Chapter 1
Cardiovascular Physical Examination
1. What is the meaning of a slow rate of rise of the carotid arterial pulse?
2. What is the significance of a brisk carotid arterial upstroke?
 Simultaneous emptying of the left ventricle into a high-pressure bed (the aorta) and a lower pressure bed: The latter can be the right ventricle (in patients with ventricular septal defect [VSD]) or the left atrium (in patients with mitral regurgitation [MR]). Both will allow a rapid left ventricular emptying, which, in turn, generates a brisk arterial upstroke. The pulse pressure, however, remains normal.
Simultaneous emptying of the left ventricle into a high-pressure bed (the aorta) and a lower pressure bed: The latter can be the right ventricle (in patients with ventricular septal defect [VSD]) or the left atrium (in patients with mitral regurgitation [MR]). Both will allow a rapid left ventricular emptying, which, in turn, generates a brisk arterial upstroke. The pulse pressure, however, remains normal.
 Hypertrophic cardiomyopathy (HCM): Despite its association with left ventricular obstruction, this disease is characterized by a brisk and bifid pulse, due to the hypertrophic ventricle and its delayed obstruction.
Hypertrophic cardiomyopathy (HCM): Despite its association with left ventricular obstruction, this disease is characterized by a brisk and bifid pulse, due to the hypertrophic ventricle and its delayed obstruction.
3. In addition to aortic regurgitation, which other processes cause rapid upstroke and widened pulse pressure?
Pulsus alternans is the alternation of strong and weak arterial pulses despite regular rate and rhythm. First described by Ludwig Traube in 1872, pulsus alternans is often associated with alternation of strong and feeble heart sounds (auscultatory alternans). Both indicate severe left ventricular dysfunction (from ischemia, hypertension, or valvular cardiomyopathy), with worse ejection fraction and higher pulmonary capillary pressure. Hence, they are often associated with an S3 gallop.
6. What is the Duroziez double murmur?
7. What is the carotid shudder?
8. What is the Corrigan pulse?
9. How do you auscultate for carotid bruits?
10. What is the correlation between symptomatic carotid bruit and high-grade stenosis?
11. What is central venous pressure (CVP)?
12. Which veins should be evaluated for assessing venous pulse and CVP?
13. Can the external jugulars be used for evaluating central venous pressure?
Theoretically not, practically yes. Not because:
 While going through the various fascial planes of the neck, they often become compressed.
While going through the various fascial planes of the neck, they often become compressed.
 In patients with increased sympathetic vascular tone, they may become so constricted as to be barely visible.
In patients with increased sympathetic vascular tone, they may become so constricted as to be barely visible.
 They are farther from the right atrium and thus in a less straight line with it. Yet, both internal and external jugular veins can actually be used for estimating CVP because they yield comparable estimates.
They are farther from the right atrium and thus in a less straight line with it. Yet, both internal and external jugular veins can actually be used for estimating CVP because they yield comparable estimates.
14. What is a “cannon” A wave?
15. How do you estimate the CVP?
 By positioning the patient so that you can get a good view of the internal jugular vein and its oscillations. Although it is wise to start at 45 degrees, it doesn’t really matter which angle you will eventually use to raise the patient’s head, as long as it can adequately reveal the vein. In the absence of a visible internal jugular, the external jugular may suffice.
By positioning the patient so that you can get a good view of the internal jugular vein and its oscillations. Although it is wise to start at 45 degrees, it doesn’t really matter which angle you will eventually use to raise the patient’s head, as long as it can adequately reveal the vein. In the absence of a visible internal jugular, the external jugular may suffice.
 By identifying the highest point of jugular pulsation that is transmitted to the skin (i.e., the meniscus). This usually occurs during exhalation and coincides with the peak of A or V waves. It serves as a bedside pulsation manometer.
By identifying the highest point of jugular pulsation that is transmitted to the skin (i.e., the meniscus). This usually occurs during exhalation and coincides with the peak of A or V waves. It serves as a bedside pulsation manometer.
 By finding the sternal angle of Louis (the junction of the manubrium with the body of the sternum). This provides the standard zero for jugular venous pressure (JVP). (The standard zero for CVP is instead the center of the right atrium.)
By finding the sternal angle of Louis (the junction of the manubrium with the body of the sternum). This provides the standard zero for jugular venous pressure (JVP). (The standard zero for CVP is instead the center of the right atrium.)
 By measuring in centimeters the vertical height from the sternal angle to the top of the jugular pulsation. To do so, place two rulers at a 90-degree angle: one horizontal (and parallel to the meniscus) and the other vertical to it and touching the sternal angle (Fig. 1-1). The extrapolated height between the sternal angle and meniscus represents the JVP.
By measuring in centimeters the vertical height from the sternal angle to the top of the jugular pulsation. To do so, place two rulers at a 90-degree angle: one horizontal (and parallel to the meniscus) and the other vertical to it and touching the sternal angle (Fig. 1-1). The extrapolated height between the sternal angle and meniscus represents the JVP.
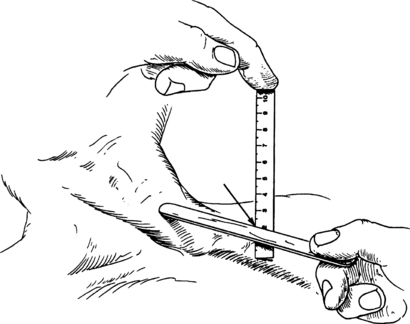
Figure 1-1 Measurement of jugular venous pressure. (From Adair OV: Cardiology secrets, ed 2, Philadelphia, 2001, Hanley & Belfus.)
 By adding 5 to convert jugular venous pressure into central venous pressure. This method relies on the fact that the zero point of the entire right-sided manometer (i.e., the point where CVP is, by convention, zero) is the center of the right atrium. This is vertically situated at 5 cm below the sternal angle, a relationship that is present in subjects of normal size and shape, regardless of their body position. Thus, using the sternal angle as the external reference point, the vertical distance (in centimeters) to the top of the column of blood in the jugular vein will provide the JVP. Adding 5 to the JVP will yield the CVP.
By adding 5 to convert jugular venous pressure into central venous pressure. This method relies on the fact that the zero point of the entire right-sided manometer (i.e., the point where CVP is, by convention, zero) is the center of the right atrium. This is vertically situated at 5 cm below the sternal angle, a relationship that is present in subjects of normal size and shape, regardless of their body position. Thus, using the sternal angle as the external reference point, the vertical distance (in centimeters) to the top of the column of blood in the jugular vein will provide the JVP. Adding 5 to the JVP will yield the CVP.
16. What is the significance of leg swelling without increased CVP?
17. What is the Kussmaul sign?
19. Which characteristics of the apical impulse should be analyzed?
 Location: Normally over the fifth left interspace midclavicular line, which usually (but not always) corresponds to the area just below the nipple. Volume loads to the left ventricle (such as aortic or mitral regurgitation) tend to displace the apical impulse downward and laterally. Conversely, pressure loads (such as aortic stenosis or hypertension) tend to displace the impulse more upward and medially—at least initially. Still, a failing and decompensated ventricle, independent of its etiology, will typically present with a downward and lateral shift in point of maximal impulse (PMI). Although not too sensitive, this finding is very specific for cardiomegaly, low ejection fraction, and high pulmonary capillary wedge pressure. Correlation of the PMI with anatomic landmarks (such as the left anterior axillary line) can be used to better characterize the displaced impulse.
Location: Normally over the fifth left interspace midclavicular line, which usually (but not always) corresponds to the area just below the nipple. Volume loads to the left ventricle (such as aortic or mitral regurgitation) tend to displace the apical impulse downward and laterally. Conversely, pressure loads (such as aortic stenosis or hypertension) tend to displace the impulse more upward and medially—at least initially. Still, a failing and decompensated ventricle, independent of its etiology, will typically present with a downward and lateral shift in point of maximal impulse (PMI). Although not too sensitive, this finding is very specific for cardiomegaly, low ejection fraction, and high pulmonary capillary wedge pressure. Correlation of the PMI with anatomic landmarks (such as the left anterior axillary line) can be used to better characterize the displaced impulse.
 Size: As measured in left lateral decubitus, the normal apical impulse is the size of a dime. Anything larger (nickel, quarter, or an old Eisenhower silver dollar) should be considered pathologic. A diameter greater than 4 cm is quite specific for cardiomegaly.
Size: As measured in left lateral decubitus, the normal apical impulse is the size of a dime. Anything larger (nickel, quarter, or an old Eisenhower silver dollar) should be considered pathologic. A diameter greater than 4 cm is quite specific for cardiomegaly.
 Duration and timing: This is probably one of the most important characteristics. A normal apical duration is brief and never passes midsystole. Thus, a sustained impulse (i.e., one that continues into S2 and beyond—often referred to as a “heave”) should be considered pathologic until proven otherwise and is usually indicative of pressure load, volume load, or cardiomyopathy.
Duration and timing: This is probably one of the most important characteristics. A normal apical duration is brief and never passes midsystole. Thus, a sustained impulse (i.e., one that continues into S2 and beyond—often referred to as a “heave”) should be considered pathologic until proven otherwise and is usually indicative of pressure load, volume load, or cardiomyopathy.
 Amplitude: This is not the length of the impulse, but its force. A hyperdynamic impulse (often referred to as a “thrust”) that is forceful enough to lift the examiner’s finger can be encountered in situations of volume overload and increased output (such as AR and VSD), but may also be felt in normal subjects with very thin chests. Similarly, a hypodynamic impulse can be due to simple obesity but also to congestive cardiomyopathy. In addition to being hypodynamic, the precordial impulse of these patients is large, somewhat sustained, and displaced downward and/or laterally.
Amplitude: This is not the length of the impulse, but its force. A hyperdynamic impulse (often referred to as a “thrust”) that is forceful enough to lift the examiner’s finger can be encountered in situations of volume overload and increased output (such as AR and VSD), but may also be felt in normal subjects with very thin chests. Similarly, a hypodynamic impulse can be due to simple obesity but also to congestive cardiomyopathy. In addition to being hypodynamic, the precordial impulse of these patients is large, somewhat sustained, and displaced downward and/or laterally.
 Contour: A normal apical impulse is single. Double or triple impulses are clearly pathologic.
Contour: A normal apical impulse is single. Double or triple impulses are clearly pathologic.
Bibliography, Suggested Readings, and Websites
1. Geisel School of Medicine at Dartmouth. On doctoring: physical examination movies. Available at http://dms.dartmouth.edu/ed_programs/course_resources/ondoctoring_yr2/. Accessed March 26, 2013
2. Basta, L.L., Bettinger, J.J. The cardiac impulse. Am Heart J. 1979;197:96–111.
3. Constant, J. Using internal jugular pulsations as a manometer for right atrial pressure measurements. Cardology. 2000;93:26–30.
4. Cook, D.J., Simel, N. Does this patient have abnormal central venous pressure? JAMA. 1996;275:630–634.
5. Davison, R., Cannon, R. Estimation of central venous pressure by examination of the jugular veins. Am Heart J. 1974;87:279–282.
6. Drazner, M.H., Rame, J.E., Stevenson, L.W., et al. Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med. 2001;345:574–581.
7. Ellen, S.D., Crawford, M.H., O’Rourke, R.A. Accuracy of precordial palpation for detecting increased left ventricular volume. Ann Intern Med. 1983;99:628–630.
8. Mangione, S. Physical diagnosis secrets, ed 2. Philadelphia: Mosby; 2008.
9. McGee, S.R. Physical examination of venous pressure: a critical review. Am Heart J. 1998;136:10–18.
10. O’Neill, T.W., Barry, M., Smith, M., et al. Diagnostic value of the apex beat. Lancet. 1989;1:410–411.
11. Sauve, J.S., Laupacis, A., Ostbye, T., et al. The rational clinical examination. Does this patient have a clinically important carotid bruit? JAMA. 1993;270:2843–2845.




