33 Care of the ophthalmic surgical patient
Amblyopia: Condition in which there is a lack of development of central vision in one eye because of a failure in using both eyes simultaneously (“lazy eye”). It primarily develops before 6 years of age and can have complete recovery with early diagnosis and treatment. Treatment is a combination therapy approach with prescriptive lenses, eye patching, prisms, and vision therapy.
Anterior Segment: The anterior one-third segment of the globe, extending from the anterior hyaloid face filled with aqueous fluid.
Blepharophimosis: Abnormal narrowing of the palpebral fissures or eye lids.
Blepharoplasty: Removal of excess tissue, fatty deposits, or tightening of the skeletal muscle from the upper or lower eyelids to increase range of vision by reduced sagging of excess skin.
Cataract: An opacity clouding that is found most commonly in the lens and the cortex of the eye.
Chalazion: A small eyelid cyst that is a result of chronic inflammation of a meibomian gland.
Choroid: The spongelike vascular membrane in the globe between the sclera and the retina, supplying nutrients to the retina.
Choroidal Melanoma: A rare form of cancer found in the spongelike vascular membrane of the eye. It is the most common form of cancer of the eye in the adult population.
Ciliary Body: A ring of tissue that encircles the lens of the eye, containing smooth muscle fibers and capillaries.
Ciliary Muscle: Smooth muscle fibers located in the ciliary body that control the shape of the lens.
Ciliary Process: Pigmented ridges located in the smooth muscle fibers surrounding the lens that contain capillaries that secrete aqueous humor into the anterior segment of the eye.
Dacryocystitis: Infection of the lacrimal sac.
Dacryocystorhinostomy: A procedure in which a new pathway is created from the lacrimal sac to the nasal passageway.
Deep Lamellar Endothelial Keratoplasty: Transplantation of the cornea in which the epithelium of the cornea is replaced without an incision in the anterior corneal surface.
Dermatochalasis: Excess tissue, fatty deposits, or excess relaxation of the skeletal muscle of the upper or lower eyelids.
Descemet’s Stripping Endothelial Keratoplasty: Transplantation of the corneal inner endothelium and its underlying membrane via two small incisions.
Ectropian: Eversion of the eyelid (typically the lower lid). Surgical correction is performed by horizontally shortening the lid.
Entropian: Inversion of the eyelid (typically the lower lid), which causes the eyelashes to continually rub against the surface of the eye. Surgical treatment is performed by one of two ways, both of which anastomose the lid after removing a small section of the skin, muscle, and tendon.
Enucleation: Complete removal of the eye globe.
Epiphora: Excessive tear production. Can be caused by secondary lacrimal duct obstruction.
Evisceration of the Eye: Removal of the entire contents of the eye globe, leaving the sclera and extraocular muscles intact.
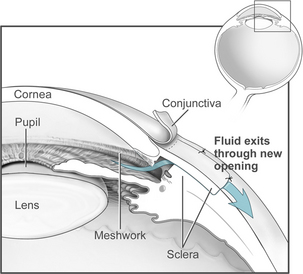
Glaucoma: A family of eye diseases characterized by increased intraocular pressure resulting in permanent optic nerve damage and visual loss. Surgical treatment is aimed at reestablishing the outflow of aqueous fluid. Nearly all procedures are so-called filtration operations (e.g., trabeculectomy or tube shunt procedures).
Goniotomy: A surgical procedure for congenital glaucoma in which a 90- to 120-degree arc incision is made within the anterior trabecular meshwork of the eye.
Hydroxyapatite Implant: An implant that is a complex calcium phosphate salt made from coral. Placed after an enucleation, the implant is less likely to be rejected because of its resemblance of human bone in its chemical and porous properties. The orbital tissues are attached directly and a prosthesis placed over it. The implant becomes integrated over time with blood vessels and tissue, thus allowing for a more realistic appearance and movement.
Intraocular Lens Implant (IOL): An artificial lens implanted to replace the crystalline lens after removal in cataract surgery. IOLs are made in a variety of styles and from a variety of materials. One of the newest and smallest multifocal IOLs is a pliable, foldable lens that can be inserted through an incision of 1.4 mm or smaller.
Keratoplasty: Replacement of the diseased, central portion of the cornea with donor tissue. A cookie-cutter–like trephine is used on both the donor and recipient cornea.
Lacrimal Punctum: The opening of the lacrimal duct at either the upper or lower eyelid at the inner canthus of the eye.
Laser-Assisted In Situ Keratomileusis (LASIK): A surgical procedure used to correct nearsightedness (myopia), farsightedness (hyperopia), and astigmatism in which an excimer laser is used to remove inner layers of cornea tissue, thereby reshaping it.
Miosis: Contraction of the pupil induced by light or eye drops.
Mydriasis: Dilation of the pupils usually induced by eye drops, but also induced by lack of light.
Oculocardiac Reflex (OCR): A sudden onset bradycardia elicited by traction on the extraocular muscles, especially the medial rectus, or by direct pressure on the eye globe. This reflex is a trigeminovagal reflex arc. It can also cause cardiac dysrhythmias such as ventricular ectopy, sinus arrest, and ventricular fibrillation. The pediatric population is especially sensitive to OCR.
Phacoemulsification: Fragmentation and removal of the lens with ultrasonic vibrations while aspirating during cataract surgery.
Plaque Therapy: A highly concentrated radiation implant most commonly used in the treatment of choroidal melanoma.
Presbyopia: A condition associated with aging whereby the lens loses its flexibility and the ability to focus on objects up close.
Proliferative Diabetic Retinopathy: The latter stages of diabetic retinopathy in which a proliferative growth of abnormal new blood vessels develop from the retina. These vessels can lead to vitreous hemorrhages and detachment of the retina.
Proptosis or Exophthalmos: Protrusion of the eyeball.
Pterygium: A benign growth of the conjunctiva that extends to the cornea at approximately a 3 o’clock or a 9 o’clock position. It is caused by excessive exposure to ultraviolet light (sunlight) or wind. Excision becomes necessary when visual disturbances become present.
Ptosis: Drooping of the upper eyelid. Surgery involves various procedures on the upper eyelid and/or the levator muscle.
Retinoblastoma: A malignant tumor of the retina that occurs predominantly in early childhood.
Retinopexy: Surgical procedure to correct a retinal tear. This is done by causing scar formation to occur with the use of laser photocoagulation, electric current, or cryotherapy.
Scleral Buckle: A piece of silicone plastic or sponge material that is surgically sewn onto the sclera in order to correct a retinal detachment via compression of the sclera against the retina. This procedure is often used in conjunction with a retinopexy, often with a pars plana vitrectomy.
Strabismus: A condition in which the eyes are not properly aligned and the extraocular muscles lack coordinated muscle movements. Inward deviation is called esotropia, and outward deviation is called exotropia. Surgical correction is performed by either shortening and removal of part of the tendon or lengthening a muscle via transfer of the muscle insertion site posterior to the original attachment point on the eye. It is occasionally treated with glasses or drops; however, it can lead to amblyopia if not treated in a timely manner.
Tonometer: An instrument used for the measurement of intraocular pressure. Can be hand-held or mounted to a slit lamp microscope. Requires topical anesthesia via eye drops, unless a noncontact “air pull” instrument is used.
Trabecular Meshwork: A ring of spongelike tissue through which aqueous humor drains to control the intraocular pressure.
Trabeculectomy: A surgical procedure to create a drainage channel from the anterior chamber to the subconjunctival space to lower intraocular pressure, for treatment of uncontrolled glaucoma.
Vitrectomy: Surgical removal of the vitreous gel within the eye. Performed to clear blood that is occluding vision, to sever vitreous traction bands that are pulling on the retina, or to help with the repair of a retinal detachment. The removed vitreous is replaced with fluid, specialized gas, or silicone oil.
Vitreous Fluid: A clear, jellylike substance that fills the posterior chamber of the eye.
Vitreous Hemorrhage: Bleeding within the vitreous fluid that is usually the result of proliferative diabetic retinopathy, a retinal tear, detachment, or trauma.
Zonule of Zinn: A ring of fibrous strands that connects the ciliary processes with the crystalline lens of the eye. The eye focuses (accommodates) by the ciliary muscle exerting traction on the zonules, thereby changing the shape of the lens.
Caring for the ophthalmic surgical patient offers unique challenges to the perianesthesia nurse. It requires a thorough understanding of not only the surgical aspect of the patient’s care, but also the pharmacologic, physiologic, and emotional concerns. As the need for maintaining quality patient care and controlling overall medical costs continues to grow, many surgical advances have taken the most complex of ophthalmic procedures from hospital-based operating rooms to free-standing ambulatory surgery centers, thus enabling more patients to return home within 24 hours of surgery.1 This trend alone necessitates that the perianesthesia nurse have a fundamental knowledge base to anticipate an array of patients’ preoperative and postoperative needs. Recognizing and treating a variety of complex symptoms and complications, providing sufficient patient education, and planning discharge are just a few of the many needs with which the perianesthesia nurse will have to contend on a daily basis. Ophthalmic surgical patients vary widely in age. Any age-appropriate special needs or medical concerns should be identified by the perianesthesia nurse during the preadmission evaluation time. Knowledge of comorbidities in elderly patients becomes even more important when the amount of time with each patient is limited. Hypertension, diabetes mellitus, coronary artery, cerebral vascular, and renal disease are just a few examples. Despite the fact that ophthalmic surgery is most common in the elderly, advances in anesthesia, surgical techniques, and surgical instrumentation have allowed the most sophisticated procedures to be performed on the most fragile of the pediatric population (i.e., premature infants and neonates).2 Normal growth and development in the pediatric patient should be assessed and any variances should be noted. These comorbidities and other factors may predispose patients to sudden and potentially life-threatening postoperative complications.3 Close attention to the preoperative assessment is of utmost importance. Working with this wide range in patient population, certifications in advanced cardiac life support (ACLS) and pediatric advanced life support (PALS) are essential in the educational foundation for the perianesthesia nurse.
Preoperative evaluation
Preadmission evaluations are a critical tool for the perianesthesia nurse. Many hospitals and free-standing ambulatory surgery facilities have established preadmission testing clinics with guidelines designed for this purpose. The goals of the preoperative evaluation in the surgical patient is to obtain informed consent, perform physical assessments, arrange for laboratory tests and any necessary consultations, prescreen for any diseases, and provide patient education to reduce patient and caregiver anxiety. Upon evaluation, if the need for further medical testing arises, the patient can then be referred to their primary care physician or to a subspecialty to obtain medical clearance.4 A preadmission evaluation can decrease cancellations, provide ample time to establish rapport, and assess for any psychological or psychosocial needs that can be addressed before the actual day of surgery. In a 10-year observational study, Jiménez and colleagues5 concluded that 57.1% of surgical cases that were cancelled had a preventable or possibly preventable cause. With preadmission evaluations, this percentage can be greatly reduced, thereby decreasing the anxiety and frustration level of patients, caregivers, and health care team members on the day of surgery.
Ophthalmic medications
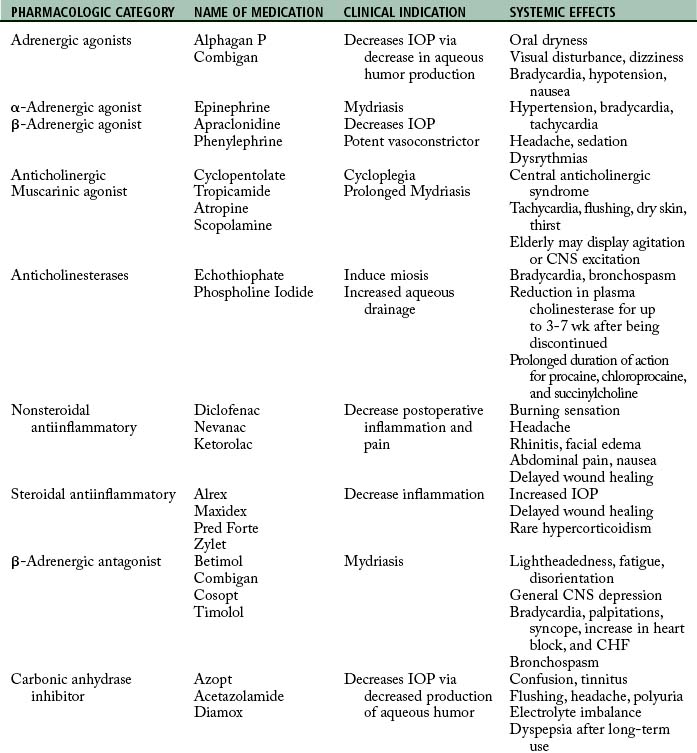
Most ophthalmic medications are administered topically in highly concentrated solutions (Table 33-1). Because of the highly vascular nature of the conjunctival sac and the nasolacrimal duct leading to the vascular mucosa of the nasopharynx, undesirable systemic effects can be caused by the rapid systemic absorption of topical solutions that are administered.6 These medications can also significantly alter a patient’s reaction to anesthetic drugs, thus causing changes in the intraocular dynamics.1 It is essential that the perianesthesia nurse learn to identify these medications and their potential systemic effects. The elderly patient is at higher risk for these severe systemic effects. This age group takes a higher number of prescription medications and undergoes a higher percentage of eye surgeries than any other age group.7
In order to easily identify the specific classifications of topical ocular medications, the American Academy of Ophthalmology (AAO), with input from pharmaceutical companies and the U.S. Food and Drug Administration (FDA), developed a universal color-coding system to distinguish between all topical ophthalmic medications. The color-coded system identifies every pharmaceutical class with its own unique cap-and-label color scheme (Table 33-2). With the introduction and implementation of the voluntary color-coding system, the AAO expects to “decrease the amount of serious adverse events resulting from patients (and medical personnel) difficulty in distinguishing between various ocular medications.”8 The threefold partnership of voluntary cooperation between the FDA, the pharmaceutical industry, and the AAO has proved effective and advantageous in the primary interest of patient safety since its inception.
| CLASS | COLOR |
|---|---|
| Adrenergic agonists | Purple |
| Antiinfectives, antimicrobials, antivirals, antifungals | Tan |
| Antiinflammatories, steroids | Pink |
| β-Blockers | Yellow |
| β-Blocker combinations | Dark Blue |
| Carbonic anhydrase inhibitors | Orange |
| Miotics | Dark Green |
| Mydriatics and cycloplegics | Red |
| Nonsteroidal antiinflammatories | Gray |
| Prostaglandin analogues | Turquoise |
Preoperative phase
Patients undergoing eye surgery have more apprehension and will need more constant verbal communication and reassurance.9 Using this opportunity, the perianesthesia nurse should review any preoperative education and postoperative instructions with the patient and any caregivers present. Expectations regarding the operative procedure’s outcome should also be explored. It is important that the patient and caregiver have realistic expectations. The more information and education that can be given to a patient and caregiver about the anticipated perioperative and postoperative course, the less amount of anxiety the patient will have and the fewer antianxiety medications that will be required.10 All preoperative lab work, medical tests, and clearance letters should be reviewed to ensure that all paperwork is in order and placed on the chart. The nurse should also verify each patient’s name, the operative eye, and procedure to be performed. Planned preoperative medications should be discussed. Depending on the type of ophthalmic procedure to be performed, ophthalmic medications may be administered in the preoperative holding area. A significant reduction of systemic absorption can be achieved by occluding the nasolacrimal duct by pressing on the inner canthus of the eye or closing the eyelids for at least 3 minutes immediately following the administration of ophthalmic medications. Doing so will reduce the chances of undesirable systemic side effects.1
Anesthetic options
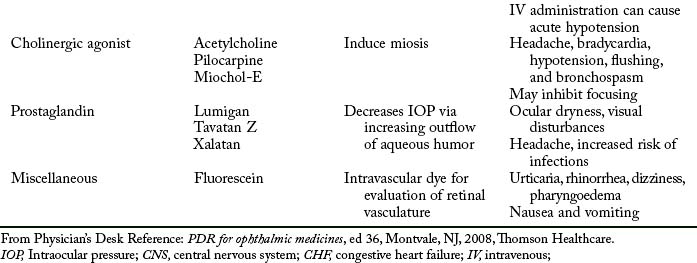
Local anesthesia can range from the topical instillation of 0.5% tetracaine anesthetic drops to an injection of a local anesthetic. A patient with a relatively quick surgeon performing a simple anterior chamber cataract removal (Fig. 33-1), intraocular lens implantation (Fig. 33-2), or glaucoma procedure (Fig. 33-3) could have a topical anesthetic, provided the patient is cooperative. Intracorneal anesthesia is also used for cataract surgery. The surgeon injects a local anesthetic directly into the anterior chamber of the cornea where anesthesia is needed. The most common regional anesthetic techniques used in eye surgical cases are the peribulbar and retrobulbar blocks. These blocks are performed by the surgeon or the anesthesia provider after sufficient sedation has been given. A 23- to 25-gauge retrobulbar (blunt-tipped) needle is used to inject 2 to 5 mL of local anesthetic either into the peribulbar or retrobulbar space. Lidocaine 2% and bupivacaine 0.75% are the most common local anesthetics used. Epinephrine (1:200,000 or 1:400,000) may be premixed into the local anesthetic to cause vasoconstriction of the blood vessels, thus reducing bleeding and decreasing the absorption rate of the local anesthetic. It is important that the perianesthesia nurse be aware of these techniques and potential side effects, because assistance may be needed with the application of a local anesthetic. An eye that has had a successful retrobulbar block will not move during head turning. Complications are rare but can include: hemorrhage, globe perforation, optic nerve injury, oculocardiac reflex, instantaneous convulsions, and respiratory arrest. Other local blocks used alone or in conjunction with the peribulbar or retrobulbar blocks are the subtenon block and the facial nerve block. It is imperative that the patient be closely monitored for any signs or symptoms of any complications while they are in the preoperative area.6
Perioperative phase
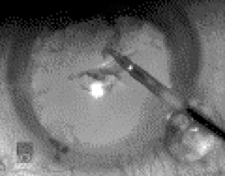
Numerous ophthalmic procedures are performed routinely. Most procedures are performed on an outpatient basis. A few exceptions include true ophthalmic emergencies such as chemical burns of the cornea, central retinal artery occlusion, open-globe injuries, endophthalmitis, acute narrow-angle glaucoma, acute retinal detachment (Fig. 33-4), corneal foreign body, and lid lacerations. These emergencies require surgical treatment within one to several hours. However, these procedures do not always necessitate an overnight admission to the hospital. If the patient is stable and able to meet discharge criteria, most physicians will discharge the patient, and schedule an appointment the following morning in the office. Semiurgent situations would include ocular tumors, blowout fractures of the orbit, congenital cataract (Fig. 33-5), and chronic retinal detachment. Treatment for these types of situations is usually started within days of the initial injury, but can be rescheduled for several weeks after an incident. Another reason for an overnight hospital admission would be for a prolonged procedure on a pediatric patient or a patient with an extensive medical history.2
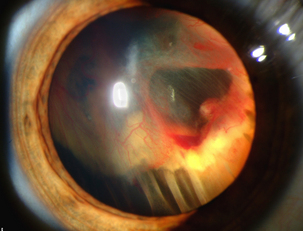
FIG. 33-4 Retinal detachment in Von Hippel-Lindau disease.
(Courtesy National Eye Institute, National Institutes of Health, Bethesda, Md.)
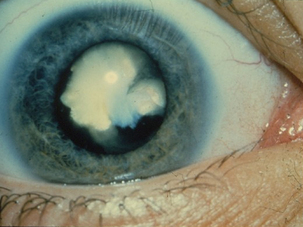
FIG. 33-5 A white congenital cataract.
(Courtesy National Eye Institute, National Institutes of Health, Bethesda, Md.)
Whatever the procedure to be performed, the risk of stimulating the oculocardiac reflex (OCR) is present. This reflex is a trigeminovagal reflex arc. It is elicited by traction on the extraocular muscles, especially the medial rectus muscle, or by placing pressure directly on the globe. This reflex causes a sudden bradycardia and cardiac dysrhythmias, such as ventricular ectopy, sinus arrest, or ventricular fibrillation. Hypotension will usually accompany this sudden decrease in heart rate. Atropine or glycopyrrolate given before surgery intravenously (IV) can often aid in preventing the reflex. OCR is most commonly seen during strabismus surgery in the pediatric population. The reflex can occur during certain retinal or glaucoma procedures during which traction is applied to the rectus muscles. Nevertheless, the reflex is still present at any age and can be triggered by any ophthalmic procedure. When the reflex occurs, cessation of the surgical stimulation should provide relief within 10 to 20 seconds. Atropine (10 to 20 mcg/kg) or glycopyrrolate (10 mcg/kg) can also be administered if bradycardia persists. The use of retrobulbar blocks can aid in reducing the incidence of OCR; however, the reflex can also be triggered at the time of placement of the regional blockade. OCR is self-limiting, in that when the stimulation has ceased, the bradycardia will end. When normal sinus rhythm has return within 10% of the baseline heart rate, it is safe to proceed.10
Postoperative phase
Upon arrival to the postanesthesia care unit (PACU), the anesthesia provider will give report to the PACU nurse. Report should include the procedure that was performed, any pertinent medical history of the patient, and any significant perioperative medications or events that have occurred. The PACU nurse will administer oxygen to the patient via a face mask and monitor the patient’s heart rate and rhythm, blood pressure, oxygen saturation, temperature, and level of consciousness. The patient’s condition will continually be monitored during this initial phase of recovery. The patient will typically respond to verbal stimuli and begin to follow commands within a short period of time. The level of postoperative care that a patient is required to have is determined by the “degree of underlying illness, the duration and complexity of anesthesia and surgery, and the risk of postoperative complications.”11
As the patient emerges from general or regional anesthesia with sedation, the incidence of postoperative nausea and vomiting (PONV) is higher in the ophthalmic surgical patient than in other surgical procedures.6,11 Other factors that can cause PONV are dehydration, hypotension, and pain. PONV avoidance should be a high priority. Antiemetics given perioperatively assist in decreasing the amount of PONV; however, ondansetron (2 to 4 mg IV) can be given as prophylaxis in the PACU, if not previously given.
If PONV persists, patients will not respond to a second dose of ondansetron because targeting an already blocked receptor is ineffective.2 Promethazine (12.5 to 25 mg IV) is the next optimal choice. Another virtually unknown alternative treatment was studied by Pellegrini and colleagues.12 In this comparison study, the inhalation of 70% isopropyl alcohol (IPA) from a standardized alcohol pad was used to successfully treat breakthrough PONV, after prophylactic treatment with ondansetron. The IPA group reported a faster time in reduction of PONV and an overall decrease in the antiemetic requirements. The implications of this study are fascinating, and the option of using IPA inhalational therapy for PONV is a viable one.
In a randomized controlled study, Pellegrini and colleagues12 evaluated the efficacy of using 70% isopropyl alcohol (IPA) in the treatment of postoperative nausea and vomiting (PONV) in two separate groups of patients that were high-risk for PONV. Patients were selected and randomly assigned into two different groups. Both groups received general anesthesia using similar medications and intravenous (IV) ondansetron intraoperatively before extubation. When the patients arrived in the postanesthesia care unit (PACU), the control group was given promethazine (12.5 to 25 mg IV) upon complaints of nausea. This dose could be repeated in 30 minutes up to a total dose of 50 mg IV. The experimental group of patients was treated with a commercially available 70% IPA pad upon complaints of nausea. The IPA pad was folded in half and placed 0.5 inches from the nares of the patient. The patient was then instructed to deeply inhale three times through their nose. The IPA treatments were to be given every 15 minutes for three applications. Demographics, a verbal numeric rating scale (VNRS) for nausea, the time it took to achieve a 50% reduction in the VNRS scores, and the overall antiemetic incidence of PONV per group were measured. The results showed no differences in the demographic variables or the baseline measurements between groups. There was a similar incidence in PONV between groups. However, the IPA group reported a faster overall time to 50% reduction in VNRS scores when compared to the control group. In addition, a decrease in the overall antiemetic requirements of the IPA group was noted.
Source: Pellegrini J, et al: Comparison of inhalation of isopropyl alcohol vs promethazine in the treatment of postoperative nausea and vomiting (PONV) in patients identified as at high risk for developing PONV, AANA J 77:293–299, 2009.
Not all ophthalmic surgical patients will have postoperative pain. Patients who receive examinations under anesthesia, cataract removal, nasolacrimal duct probing, and some glaucoma surgery, pain is usually minimal. Topical and regional anesthetics are beneficial in that they will typically last throughout the procedure and into the immediate postoperative period. This will allow the patient to progress rapidly into phase II of recovery, from which discharge will be possible within a short amount of time. These patients typically arrive in the PACU awake and alert.13 It is expected for those having longer ophthalmic procedures under general anesthesia to experience a moderate amount of pain. Opioid analgesics can cause nausea and vomiting, but the importance of controlling pain in the postoperative period takes priority. Opioid analgesics can also help to reduce coughing and decrease the incidence of emergence delirium in pediatric patients. Giving intravenous nonsteroidal antiinflammatory medications can also be a feasible option for controlling postoperative pain. Ketorolac (0.5 mg/kg) IV can be as effective as fentanyl (1 mcg/kg) or morphine (0.1 mg/kg) for postoperative pain in strabismus surgery patients without increasing PONV. Ketorolac has several advantages over opioids, in that it does not cause respiratory depression, sedation, or nausea and vomiting. A single dose will last approximately 6 to 8 hours. Conversely, ketorolac is eliminated through the kidneys and should not be given to patients with renal disease.11
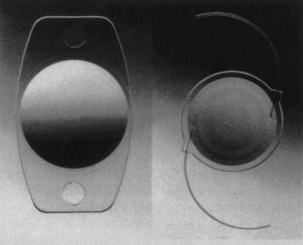
Depending on the procedure, the patient will usually have some type of sterile dressing or patch covered by an eye shield over the operative eye (Fig. 33-6). It is imperative that this dressing is not disturbed by the patient. Damage can be done to delicate sutures, resulting in excessive bleeding and possibly an unexpected return to the operating room. Continual reorientation and vigilant observation of the patient is necessary to prevent rubbing the eyes or removing the dressing. A small amount of serosanguineous drainage can be expected. Reinforcement of the initial sterile dressing is appropriate. If the dressing becomes saturated or is removed in any way, the surgeon will need to be notified immediately to assess the operative eye and to replace the dressing.

FIG. 33-6 Patient with lead shield after surgical application of iodine plaque.
(Courtesy Wills Eye Hospital, Philadelphia, Penn.)
Observation of patients until discharge criteria have been met is more beneficial than having a standard minimum time that each patient must remain in the PACU. Post anesthesia discharge scoring systems have been developed and used in many facilities to judge a patient’s readiness for discharge. A standardized patient scoring system cannot substitute for a physical assessment by the perianesthesia nurse that accounts for the individual patient’s needs. Before discharge, all of the patient’s vital signs should be within normal limits. Pain, nausea, and vomiting should also be under control. Discharge criteria should be based on the patient’s physical assessment, the severity of underlying disease, the anesthetic and recovery course, the last dose of opioids, and the level of continued care after discharge. Discharge criteria should be developed in consultation with the anesthesia department and approved by the medical staff.14 Whenever a doubt exists regarding the patient’s condition or safety, discharge should be delayed and the surgeon notified. Patients that meet predefined discharge criteria can bypass PACU and be fast-tracked to the Phase II recovery area directly from the operating room.15
Summary
The perianesthesia nurse has a role that encompasses various modalities. Being a patient advocate, educator, and collaborative health care team member will prove invaluable. Perianesthesia nurses can participate in and use evidence-based approaches that will provide a higher level of care and an advanced knowledge base to rely upon. By optimizing and streamlining patient care, the benefits in postoperative ophthalmic outcomes will have a direct physical, psychologic, and financial effect on the patient and their families.
1. McGoldrick KE, et al. Anesthesia and the eye. Barash PG, et al. Clinical anesthesia, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2006.
2. Feldman MA, Patel A. Anesthesia for eye, ear, nose, and throat surgery. Miller RD, ed. Miller’s anesthesia, ed 7, St. Louis: Churchill Livingstone, 2009.
3. George EE, Bigatello LM. The postanesthesia care unit. Hurford WE, et al. Clinical anesthesia procedures of the Massachusetts General Hospital, ed 6, Philadelphia: Lippincott Williams & Wilkins, 2002.
4. Gomillion MC. Ambulatory surgery. Yao FF, ed. Anesthesiology: problem-oriented patient management, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2003.
5. Jiménez A, et al. Cancellations in ambulatory day surgery: ten years observational study. J Ambulatory Surgery.2006;12(3):119–123.
6. Morgan GEJr, et al. Clinical anesthesiology, ed 4. New York: McGraw-Hill; 2006.
7. Cook-Sather SD. Pediatric ophthalmologic complications. In: Atlee JL, ed. Complications in anesthesia. Philadelphia: Saunders, 1999.
8. American Academy of Ophthalmology: Policy statements color codes for topical ocular medications. available at: www.aao.org/about/policy/upload/color-codes-for-topical-ocular-medications-2010.pdf, 2010. Accessed June 23, 2011
9. Lydon A, Acquadro MA. Anesthesia for head and neck surgery. Hurford WE, et al. Clinical anesthesia procedures of the Massachusetts General Hospital, ed 6, Philadelphia: Lippincott Williams & Wilkins, 2002.
10. Hauser MW, et al. Anesthesia for pediatric ophthalmic surgery. Motoyama EK, Davis PJ. Smith’s anesthesia for infants and children, ed 7, Philadelphia: Mosby, 2006.
11. Mecca RS. Postoperative recovery. Barash PG, et al. Clinical anesthesia, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2006.
12. Pellegrini J, et al. Comparison of inhalation of isopropyl alcohol vs promethazine in the treatment of postoperative nausea and vomiting (PONV) in patients identified as at high risk for developing PONV. AANA J. 2009;77(4):293–299.
13. Morgan GEJr, et al. Clinical anesthesiology, ed 4. Philadelphia: McGraw-Hill; 2006.
14. American Society of PeriAnesthesia Nurses (ASPAN): 2010-2012 Standards of perianesthesia nursing practice. Cherry Hill, NJ: ASPAN; 2010.
15. Apfel CC. Postoperative nausea and vomiting. Miller RD, ed. Miller’s anesthesia, ed 7, Philadelphia: Churchill Livingstone, 2005.
Feldman MA, Patel A, et al. Anesthesia for eye, ear, nose, and throat surgery. Miller RD, ed. Miller’s anesthesia, ed 7, St. Louis: Churchill Livingstone, 2009.
National Institutes of Health,National Eye Institute: Eye health information. available at: www.nei.nih.gov/health/, September 23, 2011. Accessed