing interval (PPI) is an indication of the proximity of the pacing site to the reentry circuit.59 The last stimulus that entrains VT produces a wave front that propagates to the reentry circuit, orthodromically through the circuit, and returns to the pacing site. Thus the time from the last pacing stimulus to the next activation at the pacing site is equal to the conduction times for propagation from the pacing site to the circuit, one revolution through the circuit (the tachycardia cycle length), and then back to the pacing site. For sites that are in the circuit, the conduction time from pacing site to circuit and back equals zero, and the PPI equals the tachycardia cycle length. At pacing sites removed from the circuit, the PPI increases as a function of the conduction time between the site and the reentry circuit.
Interpretation of the PPI requires that three assumptions be satisfied. The first is that the pacing stimuli reliably capture the myocardium. The second is that the time of activation at the pacing site following the last stimulus can be determined from the electrograms.61 Far-field electrograms can often be recognized by their visible presence during pacing, indicating that they are not due to direct depolarization of that tissue by the pacing stimulus (see Figure 124-2) and will produce a misleading PPI if used for measurement. In contrast, the local potential is obscured by the stimulus artifact during pacing. When the local potential cannot be assessed late after the stimulus, because of saturation of the recording amplifier, measuring the PPI to electrograms recorded on the adjacent proximal electrodes, that are not far-field potentials, agrees with the distal electrode recordings at approximately 85% of sites.62 The S-QRS n+1 technique can also be used to assess the PPI.63 The third assumption is that pacing does not alter conduction times in the circuit or the reentry path. Slowing of conduction, as is common in the presence of antiarrhythmic medications, falsely prolongs the PPI.
At sites that are in broad portions of the reentry circuit, such as reentry loops along the border of the scar, entrainment occurs with QRS fusion because of propagation of stimulated wave fronts away from the pacing site, but the PPI indicates that the pacing site is in the circuit.64
Termination of VT by pacing stimuli that capture without producing a propagated response, such that no QRS complex follows the stimulus, also indicate that the site is likely to be in an isthmus.65 The stimulated antidromic wave front is extinguished by collision with a returning orthodromic wave front. The stimulated orthodromic wave front encounters refractory tissue and blocks terminating tachycardia. Alternatively, the stimulus can extend the refractory period at the pacing site.
Other Ablation Targets
Approximately 8% of patients with sustained monomorphic VT associated with structural heart disease have bundle branch reentry as the cause of one of their VTs, although scar-related reentry is often present as well.66 Ablation of the right bundle branch typically eliminates this VT. Occasionally interfascicular reentry requires ablation of left bundle fascicles. Portions of the Purkinje system can also be involved in scar-related reentry circuits, particularly after myocardial infarction.67,68 These VTs can have a relatively narrow QRS duration of 145 ms or less with Purkinje potentials present in the exit region. Rarely, automaticity in the Purkinje system is the cause of VT in patients with structural heart disease.66 VT often requires isoproterenol administration for initiation. These VTs can be ablated at sites where a Purkinje potential is present and linked to the VT.
Ablation Strategies and Acute Endpoints for Scar-Related Ventricular Tachycardia
If VT is hemodynamically tolerated, mapping and ablation can be performed during VT, seeking VT termination. Scar-related VTs can require substantial lesions for interruption facilitated with irrigated or large (e.g., 8 mm) electrodes (see Chapter 122). Markers of lesion creation include a reduction or complete abolition of electrograms, increase in pacing threshold, and termination and prevention of reinitiation of VT.25,27,50,69
When VT is incessant or hemodynamically tolerated, or a clear clinical VT is identifiable, the primary aim of the procedure is to abolish that VT. When a VT isthmus can be identified, ablation is highly successful. Other morphologies of VT are often inducible, indicating the presence of other potential reentry circuits. Some centers attempt to abolish all inducible VTs, or all inducible mappable VTs, in the hope of reducing recurrences.27,28,43,70–72
Ablation lesion sets for multiple and unmappable VTs include ablation lines through exit regions, ablation through all identified isthmuses, ablation through isthmuses or exits extending to the border of the scar, and ablation of all diastolic potential or LAVA sites.46,47,49,50 These strategies and endpoints have not been compared directly. In a series of 70 patients with scar-related VTs, Jaïs et al.47 observed that VT recurred in 32% of patients in whom these potentials could be eliminated by ablation, compared to 75% of those in whom the potentials could not be eliminated. In a series of 64 patients with scar-related VT, Vergara observed recurrent VT in 10% of patients in whom late potentials were eliminated by ablation, compared to 75% of those in whom ablation failed to eliminate late potentials.50
After ablation, no monomorphic VT of any type can be induced in 38% to 95% of patients. Remaining inducible VTs are often faster and initiated by more aggressive stimulation than the initial VTs.27,30,72 When the clinical or presumptive clinical VT remains inducible after ablation, the recurrence risk exceeds 60%.71,73 Absence of any inducible VT has been associated with a lower but still significant incidence of recurrence ranging from less than 3% to 27% in single-center reports and up to 44% in a multicenter study.5,25,27,70–73 Inducible, nonclinical VTs are associated with increased risk of recurrence in some studies.72,74 Healing of initial ablation lesions and reduction of antiarrhythmic medications likely contribute to recurrences. Some patients benefit from a repeated procedure.75
There are several considerations when endocardial ablation is not successful. The reentry circuit could be subepicardial (see Chapter 126).76 In a series in which epicardial mapping is performed after failed endocardial ablation, more than 70% of patients were found to have an epicardial VT substrate.76,77 This is often suggested by the nature of the underlying heart disease, being frequent in arrhythmogenic RV cardiomyopathy and nonischemic cardiomyopathy, and the QRS configuration of VT (discussed earlier).78 In addition, the unipolar endocardial voltage map could suggest epicardial or intramural scar (discussed earlier).39,40 Endocardial mapping may show a pattern of focal activation from an endocardial breakthrough site that incorrectly suggests a focal origin.79
The VT can have an intramural origin. An intramural septal origin is suspected when the sites closest to the VT circuit are located on either side of the ventricular septum or at adjacent endocardial and epicardial sides of the ventricular free wall.39 Ablation at the best adjacent sites is usually attempted. Intracoronary ethanol ablation can also be considered in selected patients (discussed later).
Ablation in Specific Diseases
The arrhythmia substrate, and consequently ablation approaches and outcomes, vary with the type of heart disease. Ablation is usually successful for abolishing VT in patients without structural heart disease, as discussed in Chapters 80, 81, and 82. Ablation is often more challenging in patients with heart disease. In most series, these patients have recurrent episodes of VT that has failed drug therapy, and they often have more than one morphology of inducible VT.
Prior Myocardial Infarction
The majority of VT circuits can be ablated from an endocardial approach. Ablation is acutely successful, abolishing one or more VTs in 77% to 95% of patients (Table 124-1).41,80,81 In patients who have had multiple VT recurrences despite antiarrhythmic drug therapy, previously ineffective antiarrhythmic drugs are often continued. VT recurs in 19% to 50% of patients, although the frequency is reduced for the majority. Multiple morphologies of VT and unstable VTs are associated with a higher risk of recurrence.27,30 Failure of endocardial ablation can be due to intramural or epicardial reentry circuits.82,83 Procedure mortality is 2% to 3% and major complications occur in 5% to 10% of patients.
Table 124-1
Selected Large Recent Series of Catheter ablation of VT in Patients With Structural Heart Disease
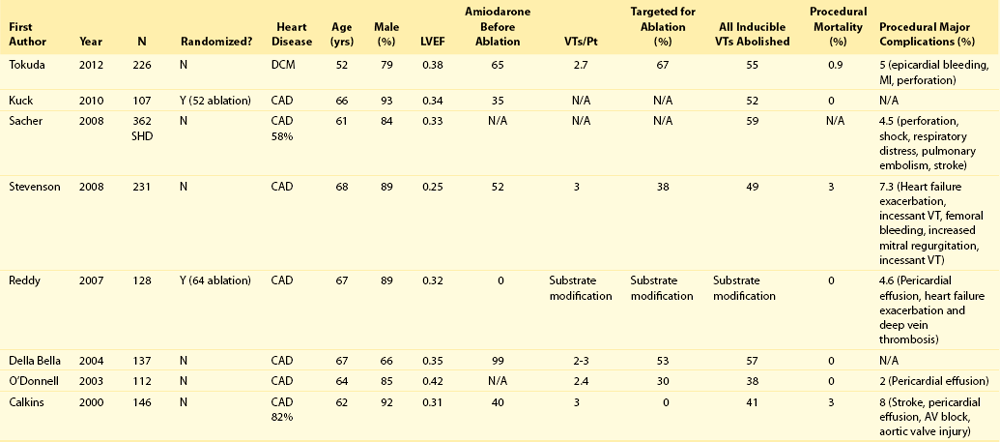
The annual mortality following catheter ablation for recurrent VT ranges from 5% to more than 20%.74,84,85 Progressive heart failure is the most common single cause of death and is consistent with the severity of heart disease and the association of VT as a marker for mortality and heart failure despite the presence of an ICD.86 Greater age, LV size and dysfunction, renal dysfunction, and recurrence of VT are markers for increased mortality.74,84,85 The potential for ablation to adversely affect LV function is of concern. Assessment of LV ejection fraction after ablation has not shown deterioration, but is not very sensitive for detection of injury.28,87 Confining ablation to regions of scar and attention to medical therapy for ventricular dysfunction seems prudent.
Whether earlier use of ablation, prior to multiple VT recurrences, improves outcomes has been evaluated in two randomized studies. In the VTACH trial, ablation was performed in patients with hemodynamically tolerated VT who were receiving ICDs. Catheter ablation extended the time to recurrent VT from a median of 5.9 months to 18.6 months, and reduced the frequency of VT.88 In the SMASH VT trial, substrate-guided ablation was performed for hemodynamically untolerated VT in patients receiving ICDs. In this trial, ablation of VT reduced ICD shocks from 31% to 9% over a mean follow-up of 22.5 ± 5 months, and it reduced VT episodes from 33% to 12%.89 These trials were too small to assess an effect on mortality.
Dilated Cardiomyopathy and Valvular Heart Disease
More than 80% of patients with sustained monomorhic VT have scar-related reentry; in the remainder, VT is due to bundle branch reentry or a focal origin.49,90 Scars can be demonstrated with MRI and are often adjacent to a valve annulus, but can be epicardial or intramural in more than one third of patients (see Figures 124-3, 124-4).20,32,36,77,91 Ablation is generally more difficult than for infarct-related VT and is more likely to require epicardial ablation. More than 70% of those who fail endocardial ablation are found to have subepicardial VTs if epicardial mapping can be performed.36,77 Late potentials and low-voltage regions indicating the substrate are generally smaller and more difficult to detect, consistent with intramural or epicardial substrate.46,49,50 Relatively small series are reported showing that VT is controlled in 50% to 82% of patients.36,46,77 Incessant idiopathic VT or ventricular ectopy can cause tachycardia-induced cardiomyopathy that improves after ablation.
Right Ventricular Cardiomyopathies
Scar-related RV tachycardias occur in idiopathic cardiomyopathy, genetic arrhythmogenic RV cardiomyopathy, and cardiac sarcoidosis.37,79,92–97 Scar can be identified from endocardial and epicardial voltage maps and on delayed enhancement on MRI.37,97–99 Scars causing VT are often adjacent to the tricuspid or pulmonic annulus.24,79 Focal-origin VTs caused by automaticity also occur. Epicardial circuits are particularly common in arrhythmogenic right ventricular cardiomyopathy, and epicardial ablation appears to improve outcomes in these patients.37,40,96,100–103 In a nonrandomized case series, Bai et al.96 reported freedom from VT over 3 years 85% of patients who received endocardial and epicardial ablation compared to 52.2% of 23 patients treated with endocardial ablation only. Ablation for VT caused by sarcoidosis has also been associated with a high recurrence rate.93
Thus, outcomes appear to be related to underlying heart disease. Ablation is palliative therapy for frequent symptomatic episodes in some patients. Cardiac perforation is the major complication, but it is infrequent.73 Death from hemodynamic deterioration in uncontrollable VT has occurred.101,102
Repaired Congenital Heart Disease
Scar-related VT involving RV regions of repair also occur later after surgical correction of congenital heart disease, notably tetralogy of Fallot.104,105 In tetralogy of Fallot, VT usually involves an isthmus that can be interrupted with ablation between the tricuspid or pulmonary valve annulus, and scar or patch material in the free wall of the RV.105 Catheter ablation is feasible, with successful outcomes during follow-up in 43% to 91% of patients reported in relatively small series with follow-up exceeding 2 years.104,105
Other Diseases
Ablation has been used successfully to control scar-related recurrent sustained monomorphic VT in patients with a history of myocarditis,90 hypertrophic cardiomyopathy,106 and valvular heart disease. An increasing number of patients are receiving left ventricular assist devices as destination therapy or as a bridge to cardiac transplantation. VT impairs hemodynamics in these patients, and small series have shown that catheter ablation can be useful for controlling the arrhythmia.107
Ablation for Polymorphic Ventricular Tachycardia and Fibrillation
Recurrent polymorphic VT causing “electrical storm” that is not due to ongoing acute ischemia is rare, but it occurs in idiopathic ventricular fibrillation, long QT syndrome, Brugada syndrome, and early and late after myocardial infarction.16,17,108,109 VT is often initiated by premature beats from one or a few foci that can be targeted for ablation if they occur with sufficient frequency. Sharp potentials consistent with Purkinje activation are often recorded from foci in the left or right ventricles. Less frequently, an RV outflow tract focus is a trigger. Arrhythmias can wax and wane. Immediate patient transport to the laboratory when the arrhythmia is active is warranted if ablation is to be attempted. In selected patients, approximately 90% of patients are free from recurrences during follow-up.16,17,108,109
In a small series of patients with Brugada syndrome and recurrent VF, epicardial mapping identified abnormal electrograms over the RV outflow tract, where ablation abolished recurrent VF.2
Transcoronary Ethanol Ablation
When endocardial and epicardial ablation attempts fail, transcoronary ethanol ablation can be considered.110 This approach requires identification and cannulation of a target artery that is supplying the VT substrate and injecting absolute ethanol to directly damage the myocardium, as well as the vessel. Tokuda et al.110 attempted this approach in 27 of 274 patients with VT related to structural heart disease. It was abandoned in five because of unsuitable anatomy; the targeted VT was acutely abolished in 82% of the remaining patients; and 9 of the 11 patients with prior VT storm remained free of VT storm. At least one VT recurred in 64% of patients, and mortality during follow-up was 32%. This technique continues to be reserved for patients who have failed other options.
References
1. Aliot, EM, Stevenson, WG, Almendral-Garrote, JM, et al. Ehra/hrs expert consensus on catheter ablation of ventricular arrhythmias: Developed in a partnership with the european heart rhythm association (EHRA), a registered branch of the european society of cardiology (ESC), and the heart rhythm society (HRS); in collaboration with the american college of cardiology (ACC) and the american heart association (AHA). Heart Rhythm. 2009; 6:886–933.
2. Nademanee, K, Veerakul, G, Chandanamattha, P, et al. Prevention of ventricular fibrillation episodes in brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011; 123:1270–1279.
3. Knecht, S, Sacher, F, Wright, M, et al. Long-term follow-up of idiopathic ventricular fibrillation ablation: A multicenter study. J Am Coll Cardiol. 2009; 54:522–528.
4. Stevenson, WG, Wilber, DJ, Natale, A, et al. Multicenter trial of irrigated rf ablation with electroanatomic mapping for ventricular tachycardia after myocardial infarction. Circulation. 2009; 110:1869.
5. Calkins, H, Epstein, A, Packer, D, et al. Catheter ablation of ventricular tachycardia in patients with structural heart disease using cooled radiofrequency energy: Results of a prospective multicenter study. Cooled rf multi center investigators group. J Am Coll Cardiol. 2000; 35:1905–1914.
6. Berruezo, A, Mont, L, Nava, S, et al. Electrocardiographic recognition of the epicardial origin of ventricular tachycardias. Circulation. 2004; 109:1842–1847.
7. Valles, E, Bazan, V, Marchlinski, FE. Ecg criteria to identify epicardial ventricular tachycardia in nonischemic cardiomyopathy. Circ Arrhythm Electrophysiol. 2010; 3:63–71.
8. Bazan, V, Gerstenfeld, EP, Garcia, FC, et al. Site-specific twelve-lead ecg features to identify an epicardial origin for left ventricular tachycardia in the absence of myocardial infarction. Heart Rhythm. 2007; 4:1403–1410.
9. Martinek, M, Stevenson, WG, Inada, K, et al. Qrs characteristics fail to reliably identify ventricular tachycardias that require epicardial ablation in ischemic heart disease. J Cardiovasc Electrophysiol. 2012; 23:188–193.
10. Merino, JL, Peinado, R, Fernandez-Lozano, I, et al. Bundle-branch reentry and the postpacing interval after entrainment by right ventricular apex stimulation: A new approach to elucidate the mechanism of wide-qrs-complex tachycardia with atrioventricular dissociation. Circulation. 2001; 103:1102–1108.
11. Yamada, T, Platonov, M, McElderry, HT, et al. Left ventricular outflow tract tachycardia with preferential conduction and multiple exits. Circ Arrhythm Electrophysiol. 2008; 1:140–142.
12. Yamada, T, McElderry, HT, Doppalapudi, H, et al. Idiopathic ventricular arrhythmias originating from the left ventricular summit: Anatomic concepts relevant to ablation. Circ Arrhythm Electrophysiol. 2010; 3:616–623.
13. Roberts-Thomson, KC, Steven, D, et al. Coronary artery injury due to catheter ablation in adults: Presentations and outcomes. Circulation. 2009; 120:1465–1473.
14. Tian, J, Jeudy, J, Smith, MF, et al. Three-dimensional contrast-enhanced multidetector ct for anatomic, dynamic, and perfusion characterization of abnormal myocardium to guide ventricular tachycardia ablations. Circ Arrhythm Electrophysiol. 2012; 3:496–504.
15. Dickfeld, T, Lei, P, Dilsizian, V, et al. Integration of three-dimensional scar maps for ventricular tachycardia ablation with positron emission tomography-computed tomography. JACC Cardiovasc Imaging. 2008; 1:73–82.
16. Szumowski, L, Sanders, P, Walczak, F, et al. Mapping and ablation of polymorphic ventricular tachycardia after myocardial infarction. J Am Coll Cardiol. 2004; 44:1700–1706.
17. Bansch, D, Oyang, F, Antz, M, et al. Successful catheter ablation of electrical storm after myocardial infarction. Circulation. 2003; 108:3011–3016.
18. Noda, T, Shimizu, W, Taguchi, A, et al. Malignant entity of idiopathic ventricular fibrillation and polymorphic ventricular tachycardia initiated by premature extrasystoles originating from the right ventricular outflow tract. J Am Coll Cardiol. 2005; 46:1288–1294.
19. Codreanu, A, Odille, F, Aliot, E, et al. Electroanatomic characterization of post-infarct scars comparison with 3-dimensional myocardial scar reconstruction based on magnetic resonance imaging. J Am Coll Cardiol. 2008; 52:839–842.
20. Nazarian, S, Bluemke, DA, Lardo, AC, et al. Magnetic resonance assessment of the substrate for inducible ventricular tachycardia in nonischemic cardiomyopathy. Circulation. 2005; 112:2821–2825.
21. Dickfeld, T, Tian, J, Ahmad, G, et al. Mri-guided ventricular tachycardia ablation: Integration of late gadolinium-enhanced 3d scar in patients with implantable cardioverter-defibrillators. Circ Arrhythm Electrophysiol. 2011; 4:172–184.
22. Bala, R, Ren, JF, Hutchinson, MD, et al. Assessing epicardial substrate using intracardiac echocardiography during vt ablation. Circ Arrhythm Electrophysiol. 2011; 4:667–673.
23. Marchlinski, FE. Perivalvular fibrosis and monomorphic ventricular tachycardia: Toward a unifying hypothesis in nonischemic cardiomyopathy. Circulation. 2007; 116:1998–2001.
24. Marchlinski, FE, Zado, E, Dixit, S, et al. Electroanatomic substrate and outcome of catheter ablative therapy for ventricular tachycardia in setting of right ventricular cardiomyopathy. Circulation. 2004; 110:2293–2298.
25. Soejima, K, Stevenson, WG, Maisel, WH, et al. Electrically unexcitable scar mapping based on pacing threshold for identification of the reentry circuit isthmus: Feasibility for guiding ventricular tachycardia ablation. Circulation. 2002; 106:1678–1683.
26. de Chillou, C, Lacroix, D, Klug, D, et al. Isthmus characteristics of reentrant ventricular tachycardia after myocardial infarction. Circulation. 2002; 105:726–731.
27. Soejima, K, Suzuki, M, Maisel, WH, et al. Catheter ablation in patients with multiple and unstable ventricular tachycardias after myocardial infarction: Short ablation lines guided by reentry circuit isthmuses and sinus rhythm mapping. Circulation. 2001; 104:664–669.
28. Marchlinski, FE, Callans, DJ, Gottlieb, CD, et al. Linear ablation lesions for control of unmappable ventricular tachycardia in patients with ischemic and nonischemic cardiomyopathy. Circulation. 2000; 101:1288–1296.
29. Klemm, HU, Ventura, R, Steven, D, et al. Catheter ablation of multiple ventricular tachycardias after myocardial infarction guided by combined contact and noncontact mapping. Circulation. 2007; 115:2697–2704.
30. Della Bella, P, Riva, S, Fassini, G, et al. Incidence and significance of pleomorphism in patients with postmyocardial infarction ventricular tachycardia. Acute and long-term outcome of radiofrequency catheter ablation. Eur Heart J. 2004; 25:1127–1138.
31. Bogun, F, Li, YG, Groenefeld, G, et al. Prevalence of a shared isthmus in postinfarction patients with pleiomorphic, hemodynamically tolerated ventricular tachycardias. J Cardiovasc Electrophysiol. 2002; 13:237–241.
32. Cesario, DA, Vaseghi, M, Boyle, NG, et al. Value of high-density endocardial and epicardial mapping for catheter ablation of hemodynamically unstable ventricular tachycardia. Heart Rhythm. 2006; 3:1–10.
33. Reddy, VY, Neuzil, P, Taborsky, M, et al. Short-term results of substrate mapping and radiofrequency ablation of ischemic ventricular tachycardia using a saline-irrigated catheter. J Am Coll Cardiol. 2003; 41:2228–2236.
34. Perez-David, E, Arenal, A, Rubio-Guivernau, JL, et al. Noninvasive identification of ventricular tachycardia-related conducting channels using contrast-enhanced magnetic resonance imaging in patients with chronic myocardial infarction: Comparison of signal intensity scar mapping and endocardial voltage mapping. J Am Coll Cardiol. 2011; 57:184–194.
35. Wijnmaalen, AP, van der Geest, RJ, van Huls van Taxis, CF, et al. Head-to-head comparison of contrast-enhanced magnetic resonance imaging and electroanatomical voltage mapping to assess post-infarct scar characteristics in patients with ventricular tachycardias: Real-time image integration and reversed registration. Eur Heart J. 2011; 32:104–114.
36. Cano, O, Hutchinson, M, Lin, D, et al. Electroanatomic substrate and ablation outcome for suspected epicardial ventricular tachycardia in left ventricular nonischemic cardiomyopathy. J Am Coll Cardiol. 2009; 54:799–808.
37. Garcia, FC, Bazan, V, Zado, ES, et al. Epicardial substrate and outcome with epicardial ablation of ventricular tachycardia in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2009; 120:366–375.
38. Hutchinson, MD, Gerstenfeld, EP, Desjardins, B, et al. Endocardial unipolar voltage mapping to detect epicardial ventricular tachycardia substrate in patients with nonischemic left ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2011; 4:49–55.
39. Haqqani, HM, Tschabrunn, CM, Tzou, WS, et al. Isolated septal substrate for ventricular tachycardia in nonischemic dilated cardiomyopathy: Incidence, characterization, and implications. Heart Rhythm. 2011; 8:1169–1176.
40. Polin, GM, Haqqani, H, Tzou, W, et al. Endocardial unipolar voltage mapping to identify epicardial substrate in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Heart Rhythm. 2011; 8:76–83.
41. Volkmer, M, Ouyang, F, Deger, F, et al. Substrate mapping vs. Tachycardia mapping using carto in patients with coronary artery disease and ventricular tachycardia: Impact on outcome of catheter ablation. Europace. 2006; 8:968–976.
42. Brunckhorst, CB, Delacretaz, E, Soejima, K, et al. Identification of the ventricular tachycardia isthmus after infarction by pace mapping. Circulation. 2004; 110:652–659.
43. Kottkamp, H, Wetzel, U, Schirdewahn, P, et al. Catheter ablation of ventricular tachycardia in remote myocardial infarction: Substrate description guiding placement of individual linear lesions targeting noninducibility. J Cardiovasc Electrophysiol. 2003; 14:675–681.
44. Arenal, A, del Castillo, S, Gonzalez-Torrecilla, E, et al. Tachycardia-related channel in the scar tissue in patients with sustained monomorphic ventricular tachycardias: Influence of the voltage scar definition. Circulation. 2004; 110:2568–2574.
45. Hsia, HH, Lin, D, Sauer, WH, et al. Anatomic characterization of endocardial substrate for hemodynamically stable reentrant ventricular tachycardia: Identification of endocardial conducting channels. Heart Rhythm. 2006; 3:503–512.
46. Nakahara, S, Tung, R, Ramirez, RJ, et al. Characterization of the arrhythmogenic substrate in ischemic and nonischemic cardiomyopathy implications for catheter ablation of hemodynamically unstable ventricular tachycardia. J Am Coll Cardiol. 2010; 55:2355–2365.
47. Jais, P, Maury, P, Khairy, P, et al. Elimination of local abnormal ventricular activities: A new end point for substrate modification in patients with scar-related ventricular tachycardia. Circulation. 2012; 125:2184–2196.
48. Bogun, F, Good, E, Reich, S, et al. Isolated potentials during sinus rhythm and pace-mapping within scars as guides for ablation of post-infarction ventricular tachycardia. J Am Coll Cardiol. 2006; 47:2013–2019.
49. Kuhne, M, Abrams, G, Sarrazin, JF, et al. Isolated potentials and pace-mapping as guides for ablation of ventricular tachycardia in various types of nonischemic cardiomyopathy. J Cardiovasc Electrophysiol. 2010; 21:1017–1023.
50. Vergara, P, Trevisi, N, Ricco, A, et al. Late potentials abolition as an additional technique for reduction of arrhythmia recurrence in scar related ventricular tachycardia ablation. J Cardiovasc Electrophysiol. 2012.
51. Bogun, F, Kim, HM, Han, J, et al. Comparison of mapping criteria for hemodynamically tolerated, postinfarction ventricular tachycardia. Heart Rhythm. 2006; 3:20–26.
52. Verma, A, Marrouche, NF, Schweikert, RA, et al. Relationship between successful ablation sites and the scar border zone defined by substrate mapping for ventricular tachycardia post-myocardial infarction. J Cardiovasc Electrophysiol. 2005; 16:465–471.
53. Bunch, TJ, Darby, A, May, HT, et al. Efficacy and safety of ventricular tachycardia ablation with mechanical circulatory support compared with substrate-based ablation techniques. Europace. 2012; 14:709–714.
54. Miller, MA, Dukkipati, SR, Mittnacht, AJ, et al. Activation and entrainment mapping of hemodynamically unstable ventricular tachycardia using a percutaneous left ventricular assist device. J Am Coll Cardiol. 2011; 58:1363–1371.
55. Bogun, F, Knight, B, Goyal, R, et al. Discrete systolic potentials during ventricular tachycardia in patients with prior myocardial infarction. J Cardiovasc Electrophysiol. 1999; 10:364–369.
56. Segal, OR, Chow, AW, Markides, V, et al. Long-term results after ablation of infarct-related ventricular tachycardia. Heart Rhythm. 2005; 2:474–482.
57. Della Bella, P, Pappalardo, A, Riva, S, et al. Non-contact mapping to guide catheter ablation of untolerated ventricular tachycardia. Eur Heart J. 2002; 23:742–752.
58. Strickberger, SA, Knight, BP, Michaud, GF, et al. Mapping and ablation of ventricular tachycardia guided by virtual electrograms using a noncontact, computerized mapping system. J Am Coll Cardiol. 2000; 35:414–421.
59. Stevenson, WG, Khan, H, Sager, P, et al. Identification of reentry circuit sites during catheter mapping and radiofrequency ablation of ventricular tachycardia late after myocardial infarction. Circulation. 1993; 88:1647–1670.
60. Henthorn, RW, Okumura, K, Olshansky, B, et al. A fourth criterion for transient entrainment: The electrogram equivalent of progressive fusion. Circulation. 1988; 77:1003–1012.
61. Tung, S, Soejima, K, Maisel, WH, et al. Recognition of far-field electrograms during entrainment mapping of ventricular tachycardia. J Am Coll Cardiol. 2003; 42:110–115.
62. Hadjis, TA, Harada, T, Stevenson, WG, et al. Effect of recording site on postpacing interval measurement during catheter mapping and entrainment of postinfarction ventricular tachycardia. J Cardiovasc Electrophysiol. 1997; 8:398–404.
63. Soejima, K, Stevenson, WG, Maisel, WH, et al. The n + 1 difference: A new measure for entrainment mapping. J Am Coll Cardiol. 2001; 37:1386–1394.
64. Stevenson, WG, Friedman, PL, Sager, PT, et al. Exploring postinfarction reentrant ventricular tachycardia with entrainment mapping. J Am Coll Cardiol. 1997; 29:1180–1189.
65. Bogun, F, Krishnan, SC, Marine, JE, et al. Catheter ablation guided by termination of postinfarction ventricular tachycardia by pacing with nonglobal capture. Heart Rhythm. 2004; 1:422–426.
66. Lopera, G, Stevenson, WG, Soejima, K, et al. Identification and ablation of three types of ventricular tachycardia involving the his-purkinje system in patients with heart disease. J Cardiovasc Electrophysiol. 2004; 15:52–58.
67. Hayashi, M, Kobayashi, Y, Iwasaki, YK, et al. Novel mechanism of postinfarction ventricular tachycardia originating in surviving left posterior purkinje fibers. Heart Rhythm. 2006; 3:908–918.
68. Bogun, F, Good, E, Reich, S, et al. Role of purkinje fibers in post-infarction ventricular tachycardia. J Am Coll Cardiol. 2006; 48:2500–2507.
69. Delacretaz, E, Soejima, K, Brunckhorst, CB, et al. Assessment of radiofrequency ablation effect from unipolar pacing threshold. Pacing Clin Electrophysiol. 2003; 26:1993–1996.
70. Della Bella, P, Riva, S, Fassini, G, et al. Long-term follow-up after radiofrequency catheter ablation of atrial fibrillation: Role of the acute procedure outcome and of the clinical presentation. Europace. 2005; 7:95–103.
71. O’Donnell, D, Bourke, JP, Furniss, SS. Standardized stimulation protocol to predict the long-term success of radiofrequency ablation of postinfarction ventricular tachycardia. Pacing Clin Electrophysiol. 2003; 26:348–351.
72. Deneke, T, Grewe, PH, Lawo, T, et al. Substrate-modification using electroanatomical mapping in sinus rhythm to treat ventricular tachycardia in patients with ischemic cardiomyopathy. Z Kardiol. 2005; 94:453–460.
73. van der Burg, AE, de Groot, NM, van Erven, L, et al. Long-term follow-up after radiofrequency catheter ablation of ventricular tachycardia: A successful approach? J Cardiovasc Electrophysiol. 2002; 13:417–423.
74. Della Bella, P, De Ponti, R, Uriarte, JA, et al. Catheter ablation and antiarrhythmic drugs for haemodynamically tolerated post-infarction ventricular tachycardia; long-term outcome in relation to acute electrophysiological findings. Eur Heart J. 2002; 23:414–424.
75. Kosmidou, I, Inada, K, Seiler, J, et al. Role of repeat procedures for catheter ablation of postinfarction ventricular tachycardia. Heart Rhythm. 2011; 8:1516–1522.
76. Schmidt, B, Chun, KR, Baensch, D, et al. Catheter ablation for ventricular tachycardia after failed endocardial ablation: Epicardial substrate or inappropriate endocardial ablation? Heart Rhythm. 2010; 7:1746–1752.
77. Soejima, K, Stevenson, WG, Sapp, JL, et al. Endocardial and epicardial radiofrequency ablation of ventricular tachycardia associated with dilated cardiomyopathy: The importance of low-voltage scars. J Am Coll Cardiol. 2004; 43:1834–1842.
78. Valles, E, Bazan, V, Marchlinski, FE. Ecg criteria to identify epicardial ventricular tachycardia in nonischemic cardiomyopathy. Circ Arrhythm Electrophysiol. 2010; 3:63–71.
79. Miljoen, H, State, S, de Chillou, C, et al. Electroanatomic mapping characteristics of ventricular tachycardia in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Europace. 2005; 7:516–524.
80. Dinov, B, Schonbauer, R, Wojdyla-Hordynska, A, et al. Long-term efficacy of single procedure remote magnetic catheter navigation for ablation of ischemic ventricular tachycardia: A retrospective study. J Cardiovasc Electrophysiol. 2012; 23:499–505.
81. Deneke, T, Lawo, T, Grewe, PH, et al. Usefulness of a limited linear ablation of post-myocardial infarction ventricular tachycardia using a standardized approach based on sinus rhythm mapping. Am J Cardiol. 2010; 105:1235–1239.
82. Sosa, E, Scanavacca, M, d’Avila, A, et al. Nonsurgical transthoracic epicardial catheter ablation to treat recurrent ventricular tachycardia occurring late after myocardial infarction. J Am Coll Cardiol. 2000; 35:1442–1449.
83. Brugada, J, Berruezo, A, Cuesta, A, et al. Nonsurgical transthoracic epicardial radiofrequency ablation: An alternative in incessant ventricular tachycardia. J Am Coll Cardiol. 2003; 41:2036–2043.
84. Sauer, WH, Zado, E, Gerstenfeld, EP, et al. Incidence and predictors of mortality following ablation of ventricular tachycardia in patients with an implantable cardioverter-defibrillator. Heart Rhythm. 2010; 7:9–14.
85. Nabar, A, Rodriguez, LM, Batra, RK, et al. Echocardiographic predictors of survival in patients undergoing radiofrequency ablation of postinfarct clinical ventricular tachycardia. J Cardiovasc Electrophysiol. 2002; 13:S118–S121.
86. Moss, AJ, Greenberg, H, Case, RB, et al. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation. 2004; 110:3760–3765.
87. Khan, HH, Maisel, WH, Ho, C, et al. Effect of radiofrequency catheter ablation of ventricular tachycardia on left ventricular function in patients with prior myocardial infarction. J Interv Card Electrophysiol. 2002; 7:243–247.
88. Kuck, KH, Schaumann, A, Eckardt, L, et al. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): A multicentre randomised controlled trial. Lancet. 2010; 375:31–40.
89. Reddy, VY, Reynolds, MR, Neuzil, P, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007; 357:2657–2665.
90. Dello Russo, A, Casella, M, Pieroni, M, et al. Drug-refractory ventricular tachycardias following myocarditis: Endocardial and epicardial radiofrequency catheter ablation. Circ Arrhythm Electrophysiol. 2012.
91. Hsia, HH, Callans, DJ, Marchlinski, FE. Characterization of endocardial electrophysiological substrate in patients with nonischemic cardiomyopathy and monomorphic ventricular tachycardia. Circulation. 2003; 108:704–710.
92. Satomi, K, Kurita, T, Suyama, K, et al. Catheter ablation of stable and unstable ventricular tachycardias in patients with arrhythmogenic right ventricular dysplasia. J Cardiovasc Electrophysiol. 2006; 17:469–476.
93. Koplan, BA, Soejima, K, Baughman, K, et al. Refractory ventricular tachycardia secondary to cardiac sarcoid: Electrophysiologic characteristics, mapping, and ablation. Heart Rhythm. 2006; 3:924–929.
94. Verma, A, Kilicaslan, F, Schweikert, RA, et al. Short- and long-term success of substrate-based mapping and ablation of ventricular tachycardia in arrhythmogenic right ventricular dysplasia. Circulation. 2005; 111:3209–3216.
95. O’Donnell, D, Cox, D, Bourke, J, et al. Clinical and electrophysiological differences between patients with arrhythmogenic right ventricular dysplasia and right ventricular outflow tract tachycardia. Eur Heart J. 2003; 24:801–810.
96. Bai, R, Di Biase, L, Shivkumar, K, et al. Ablation of ventricular arrhythmias in arrhythmogenic right ventricular dysplasia/cardiomyopathy: Arrhythmia-free survival after endo-epicardial substrate based mapping and ablation. Circ Arrhythm Electrophysiol. 2011; 4:478–485.
97. Berruezo, A, Fernandez-Armenta, J, Mont, L, et al. Combined endocardial and epicardial catheter ablation in arrhythmogenic right ventricular dysplasia incorporating scar dechanneling technique. Circ Arrhythm Electrophysiol. 2012; 5:111–121.
98. Corrado, D, Basso, C, Leoni, L, et al. Three-dimensional electroanatomic voltage mapping increases accuracy of diagnosing arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2005; 111:3042–3050.
99. Tandri, H, Saranathan, M, Rodriguez, ER, et al. Noninvasive detection of myocardial fibrosis in arrhythmogenic right ventricular cardiomyopathy using delayed-enhancement magnetic resonance imaging. J Am Coll Cardiol. 2005; 45:98–103.
100. Haqqani, HM, Tschabrunn, CM, Betensky, BP, et al. Layered activation of epicardial scar in arrhythmogenic right ventricular dysplasia: Possible substrate for confined epicardial circuits. Circ Arrhythm Electrophysiol. 2012.
101. Della Bella, P, Brugada, J, Zeppenfeld, K, et al. Epicardial ablation for ventricular tachycardia: A european multicenter study. Circ Arrhythm Electrophysiol. 2011; 4:653–659.
102. Dalal, D, Jain, R, Tandri, H, et al. Long-term efficacy of catheter ablation of ventricular tachycardia in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Am Coll Cardiol. 2007; 50:432–440.
103. Pokushalov, E, Romanov, A, Turov, A, et al. Percutaneous epicardial ablation of ventricular tachycardia after failure of endocardial approach in the pediatric population with arrhythmogenic right ventricular dysplasia. Heart Rhythm. 2010; 7:1406–1410.
104. Morwood, JG, Triedman, JK, Berul, CI, et al. Radiofrequency catheter ablation of ventricular tachycardia in children and young adults with congenital heart disease. Heart Rhythm. 2004; 1:301–308.
105. Zeppenfeld, K, Schalij, M, Bartelings, MM, et al. Catheter ablation of ventricular tachycardia after repair of congenital heart disease electroanatomical identification of the critical right ventricular isthmus. Circulation. 2007; 116:2241–2252.
106. Inada, K, Seiler, J, Roberts-Thomson, KC, et al. Substrate characterization and catheter ablation for monomorphic ventricular tachycardia in patients with apical hypertrophic cardiomyopathy. J Cardiovasc Electrophysiol. 2011; 22:41–48.
107. Cantillon, DJ, Bianco, C, Wazni, OM, et al. Electrophysiologic characteristics and catheter ablation of ventricular tachyarrhythmias among patients with heart failure on ventricular assist device support. Heart Rhythm. 2012; 9:859–864.
108. Haissaguerre, M, Extramiana, F, Hocini, M, et al. Mapping and ablation of ventricular fibrillation associated with long-qt and brugada syndromes. Circulation. 2003; 108:925–928.
109. Marrouche, NF, Verma, A, Wazni, O, et al. Mode of initiation and ablation of ventricular fibrillation storms in patients with ischemic cardiomyopathy. J Am Coll Cardiol. 2004; 43:1715–1720.
110. Tokuda, M, Sobieszczyk, P, Eisenhauer, AC, et al. Transcoronary ethanol ablation for recurrent ventricular tachycardia after failed catheter ablation: An update. Circ Arrhythm Electrophysiol. 2011; 4:889–896.
111. Stevenson, WG, Soejima, K. Catheter ablation for ventricular tachycardia. Circulation. 2007; 115:2750–2760.
112. Harada, T, Stevenson, WG, Kocovic, DZ, et al. Catheter ablation of ventricular tachycardia after myocardial infarction: relation of endocardial sinus rhythm late potentials to the reentry circuit. J Am Coll Cardiol. 1997; 30:1015–1023.







