11 Cardiac Monitoring and Cardiopulmonary Resuscitation
Note 1: This book is written to cover every item listed as testable on all Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and WRE, it will simply be shown as (Code: …). If an item is only testable on the ELE, it will be shown as (ELE code: …). If an item is only testable on the WRE, it will be shown as (WRE code: …).
MODULE A
1. Manipulate electrocardiogram monitors by order or protocol (ELE code: IIA18) [Difficulty: ELE: R, Ap]
a. Get the necessary equipment for the procedure
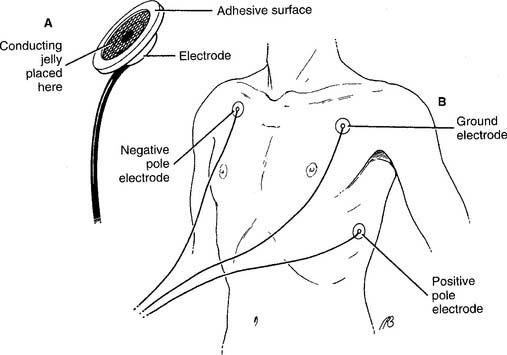
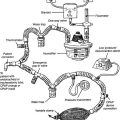
To perform electrocardiogram (ECG) monitoring, it is necessary to select the proper cardiac electrodes and the monitoring unit. Cardiac electrodes, or leads, pick up the electrical signal from a heart contraction and conduct it to the monitor. They are usually called chest leads (or chest electrodes or precordial leads) and consist of four parts: (1) a conducting wire coated with an electrically neutral plastic, (2) an adapter at one end of the wire that plugs into the electrocardiograph machine, (3) a different adapter at the opposite end of the wire that attaches to a patient electrode, and (4) the patient electrode (Figure 11-1, A). Conducting jelly is added to the surface of the electrode to reduce the skin’s resistance to the heart’s electrical signal. An adhesive ring holds the electrode tightly to the skin. The conducting wire snaps or clips onto the back of the electrode. Typically, three to five of these chest leads are used for a period of hours or days for basic rhythm monitoring or Holter monitoring. Typically, three or four chest leads are used for rhythm monitoring. Holter monitoring typically involves using five chest leads.
One of the following monitoring units must be selected, based on the patient’s situation:
1. Basic bedside rhythm monitoring
A bedside rhythm monitoring unit usually receives input from three or four chest leads (Figure 11-1, B). That collective signal is sent to an oscilloscope (video display terminal) for a real-time display of the patient’s rhythm. These ECG machines have several additional features. They continuously display the patient’s heart rate. High and low heart rate alarm settings can be set. If the high or low setting is reached, an audible and visual alarm is triggered. The patient’s heart rhythm can be recorded on ECG paper manually by pushing a record button or automatically when an alarm setting is reached. These units are often seen mounted at the patient’s bedside in the intensive care unit.
2. Cardiopulmonary resuscitation cart
Cardiopulmonary resuscitation (CPR) “crash” carts have electrocardiographs and oscilloscopes mounted on them. These are connected to the defibrillator to allow synchronous defibrillation (cardioversion) or asynchronous defibrillation. Typically, three or four chest leads are used for rhythm monitoring (Figure 11-1, B). Crash carts have other features that are similar to those seen on bedside rhythm monitoring units. Portable versions of these units are used when the patient must be transported. A portable unit operates by battery power when unplugged from the wall electrical outlet.
3. Holter monitoring
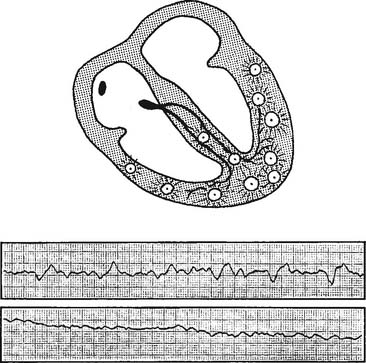
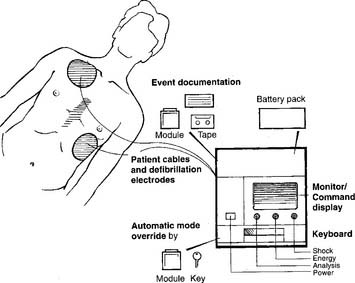
Holter monitoring involves recording a patient’s complete ECG for 1 to 3 days through the use of a portable, battery-powered monitor. In addition, the patient keeps a diary of any episodes of chest pain, dyspnea, and so forth. The whole system includes the recording device for the patient’s ECG, a set of chest leads, a carrying bag for the recording device, and a patient activity diary (Figure 11-2).
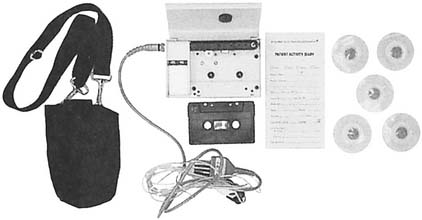
Figure 11-2 Holter monitoring system for ambulatory electrocardiography.
(From Pagana K, Pagana TJ: Mosby’s manual of diagnostic and laboratory tests, ed 3, St Louis, 2006, Mosby.)
2. Manipulate diagnostic electrocardiogram machines by order or protocol (ELE code: IIA19) [Difficulty: ELE: R, Ap]
a. Get the necessary equipment for the procedure
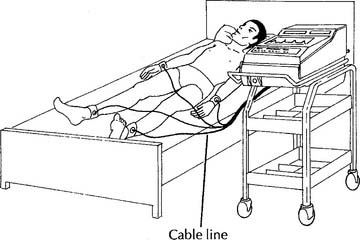
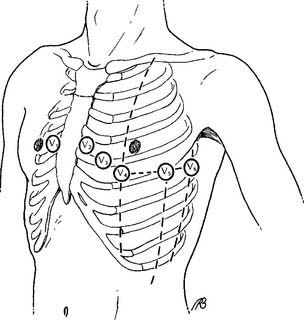
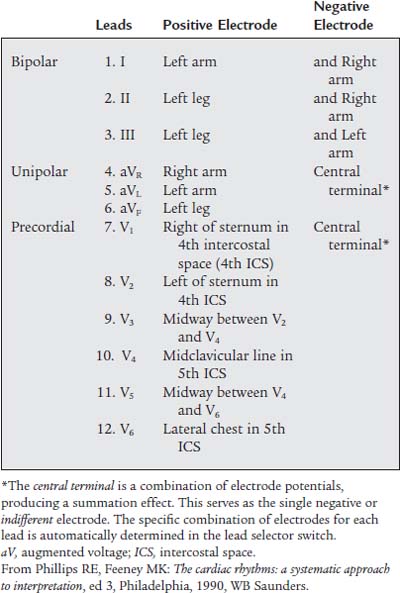
A 12-lead ECG test requires a machine capable of receiving electrical input from the four limb leads and six precordial leads (see Figures 11-3 and 11-4). The operator can manually select the lead combinations needed to get the 12 different combinations for a 12-lead ECG tracing. However, modern units do this automatically when the operator turns them on. The various ECG combinations are printed out on ECG paper. Modern units also store the patient’s information on a self-contained computer.
b. Put the equipment together and make sure that it works properly
The limb leads come as a group of four with one for each arm and leg (Figure 11-3). Precordial leads came in a group of six and are placed on the chest in the positions shown in Figure 11-4. A conducting and adhesive jelly is used to reduce the skin’s resistance and to hold the lead in place. The limb leads are longer, and they may need to be held in place by a rubber strap.
3. Cardiac monitoring
c. Monitor the cardiac rhythm to evaluate the patient’s response to respiratory care (Code: IIIE6) [Difficulty: ELE: R, Ap; WRE: An]
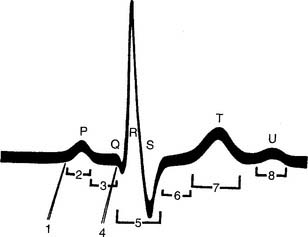
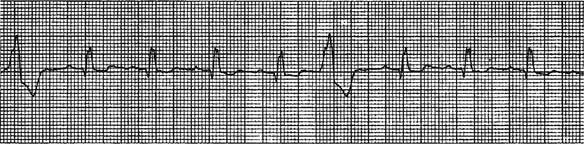
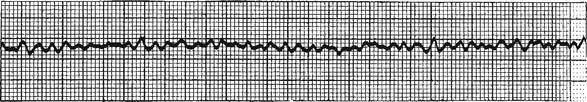
The most common chest electrode pattern used for rhythm monitoring is called lead II. The three chest electrodes are placed as shown in Figure 11-1, B. The negative (right arm, RA) electrode is on the right upper chest. The positive (left leg, LL) electrode is placed on the left lateral chest. The ground (left arm, LA) electrode is placed on the left upper chest. With this electrode configuration, known as the Einthoven triangle, the heart’s electrical signal is followed as it flows from the right atrium to the left ventricle. This results in the so-called normal ECG tracing with upright P, R, and T waves, as shown in Figures 11-5 and 11-6. Table 11-1 shows the sequential electrical events of the normal cardiac rhythm that correspond with those in Figure 11-5.
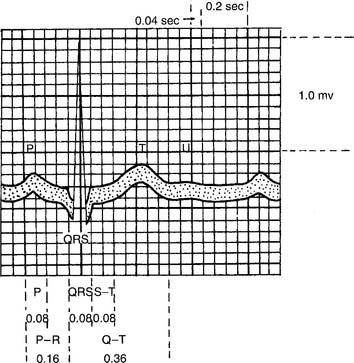
Figure 11-6 Timing of the electrical events of the cardiac cycle during normal sinus rhythm.
(From Spearman CB, Sheldon RL, Egan DF: Egan’s fundamentals of respiratory therapy, ed 4, St Louis, 1982, Mosby.)
TABLE 11-1 Electrophysiologic Events Represented by the Electrocardiogram Sequential Electrical Events Electrocardiographic of the Cardiac Cycle Representation
| 1. Impulse from the sinus node | Not visible |
| 2. Depolarization of the atria | P wave |
| 3. Depolarization of the atrio-ventricular node | Isoelectric |
| 4. Repolarization of the atria | Usually obscured by the QRS complex |
| 5. Depolarization of the ventricles | QRS complex |
| a. Intraventricular septum | a. Initial portion |
| b. Right and left ventricles | b. Central and terminal portions |
| 6. Quiescent state of the ventricles immediately after depolarization | ST segment: isoelectric |
| 7. Repolarization of the ventricles | T wave |
| 8. Afterpotentials following repolarization of the ventricles | U wave |
From Phillips RE, Feeney MK: The cardiac rhythms: systematic approach to interpretation, ed 3, Philadelphia, 1990, WB Saunders.
4. Diagnostic electrocardiogram
b. Recommend an electrocardiogram to obtain additional data (Code: IC9) [Difficulty: ELE: R, Ap; WRE: An]
A diagnostic electrocardiogram (also called a 12-lead ECG) test is indicated if the patient is suspected of having cardiac problems. Symptoms such as syncope, angina pectoris, sudden crushing chest pain, shortness of breath, or unstable heart rate and blood pressure point to a heart problem. Growing evidence indicates that men and women have different signs and symptoms during an acute myocardial infarction (AMI or MI). Men tend to have crushing central chest pain that may radiate down the left arm or the left side of the neck, diaphoresis, cold extremities, shortness of breath, and a feeling of impending doom. Women tend to experience pain in the lower back and the abdominal area. A diagnostic ECG is indicated to document the nature of the cardiac problem or rule out the heart as a source of the symptoms.
c. Perform a diagnostic electrocardiogram (Code: IB9a) [Difficulty: ELE: R, WRE: Ap, An]
The 12-lead ECG involves the use of an electrocardiograph machine with heat-sensitive ECG recording paper, four limb leads, and six precordial leads (see Figures 11-3 and 11-4). Table 11-2 describes the locations of the precordial leads and the positive and negative electrode combinations that are used to record the heart’s electrical signal through the 12 different leads. Each lead individually records the heart’s electrical activity, but it does so from a different position in relation to the heart. These 12 leads give the physician a three-dimensional impression of how the cardiac conduction system and the myocardium are functioning. Abnormal functioning can be diagnosed. Review the normal anatomy and physiology of the heart and its conduction system, if necessary.
MODULE B
1. Manipulate a manual resuscitator (bag-valve or bag-mask by order or protocol (ELE code: IIA5) [Difficulty: ELE: R, Ap, An]
a. Get the necessary equipment for the procedure
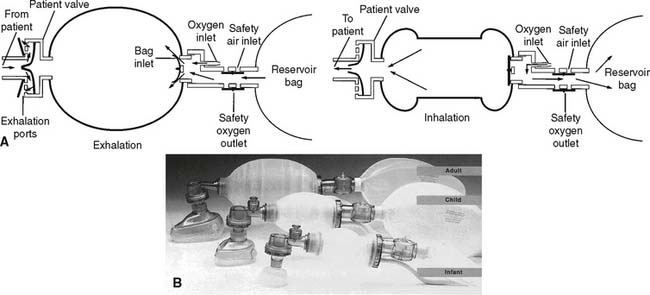
The first consideration when deciding which manual resuscitator to select is the size of the patient. Although the volume of the reservoir bag and the tidal volume expelled from it vary among the types of bags, three basic sizes are available. An infant or newborn unit typically has a reservoir bag volume of about 250 mL. A pediatric unit usually has a reservoir bag volume of about 250 to 500 mL, and an adult unit typically has a reservoir bag volume of 1500 to 2000 mL. In addition to all of these reusable units, a number of disposable units are thrown away after one patient use. They also come in comparable infant, pediatric, and adult reservoir bag volumes.
b. Put the equipment together and make sure that it works properly
Figure 11-7 shows line drawings of a complete set of Laerdal infant, pediatric, and adult manual resuscitators. The following steps should be taken when the function of a manual resuscitator is evaluated:
c. Troubleshoot any problems with the equipment
Check for a reversed or improperly seated one-way valve (spring-loaded, duckbill, or leaf type) if the gas does not enter or exit the unit as it should. In clinical use, mucus, vomitus, and blood can foul the expiratory one-way valve system. By regulation, the valve must be clearable within 20 seconds. Do this by disconnecting the unit from the patient, aiming the adapter into a neutral area, and squeezing the bag to blow out the obstruction. Replace a unit that cannot be promptly cleared of any debris.
2. Manipulate a mouth-to-valve mask resuscitator (ELE code: IIA5) [Difficulty: ELE: R, Ap, An]
a. Get the necessary equipment for the procedure
b. Put the equipment together and make sure that it works properly
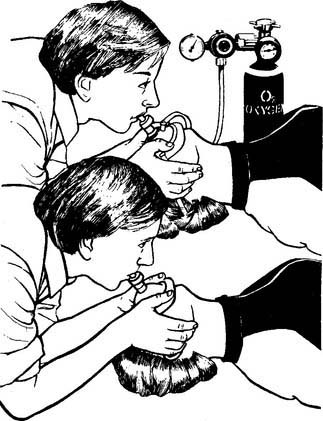
Mouth-to-valve resuscitators are relatively simple devices. Most have only two or three pieces: a face mask, a mouthpiece with a one-way valve, and possibly an oxygen T-piece (Figure 11-8). The “male” and “female” connections are designed to fit together in only one way. When they are properly assembled, no air should leak out when the breath is delivered to the victim.
MODULE C
1. Basic cardiac life support (ELE code: III I1a) [Difficulty: ELE: R, Ap, An]
The key steps of basic cardiac life support (BCLS) include the following:
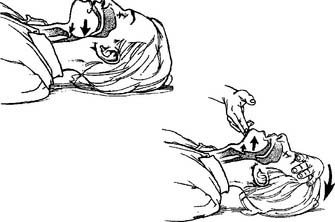
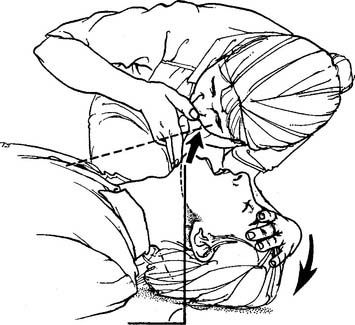
c. Open the airway
The head-tilt/chin-lift maneuver is the procedure of choice for opening the airways of all victims except those with a known or suspected cervical (neck) spine injury. The victim is gently positioned on his or her back. In an adult, the head is firmly pushed back with one hand, and the jaw is pulled upward with the fingers of the other hand (Figure 11-9). In an infant, it is not necessary to tilt the head back beyond a neutral position. Children may need to have the head pushed back slightly beyond neutral.
The jaw-thrust maneuver is the procedure of choice for opening the airway of all victims with a known or suspected cervical spine injury. The rescuer’s elbows are rested on the ground, and the hands are placed on either side of the victim’s jaw. Lifting of the jaw usually opens the airway and eliminates the need to tilt the head back. See Figure 11-10 for the adult maneuver.

Figure 11-10 Opening the adult’s airway by the jaw-thrust method.
(From Watson MA: Cardiopulmonary resuscitation. In: Barnes TA, editor: Respiratory care practice, St Louis, 1988, Mosby.)
Any obstruction that can be seen in the mouth or throat should be removed. The cross-finger technique can be used to open the mouth wide enough so that a finger or suction device can be inserted to remove a blockage (Figure 11-11). An oral airway should be used only in an unconscious patient to keep the tongue from falling back and blocking the airway.
d. Determine that the patient is not breathing
The rescuer places his or her face close to the victim’s face to look for rising and falling of the chest, listen for victim’s air movement, and feel any air movement from the victim’s breathing (Figure 11-12). The entire procedure should not take longer than 10 seconds.
e. Ventilate the patient
1. Mouth-to-mouth breathing
The first rescuer should begin mouth-to-mouth breathing as soon as possible if no spontaneous breathing by the victim occurs once the airway is opened. No matter the age of the victim, an effective seal must be present between the rescuer and the victim. The adult victim’s nose must be pinched closed; often the rescuer’s cheek can block the infant’s nose. The rescuer’s mouth can cover both the nose and mouth of an infant. Alternative methods include mouth-to-nose and mouth-to-stoma ventilation (Figure 11-13).

Figure 11-13 A, Adult mouth-to-mouth, mouth-to-nose (B), and mouth-to-stoma (C) ventilation.
(From Standards and guidelines for cardiopulmonary resuscitation [CPR] and emergency cardiac care [ECC], JAMA 268:2188, 1992.) Copyright © 1992, American Medical Association. All rights reserved.
A child should be given two breaths large enough to raise the victim’s chest. A child obviously needs less volume than an adult. All of the same considerations apply as for the adult. Rescue breathing should be performed at a rate of 12 to 20 per minute (every 3 to 5 seconds) in an infant and a child. A newly born infant should be ventilated at a rate of 40 to 60 per minute.

Figure 11-14 Administering the Heimlich maneuver to an unconscious adult victim of an airway obstruction.
(From Standards and guidelines for cardiopulmonary resuscitation [CPR] and emergency cardiac care [ECC], JAMA 268:2193, 1992.) Copyright © 1992, American Medical Association. All rights reserved.
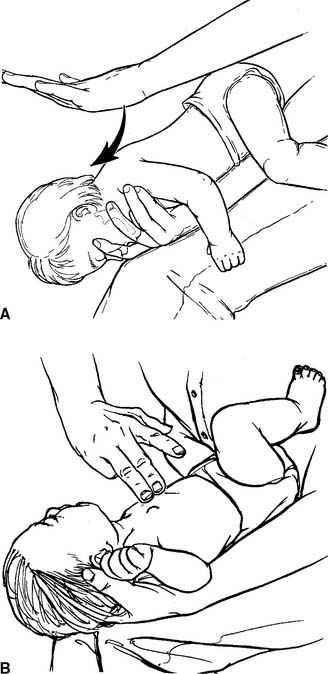
Figure 11-15 Administering (A) back blows and (B) chest thrusts to an infant victim of an obstructed airway.
(From Standards and guidelines for cardiopulmonary resuscitation [CPR] and emergency cardiac care [ECC], JAMA 268:2258, 1992.) Copyright © 1992, American Medical Association. All rights reserved.
2. Manual resuscitator (bag-valve)
A manual resuscitator should be used during hospital-based CPR as soon as one is available. The resuscitation mask must be held to the victim’s face so that no air leak occurs during the forced inspiration (Figure 11-16). An assistant can hold the mask tightly to the face so that the rescuer who is pumping the resuscitation bag can use both hands. This has been shown to produce a larger tidal volume. If the victim’s airway contains an endotracheal tube or tracheostomy tube, the expiratory valve adapter fits directly over the tube adapter. Rescue breathing continues with the previously mentioned considerations for volume and rate. After an adult victim has had an endotracheal tube placed, the tidal volume goal is 500 to 600 mL over a 1-second period to produce a visible chest rise.
3. Mouth-to-valve mask ventilation
A mouth-to-valve mask device (or pocket mask) combines a resuscitation mask with a one-way valve mouthpiece. It is used to ventilate an apneic patient rather than perform mouth-to-mouth breathing. Concerns about protecting the rescuer from patient infections such as acquired immunodeficiency syndrome (AIDS) and hepatitis have led to their widespread acceptance. As shown in Figure 11-8, the patient’s neck is hyperextended, the mask is applied over the mouth and nose to get an airtight seal, and the rescuer breathes into the mouthpiece. It is best if the rescuer is positioned at the victim’s head so that the chest can be seen to rise with each delivered breath. The one-way valve is designed so that the victim’s exhaled gas is vented out to the room air. Some units have a nipple adapter so that supplemental oxygen can be added to the delivered breath. Simply attach oxygen tubing between the nipple and oxygen flowmeter, and turn the flowmeter on to the manufacturer’s recommended flow. When this type of device is used with an adult victim, the tidal volume goal is 500 to 600 mL over a 1-second period to produce a visible chest rise. These devices should be replaced by a manual resuscitator as soon as possible.
g. Determine pulselessness
The carotid pulse is felt for in all victims except children younger than 1 year. The carotid pulse is found by gently feeling with two or three fingers in the groove between the larynx and the sternocleidomastoid muscle on either side of the neck (Figure 11-17). Check for 5 to 10 seconds to be sure that the victim is pulseless and not just bradycardic. In addition, check for other signs of circulation such as spontaneous breathing, coughing, and movement. An infant younger than 1 year should have the pulse felt in the brachial artery; the carotid artery is difficult to find in such young children because they have short, chubby necks.
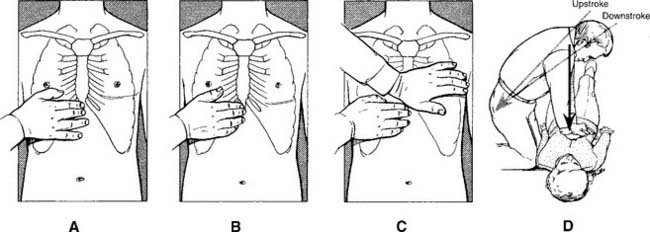
h. Perform external chest compressions
In adults and large children or those older than 8 years, the heel of the rescuer’s hand is placed over the lower half of the sternum. This is found by placing the middle finger of one hand in the notch where the ribs meet the sternum, placing the index finger next to it, and placing the other hand next to the finger. The first hand is placed over it, the elbows are locked, and the shoulders are directly over the hands. This creates the most efficient pumping action (Figure 11-18). The rescuer pivots from the hips, with half of the time spent pumping down and half of the time releasing pressure. The hands should always touch the victim’s chest. The sternum must be compressed 4 to 5 cm (1.5 to 2.0 inches) in an adult at a rate of 100 compressions per minute for an actual rate of more than 80 per minute.
In newly born infants and older infants, the preferred method of chest compressions is called the two thumbs–encircling hands technique (Figure 11-19). This method works best when a second rescuer can ventilate the infant. It also is acceptable to compress with two or three fingers placed over the middle of the sternum one finger’s width below an imaginary line drawn between the nipples (Figure 11-20). This method is easier when one rescuer must provide ventilations and compressions. In either case, the child’s sternum must be compressed to a depth of 1.3 to 2.5 cm (0.5 to 1 in.). Half the time should be spent on compression and half the time on relaxation. A newly born infant should have a rate of at least 120 compressions per minute to achieve an actual rate of 90 per minute.
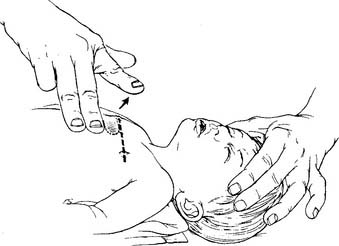
Figure 11-20 Locating the proper finger position for chest compressions on an infant.
(From Standards and guidelines for cardiopulmonary resuscitation [CPR] and emergency cardiac care [ECC], JAMA 268:2256, 1992.) Copyright © 1992, American Medical Association. All rights reserved.)
The steps for one- and two-person hospital-based CPR follow.
1. Adult one-rescuer CPR
2. Adult two-rescuer CPR
3. Infant and child one- and two-rescuer CPR
4. Neonatal one and two-rescuer CPR
2. Advanced cardiac life support (Code: III I1b) [Difficulty: ELE: R, Ap; WRE: An]
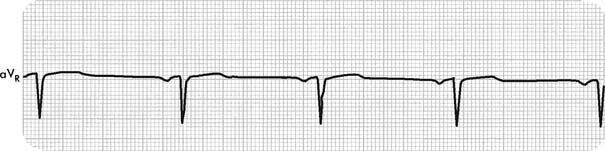
a. Interpret the results of a diagnostic electrocardiogram (Code: IB10a) [Difficulty: ELE: R, Ap; WRE: An]
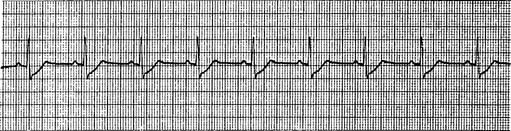
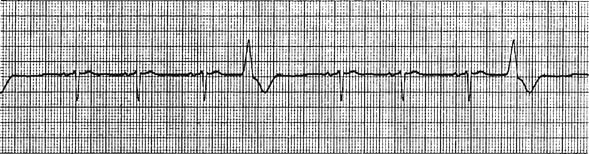
1. ECG paper
Before discussing 12-lead ECG interpretation, it is important to understand how ECG paper is designed so that the heart’s electrical signal traced on it can be understood. This special paper is heat sensitive and, after exiting the ECG machine, shows a black line from the heated stylus. Figure 11-21 shows the grid markings on the paper and how to interpret the ECG tracing for voltage and time. Each large square box is 5 mm in height and represents 0.5 millivolts (mV) of the heart’s electrical force. The large square box is divided into five smaller boxes that are 1 mm in height and represent 0.1 mV. Timing of the ECG tracing is determined by the speed with which the paper passes under the heated stylus. Normally, this is 25 mm/sec. At this speed, each large square box is 20 seconds, and each of the five small boxes is 0.04 seconds; 300 large boxes compose 1 minute’s time (0.20 seconds ¥ 300 = 60 seconds).
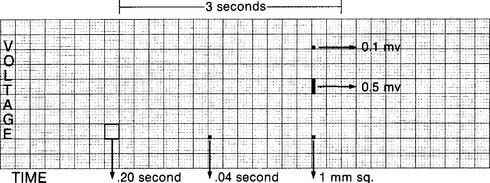
Figure 11-21 ECG paper with added details on how to interpret time and voltage.
(From Patel JM, McGowan SG, Moody LA: Arrhythmias: detection, treatment, and cardiac drugs, Philadelphia, 1989, Saunders.)
The following 10 features should be examined and time interval measured in every ECG:
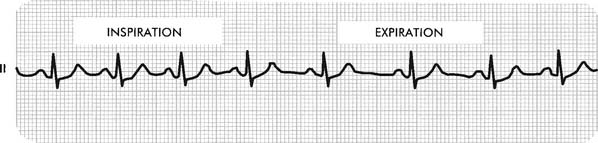
3. Heart rate
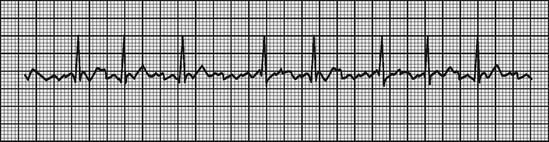
For example, in Figure 11-22, during inspiration there are three large boxes between R waves for a heart rate of about 100/minute. During exhalation there are four large boxes between R waves for a heart rate of about 75/minute.
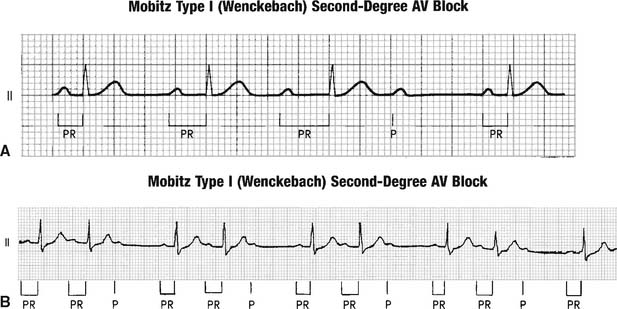
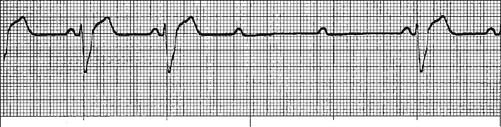
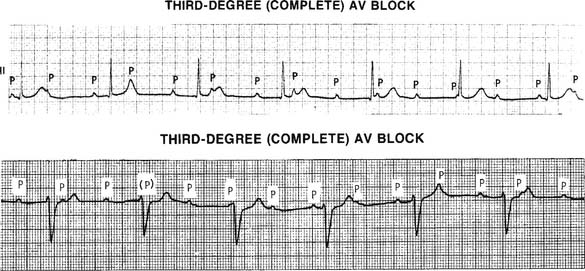
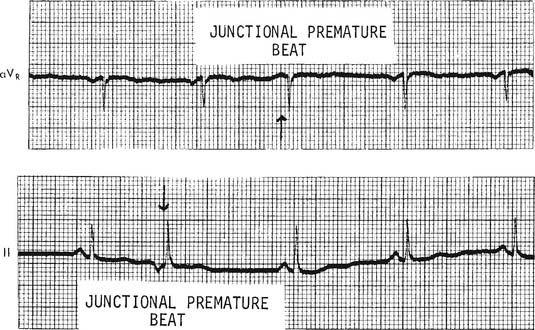
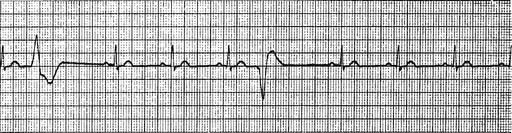
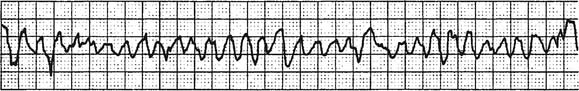
b. Abnormal cardiac rhythms.
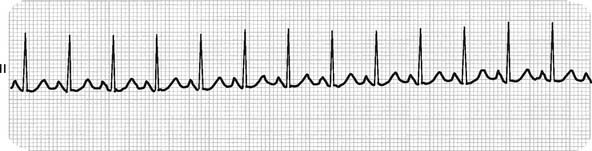
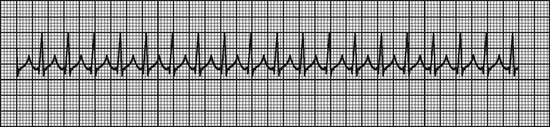
Figure 11-23 Sinus tachycardia.
(From Goldberger AL: Clinical electrocardiography: a simplified approach, ed 7, St Louis, 2006, Mosby.)
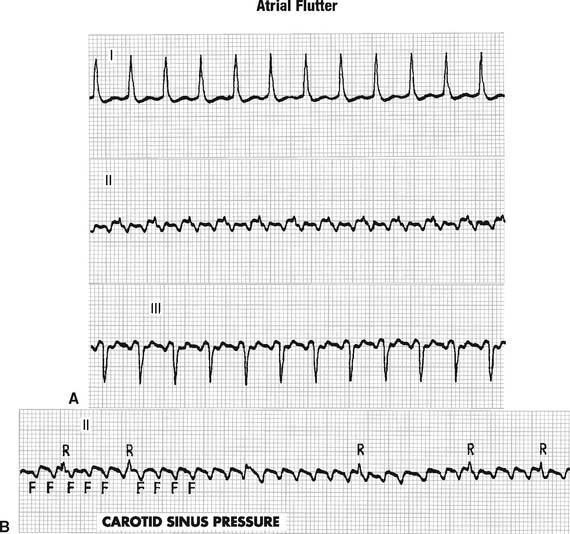
Patients with long runs of PAT usually complain of a sudden onset of pounding or fluttering in the chest. This is often associated with breathlessness, weakness, and angina pectoris in patients with coronary artery disease. Because of these problems, long runs of PAT must be treated. Treatment usually progresses in the following sequence: (1) give a sedative, (2) stimulate the vagus nerve by rubbing the carotid sinus (Figure 11-26), (3) give propranolol (Inderal) or a similar medication, and (4) perform synchronized cardioversion. (This last procedure is described in Chapter 18.) Obviously, if the patient responds to one treatment method, no need exists to go on to the next.
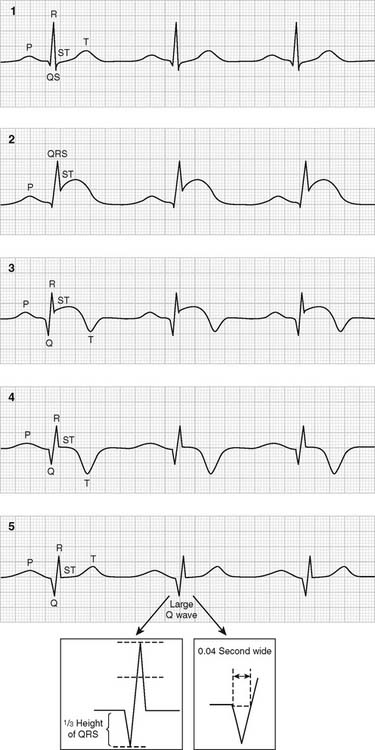
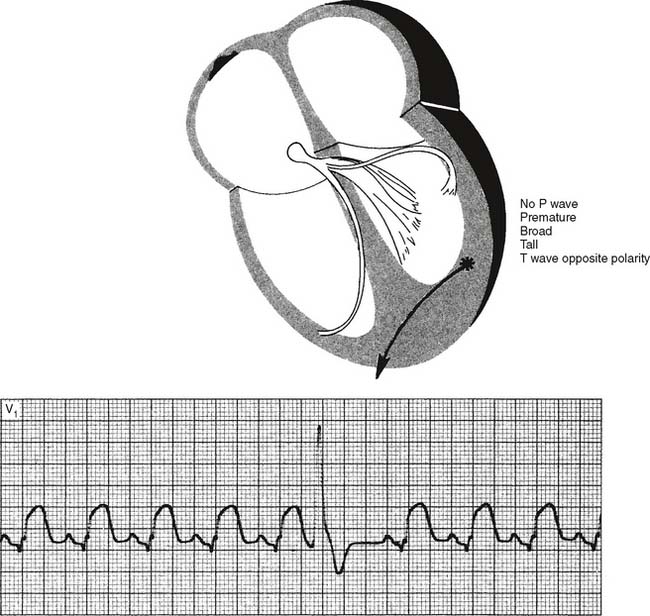
Often, however, the patient comes to the hospital too late, and an MI with heart damage is present. If the damaged area is large enough, the heart fails to pump adequately, and the patient dies. A smaller infarct weakens the heart. In addition, the damaged or dying tissue acts as an abnormal focus for the arrhythmias discussed next. The ECG changes that occur during the acute stage of an MI and as the heart heals are shown in Figure 11-34 and are listed here:
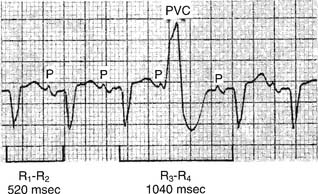
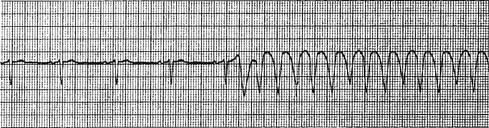
A single PVC is not dangerous unless it originates during the T wave, when the heart is especially vulnerable to electrical stimulation (Figure 11-37). Then, it can cause ventricular fibrillation.
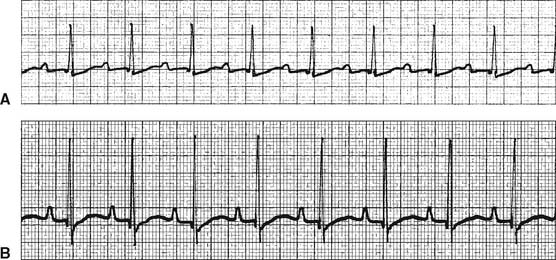
If all PVCs look the same, they originate from the same area (focus) and are called unifocal. All patients with PVCs should be watched more closely and probably treated when their PVCs are seen more frequently than 1 in 10 beats, seen in groups of two or three, or seen in multiple configurations. For example, two different-looking PVCs mean that two different ventricular foci are firing prematurely (Figure 11-38). These different looking PVCs would be called multifocal. Bigeminy occurs when every second beat is a PVC; trigeminy is when every third beat is a PVC. These dangerous situations must be rapidly treated. Lidocaine (Xylocaine) is given intravenously if the heart rate is more than 60 beats/min. If that does not work, procainamide hydrochloride (Pronestyl) is added. Additionally, the patient is given supplemental oxygen to improve oxygenation to the irritable heart.
b. Draw an arterial blood gas sample (Code: IB9f, IIIE2a) [Difficulty: ELE: R, Ap; WRE: An]
Blood for arterial blood gas (ABG) determination is usually drawn in any hospital-based CPR effort. It should not be done at the expense of time that should be spent starting effective ventilations and chest compressions or defibrillating the heart. The blood gas values give important information on the patient’s oxygenation and helps to determine whether the patient is acidotic. Changes in the ventilation efforts and medications such as bicarbonate are based on information from the ABGs. See Chapter 3 for the discussion on arterial blood sampling.
The femoral site is usually the best to draw from in a CPR situation because it is the largest artery and the easiest to hit. It is far enough from the chest that blood can be drawn without interfering in the chest compression efforts.
c. Interpret the results of arterial blood gas analysis (ELE code: IIIE4a) [Difficulty: ELE: R, Ap, An]
The full discussion of ABG interpretation is presented in Chapter 3. During a CPR attempt, the key things to look for are the patient’s Pao2 and PaCO2, because they relate to the adequacy of ventilations and chest compressions. If the patient has an acidotic pH and a normal or low PaCO2, the patient has an uncorrected metabolic acidosis. Intravenous (IV) sodium bicarbonate is indicated.
d. Perform endotracheal intubation (Code: IIIB3) [Difficulty: ELE: R, Ap; WRE: An]
Oral endotracheal intubation is usually performed during a CPR attempt. See Chapter 12 for a complete discussion of endotracheal tubes, intubation equipment, and the process of performing intubation. Current CPR guidelines indicate that if an endotracheal tube cannot be placed into a patient, a laryngeal mask airway (LMA) or Combitube may be inserted to provide a secure airway.
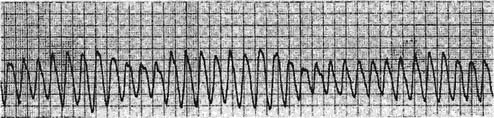
e. Make the recommendation to defibrillate the patient
Defibrillation sends a specific amount of direct electrical current (DC) through the patient’s chest wall and heart. Its purpose is to stimulate the entire cardiac muscle and electrical system so that the source of an abnormal signal will be suppressed. The SA node usually then takes over as the normal pacemaker. Chapter 18 includes a table listing the stepped progression of power used in defibrillation.
Synchronized defibrillation (cardioversion) (see Chapter 18) should be performed under the following circumstances: atrial flutter, PAT, atrial fibrillation, and ventricular tachycardia unless the patient is pulseless, unresponsive, hypotensive, or in pulmonary edema.
f. Recommend ACLS protocol agents (Code: IIIG4d) [Difficulty: ELE: R, Ap; WRE: An]
2. Antiarrhythmic drugs
Tachycardia (a resting adult heart rate of greater than 100 beats/min) and abnormal, fast heartbeats originating from the atria or ventricles are potentially very dangerous. Fast tachycardia and dangerous arrhythmias must be controlled with medications that slow the heart’s conduction system or suppress the generation of abnormal electrical signals. Common medications that do this include propranolol (Inderal), lidocaine (Xylocaine), and procainamide (Pronestyl).
g. Administer ACLS protocol medications by endotracheal installation (Code: IIID5c) [Difficulty: ELE: R, Ap; WRE: An]
Cardiac medications may be instilled down the endotracheal tube when a resuscitation attempt is under way and the patient does not have a functional central or peripheral IV line. The following medications may be instilled into adult patients: naloxone (Narcan), atropine, vasopressin (Arginine), epinephrine, and lidocaine (Xylocaine). (Hint: Use “NAVEL,” from the first letters of the generic name of these medications, to help remember them.) Naloxone should only be given intravenously to a newborn infant. The dose of any medication is based on the patient’s size and may be larger than that given intravenously. This is because the medication is diluted through the airways and must be absorbed through the mucous membrane. Previous adult guidelines indicated that the endotracheal dose should be 2 to 2.5 times greater than the normal IV amount. The medication should be diluted by adding 10 mL of normal saline or distilled water. ‘
The following steps for instillation are recommended:
i. Recommend (Code: IC10) [Difficulty: ELE: R, Ap; WRE: An] and perform capnography or exhaled carbon dioxide measurement (Code: IB9c) [Difficulty: ELE: R; WRE: Ap, An] to evaluate the adequacy of resuscitation
The general discussion of capnography was presented in Chapter 5, and exhaled carbon dioxide monitoring was presented in Chapter 12. Either can be used to help confirm that the endotracheal tube is properly located within the trachea and the patient is exhaling carbon dioxide. It also is helpful if the patient is being transported or the endotracheal tube is being repositioned. In addition, clinical evidence suggests that monitoring the exhaled carbon dioxide level during a CPR attempt is helpful in evaluating the patient’s metabolic response. In general, if chest compressions and assisted ventilation are effective, carbon dioxide will be removed from the tissues and circulated to the lungs for exhalation. If the CPR efforts are ineffective, little exhaled carbon dioxide is measured. The absence of exhaled carbon dioxide, despite a proper CPR effort, is a grave sign.
3. Pediatric advanced life support (Code: III I1c) [Difficulty: ELE: R, Ap; WRE: An]
The general steps and procedures related to pediatric advanced life support (PALS) are covered in this chapter and Chapter 12.
4. Neonatal resuscitation program (Code: III I1d) [Difficulty: ELE: R, Ap; WRE: An]
A neonatal resuscitation program (NRP) provides training in resuscitating a newborn at birth in the delivery room. In addition to the basic and advanced CPR steps discussed in this chapter and Chapter 12, the person trained in NRP is prepared to perform the following:
MODULE D
1. Analyze available information to determine the patient’s pathophysiologic state (Code code: IIIH1) [Difficulty: ELE: R, Ap; WRE: An]
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care: Part 4: Adult basic life support. Circulation 2005. Nov. 28, 2005;112:IV-19-IV-34.
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care: Part 7.1: Adjuncts for airway control and ventilation. Circulation 2005. Nov. 28, 2005;112:IV-51-IV-75.
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care: Part 11: Pediatric basis life support. Circulation 2005. Nov. 28, 2005;112:IV-156-IV-166.
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care: Part 12: Pediatric advanced life support. Circulation 2005. Nov. 28, 2005;112:IV-167-IV-187.
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care: Part 13: Neonatal resuscitation guideline. Circulation 2005. Nov. 28, 2005;112:IV-188-IV-195.
Abedin Z, Conner RP. 12-Lead ECG interpretation: the self-assessment approach. Philadelphia: WB Saunders, 1989.
Aloan CA, Hill TV, editors. Respiratory care of the newborn and child, ed 2, Philadelphia: Lippincott-Raven, 1997.
American Association for Respiratory Care. Clinical practice guideline: capnography/capnometry during mechanical ventilation—2-3 revision & update. Respir Care. 2003;48(5):534.
American Association for Respiratory Care. Clinical practice guideline: defibrillation during resuscitation. Respir Care. 1995;40(7):744.
American Association for Respiratory Care. Clinical practice guideline: resuscitation and defibrillation in the health care setting: 2004 revision and update. Respir Care. 2004;49(9):1085.
American Association for Respiratory Care. Clinical practice guideline: management of airway emergencies. Respir Care. 1995;40(7):749.
American Association for Respiratory Care. Clinical practice guideline: resuscitation in acute care hospitals. Respir Care. 1993;38(11):1179.
American Heart Association. ACLS provider manual. Dallas, Tex: American Heart Association, 2001.
American Heart Association. PALS provider manual. Dallas, Tex: American Heart Association, 2002.
American Heart Association. Part 4: Adult basic life support. Circulation. 2004;112:IV18-IV34.
American Heart Association. Part 11: Pediatric basic life support. Circulation. 2005;112:IV156-IV166.
American Heart Association. Part 13: Neonatal resuscitation guidelines. Circulation. 2005;112:IV188-IV195.
Barnes TA. Emergency cardiovascular life support. In Wilkins RL, Stoller JK, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Barnes TA, editor. Core textbook of respiratory care practice, ed 2, St Louis: Mosby, 1994.
Barnes TA, Boudin KM. Cardiopulmonary resuscitation. In Burton GG, Hodgkin JE, Ward JJ, editors: Respiratory care: a guide to clinical practice, ed 4, Philadelphia: Lippincott-Raven, 1997.
Barnes TA, Hess DR. Cardiopulmonary resuscitation. In: Hess DR, MacIntyre NR, Mishoe SC, editors. Respiratory care principles and practice. Philadelphia: WB Saunders, 2002.
Barnhart SL, Czervinske MP. Perinatal and pediatric respiratory care. Philadelphia: WB Saunders, 1995.
Branson RD, Hess DR, Chatburn RL, editors. Respiratory care equipment, ed 2, Philadelphia: Lippincott Williams & Wilkins, 1999.
Burton GC, Hodgkin JE, Ward JJ, editors. Respiratory care: a guide to clinical practice, ed 4, Philadelphia: LippincottRaven, 1997.
Butler HH. How to read an ECG. RN. 1973;36(1):35.
Butler HH. How to read an ECG. RN. 1973;36(2):49.
Butler HH. How to read an ECG. RN. 1973;36(3):50.
Cairo JM. Assessment of cardiovascular function. In Cairo JM, Pilbeam SP, editors: Mosby’s respiratory care equipment, ed 8, St Louis: Mosby, 2010.
Davis D. Differential diagnosis of arrhythmias. Philadelphia: WB Saunders, 1991.
Durbin CG. Airway management. In Cairo JM, Pilbeam SP, editors: Mosby’s respiratory care equipment, ed 7, St Louis: Mosby, 2004.
Eubanks DH, Bone RC. Comprehensive respiratory care, ed 2. St Louis: Mosby, 1990.
Fink JB, Hunt GE, editors. Clinical practice in respiratory care. Philadelphia: Lippincott-Raven, 1999.
Fluck RR. Emergency medicine. In: Wyka KA, Mathews PJ, Clark WF, editors. Foundations of respiratory care. Albany, NY: Delmar, 2002.
Goldberger AL, Goldberger E. Clinical electrocardiography. St Louis: Mosby, 1981.
Harwood R. Exam review and study guide for perinatal/pediatric respiratory care. Philadelphia: FA Davis, 1999.
Hess D, Goff G, Johnson K. The effect of hand size, resuscitator brand, and use of two hands on volumes delivered during adult bag-valve ventilation. Respir Care. 1989;34:805.
Kacmarek RM, Mack CW, Dimas S. The essentials of respiratory care, ed 3. St Louis: Mosby, 1990.
Madama VC. Safe mouth-to-mouth resuscitation requires adjunct equipment, caution, Occup. Health Saf. 1991;60(1):56.
Marriott HJL. Practical electrocardiography, ed 7. Baltimore: Williams & Wilkins, 1983.
Marshak AB. Emergency life support. In Wilkins RL, Stoller JK, Scanlan CL, editors: Egan’s fundamentals of respiratory therapy, ed 8, St Louis: Mosby, 2003.
Pagana K, Pagana TJ. Mosby’s diagnostic and laboratory test reference, ed 9. St Louis: Mosby, 2009.
Patel JM, McGowan SG, Moody LA. Arrhythmias: detection, treatment, and cardiac drugs. Philadelphia: WB Saunders, 1989.
Phillips RE, Feeney MK. The cardiac rhythms: a systematic approach to interpretation, ed 3. Philadelphia: WB Saunders, 1990.
Physicians’ desk reference. ed 60, 2006; Thomson PDR: Montvale, NJ.
Shapiro BA, Kacmarek RM, Cane RD, et al, editors. Clinical application of respiratory care, ed 4, St Louis: Mosby, 1991.
Simmons KF, Scanlan CL. Airway management. In Wilkins RL, Stoller JK, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Sorensen KA, Wilkins RL. Interpretation of the electrocardiogram. In Wilkins RL, Stoller JK, Kacmarek RM, editors: Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
Stein E. Clinical electrocardiography: a self-study course. Philadelphia: Lea & Febiger, 1987.
Sweetwood HM. Clinical electrocardiography for nurses. Rockville, Md: Aspen Systems, 1983.
Whitaker K. Comprehensive perinatal and pediatric respiratory care, ed 2. Albany, NY: Delmar, 1997.
White GC. Equipment theory for respiratory care, ed 4. Albany, NY: Delmar, 2005.
Wilkins RL, Heuer AJ. Interpretation of electrocardiogram tracings. In Wilkins RL, Dexter JR, Heuer AJ, editors: Clinical assessment in respiratory care, ed 6, St Louis: Mosby, 2010.
Wilkins RL, Stoller JK, Kacmarek RM, editors. Egan’s fundamentals of respiratory care, ed 9, St Louis: Mosby, 2009.
SELF-STUDY QUESTIONS FOR THE ENTRY LEVEL EXAM See page 593 for answers
SELF-STUDY QUESTIONS FOR THE WRITTEN REGISTRY EXAM See page 618 for answers