Cardiac and Pericardial Tumors
Primary cardiac tumors are rare in infants and children, with a reported prevalence of up to 0.32%.1 Use of echocardiography has resulted in more frequent detection of cardiac tumors in the fetus and neonate.2 More than 90% of cardiac tumors in infants and children are benign.1 Symptoms are variable and usually depend on tumor location and size. Intracavitary cardiac tumors can cause cardiac valve obstruction or result in spread of tumor emboli into either the pulmonary or systemic vascular beds. Children with intracavitary cardiac tumors present with heart failure, dyspnea, or neurologic symptoms. Myocardial tumors compress the cardiac lumen, leading to obstruction or heart failure, and can be associated with arrhythmias. Pericardial tumors are associated with pericardial effusions. Conventional radiographs may show cardiomegaly, an abnormal cardiac shape, or pulmonary edema from congestive heart failure (e-Fig. 81-1). Cardiac tumors in children can be associated with several syndromes, as shown in Table 81-1. Computed tomography (CT) and magnetic resonance imaging (MRI) findings can help differentiate tumor types (Table 81-2).
Table 81-1
Cardiac Tumors Associated with Syndromes
| Tumor | Association |
| Rhabdomyoma | Tuberous sclerosis |
| Fibroma | Gorlin (basal cell nevus) syndrome |
| Myxoma | Carney syndrome |
Table 81-2
Cardiac Tumors: Computed Tomographic and Magnetic Resonance Imaging Findings
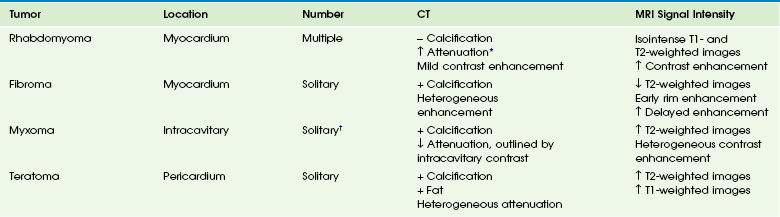
CT, computed tomography; MRI, magnetic resonance imaging.
†Multiple and recurrent tumors associated with familial forms.

e-Figure 81-1 Cardiomegaly in a child with a cardiac fibroma.
Rhabdomyoma
Pathophysiology and Clinical Presentation: Rhabdomyoma is the most common primary cardiac tumor of childhood and accounts for 60% to 79% of all cardiac tumors during the first year of life.1,3 Rhabdomyomas are hamartomas that regress and have no potential for malignancy. More than half of fetuses with rhabdomyomas are asymptomatic. Patients with rhabdomyomas can present with nonimmune fetal hydrops, outflow tract obstruction, or arrhythmia. At least 50% of patients with rhabdomyomas have tuberous sclerosis, and rhabdomyomas can be the first detectable manifestation of tuberous sclerosis.3
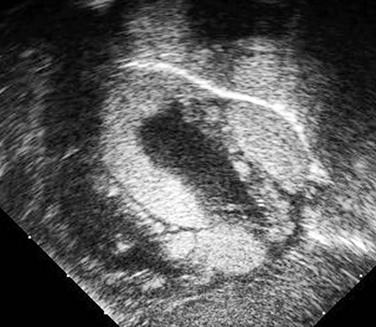
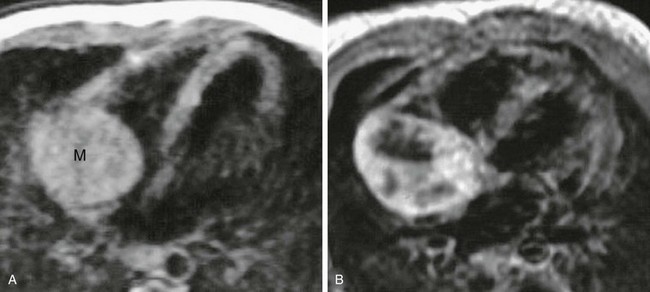
Imaging: Rhabdomyomas are round, hyperechoic, solid masses on echocardiography (e-Fig. 81-2). They usually are multiple and occur most commonly in the ventricular tissue but also can arise from atrial walls.4,5 The rhabdomyoma signal characteristics on T1- and T2-weighted MRI are similar to those of myocardium, making MRI less sensitive than echocardiography.6 Signal is increased on contrast-enhanced T1-weighted and proton-weighted imaging.7 Rhabdomyomas are easier to detect when they extend into the cardiac lumen (Fig. 81-3). They have increased attenuation compared with myocardium on noncontrast-enhanced CT scans, and they have mild delayed enhancement with contrast (e-Fig. 81-4).8 Small fat globules may be detected in rhabdomyomas.
Fibroma
Pathophysiology and Clinical Presentation: Cardiac fibroma is the second most common and the most commonly resected primary cardiac tumor of childhood.9,10 The tumors frequently are detected in the first year of life but can present throughout childhood. Fibromas are solitary tumors located in the myocardium. They are composed of fibroblasts and collagen. Calcifications are frequent and a differentiating finding compared with rhabdomyomas.1,10 The tumor can be associated with Gorlin (basal cell nevus) syndrome.7,9,10 Children can present with heart failure and arrhythmia.
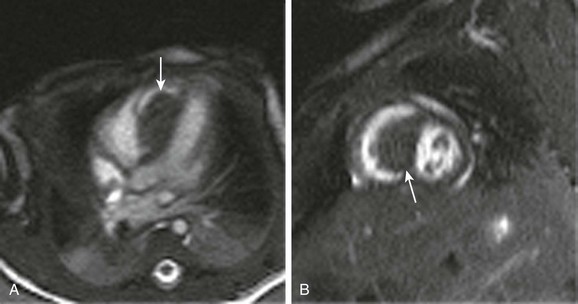
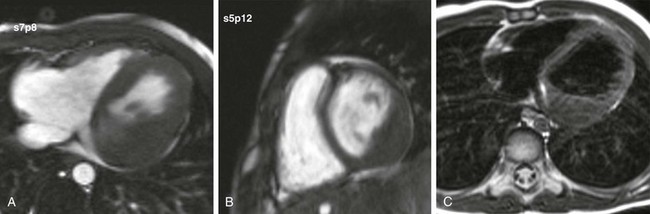
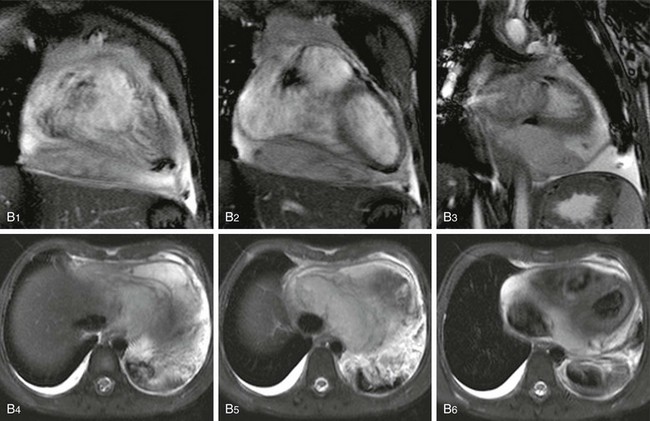
Imaging: Echocardiography reveals a heterogeneous, echogenic, solitary mass.10 Cardiac fibroma signal intensity is isointense to slightly hypointense on T1-weighted imaging and low on T2-weighted imaging.9,11 Classically, contrast-enhanced MRI of fibromas initially shows rim enhancement but decreased central enhancement compared with myocardium.12 Enhancement on delayed imaging is characteristic (Video 81-1 and Fig. 81-5 and e-Figs. 81-6 and 81-7).7,13 Calcifications may be detected by CT (e-Fig. 81-8).14
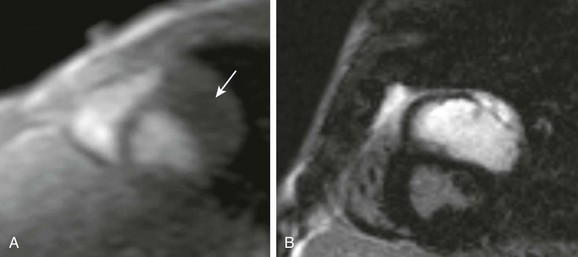
e-Figure 81-6 A solitary left ventricular mass on steady-state free-precession short-axis cine imaging.
No left ventricular contraction occurs in the region of the fibroma. A, Short-axis first-pass gadolinium perfusion shows no enhancement of the mass (arrow). B, Intense delayed enhancement in the mas is extensive and homogeneous.
Myxoma
Pathophysiology and Clinical Presentation: Myxomas are the most common cardiac tumor in adults, but they are rare in children.1,3,9,10 A myxoma is an exophytic mass extending into a cardiac chamber. Most myxomas are pedunculated, irregular masses attached to the atrial septum, but myxomas can originate from other locations on the endocardium. Calcifications are common. Myxomas occurring in children frequently are associated with Carney syndrome.15 Carney syndrome is an autosomal-dominant condition that includes cardiac myxomas, skin myxomas, hyperpigmentation, and overactivity of the endocrine system. Myxomas in children are more likely to be multiple and to recur than in adults. Clinical symptoms include obstructive cardiac symptoms, embolic phenomena, and constitutional symptoms.
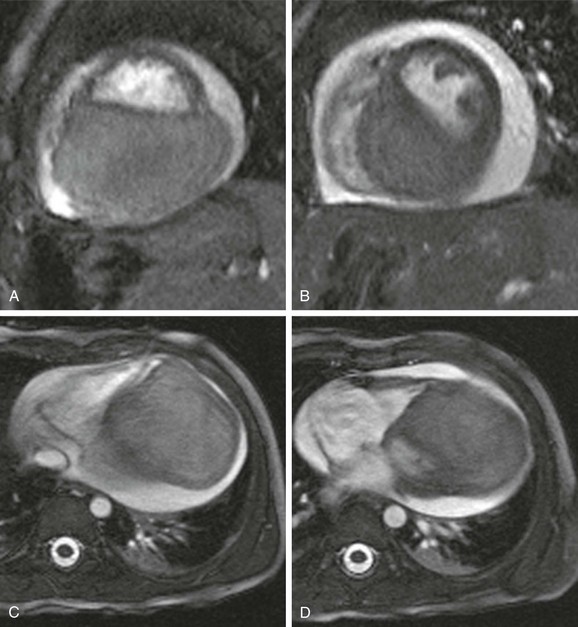
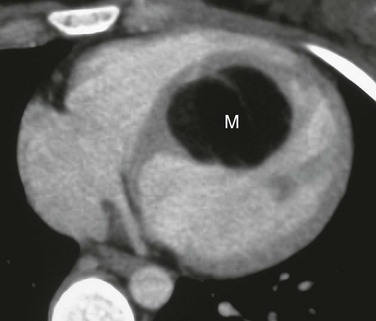
Imaging: Echocardiography identifies a heterogeneous, spherical mass attached to the endocardial surface.6,10 The pedunculated mass can be seen to prolapse across the mitral or tricuspid valve during the cardiac cycle. Myxomas have a heterogenous signal and myxoid regions; they have a low signal on T1-weighted imaging and a high signal on T2-weighted imaging6,7,9,11; and they enhance with administration of gadolinium (Fig. 81-9). Prolapse of the pedunculated mass can be identified with cine imaging.14 Tumor attenuation is lower than nonopacified blood on CT sections. Calcifications may be visualized.14 The mass is well outlined on contrast-enhanced CT scans.9
Teratoma
Pathophysiology and Clinical Presentation: Cardiac teratomas overall are rare, but they are the most common pericardial tumors in infants, and most are identified during infancy.3,10,16,17 Teratomas typically are attached to the pulmonary artery and aortic root and extend into the pericardium3,16; rarely, they originate from the myocardium.18 Pericardial effusions usually are present. Fetal hydrops from caval obstruction can lead to spontaneous abortion.
Imaging: Echocardiography, CT, and MRI show a mixed, solid, and multicystic tumor in the pericardium with a pericardial effusion3 (e-Fig. 81-10). Calcification may be present. Echocardiography shows a heterogeneous, multilocular, cystic mass that may be associated with cardiac chamber compression.10 MRI with both T1- and T2-weighted sequences can show high signal within a well-defined pericardial mass.19 Calcifications and lipids within these tumors are well defined by CT.16
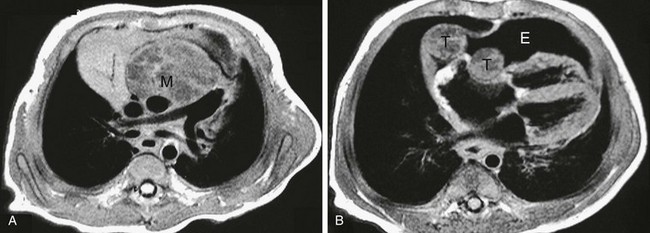
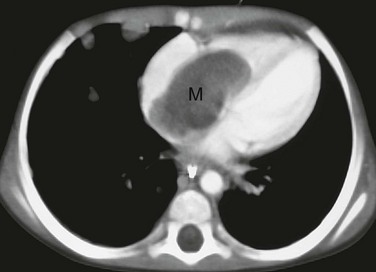
e-Figure 81-10 A pericardial teratoma in a child.
A, Axial T1-weighted magnetic resonance imaging shows a pericardial mass (M) with low-signal cystic components in a child with a pericardial teratoma. B, Daughter tumors (T) are present in the pericardial space. Note the large pericardial effusion (E).
Other Cardiac Tumors
Other benign tumors, such as fibroelastomas, hemangiomas, and lipomas, are extremely rare in children. A fibroelastoma is an intracavitary tumor rarely found in children.20,21 Unlike myxomas, fibroelastomas usually are attached to cardiac valves.20 Hemangiomas can occur in the heart and pericardium and also are associated with pericardial effusion.3 Hemangiomas enhance intensely on CT (Fig. 81-11) and have a high signal on T2-weighted sequences and postgadolinium T1-weighted sequences (Fig. 81-12).10,22 Lipomas can occur at any age but are rare in children.23 CT and MRI demonstration of fat allows for the specific diagnosis.19 (Fig. 81-13).
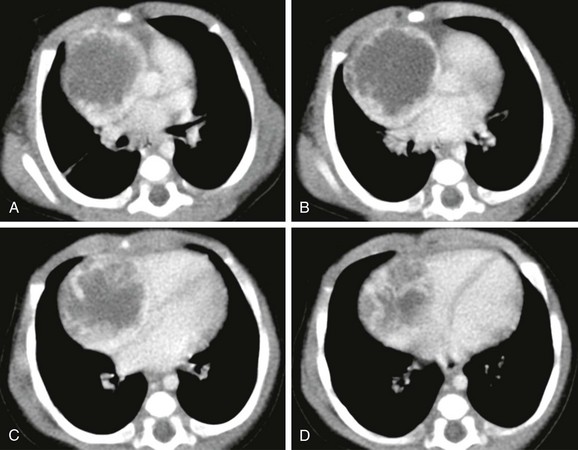
Figure 81-11 A pericardial hemangioma in a newborn.
Computed tomography shows a hypodense pericardial mass arising from the right atrial wall that compresses the right atrium. Dense peripheral contrast enhancement is present.

Figure 81-12 A pericardial hemangioma in an 8-year-old child.
Magnetic resonance shows a high-signal mass (M) on T1-weighted imaging. The mass impinges on the right ventricle.
Malignant Tumors
Primary malignant tumors are so rare that frequently they are absent from series of cardiac tumors in children, appearing only in case reports.1,2,24 Only four malignant primary cardiac tumors were confirmed in Great Britain during a 21-year period.25 Sarcomas (Fig. 81-14),26 primary lymphoma,27 and kaposiform hemangioendothelima28 of the heart have been reported in children. Primary cardiac lymphoma is defined as lymphoma restricted to the heart and pericardium (Fig. 81-15). Kaposiform hemangioendothelioma can occur antenatally and is associated with pericardial effusion. CT shows a soft tissue mass without fat and MRI shows a high signal on T2-weighted images. Contrast uptake is similar to hemangiomas (Fig. 81-16). Metastatic tumors are more common than primary cardiac malignancies19 and may be the result of leukemia, lymphoma, Wilms tumor, hepatoblastoma, neuroblastoma, Ewing sarcoma, and osteosarcoma. Spread may be from direct extension, by tumor extension through the inferior vena cava (Fig. 81-17), or via hematogenous metastases.
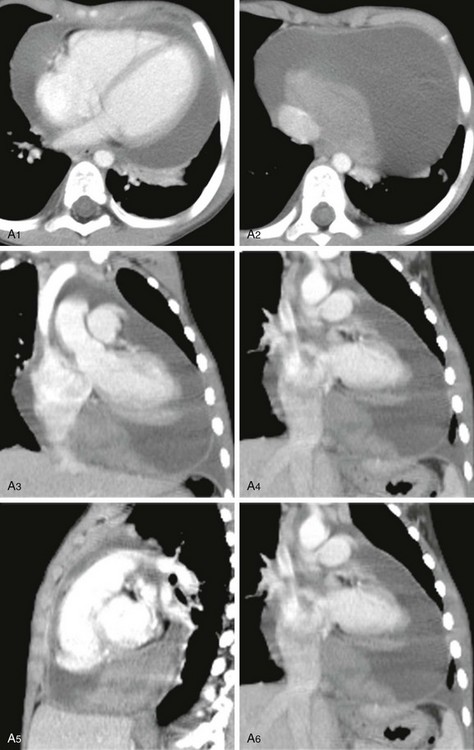
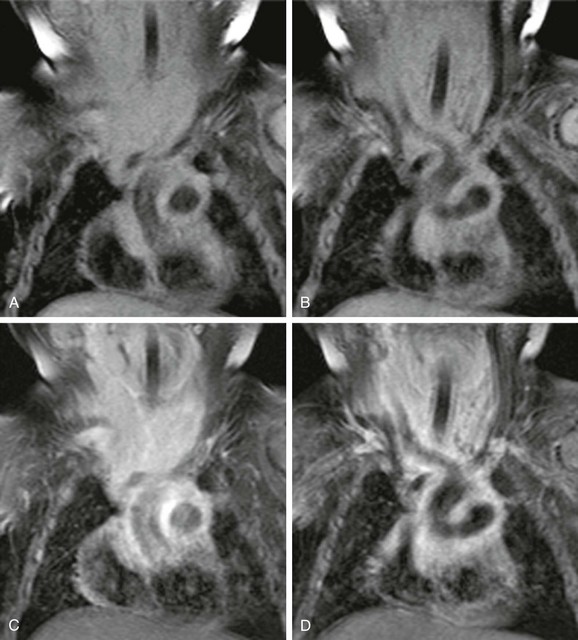
e-Figure 81-14 A pericardial synovial sarcoma in a 6-year-old child who presented with chest pain.
A, Computed tomography images (1 through 6) show a large pericardial effusion with a focal soft tissue density mass at the base of the pericardium adjacent to the right atrium. B, Coronal fast spin echo (1 through 3) and axial T2-weighted magnetic resonance imaging (4 through 6) show the pericardial effusion and a mass with slight hyperintensity on T2-weighted images.
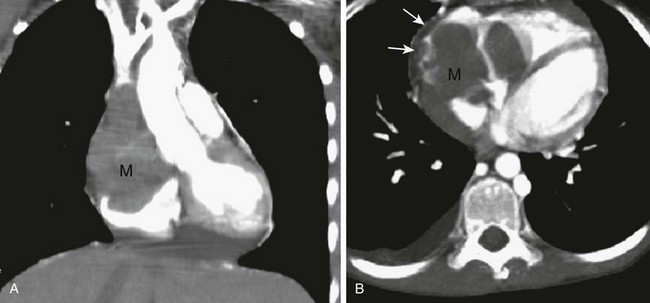
e-Figure 81-15 A primary cardiac lymphoma in a child.
Coronal (A) and axial (B) computed tomography images show a low-attenuation mass (M) involving the pericardium (arrows in B) and right heart.
e-Figure 81-16 A kaposiform hemangioendothelioma in a 1-month-old child who presented initially with a pericardial effusion.
Coronal T1-weighted precontrast and postcontrast magnetic resonance images show an infiltrative enhancing vascular mass encasing the great vessels and airway.
Beroukhim, RS, Prakash, A, Valsangiacomo Buechel, ER, et al. Characterization of cardiac tumors in children by cardiovascular magnetic resonance imaging. J Am Coll Cardiol. 2011;58:1044–1054.
Bruce, CJ. Cardiac tumours: diagnosis and management. Heart. 2011;97:151–160.
Isaacs, H. Fetal and neonatal cardiac tumors. Pediatr Cardiol. 2004;25:252–273.
Salanitri, J, Lisle, D, Rigsby, C, et al. Benign cardiac tumours: cardiac CT and MRI imaging appearances. J Med Imaging Radiat Oncol. 2008;52(6):550–558.
Van Beek, EJR, Stolpen, AH, Khanna, G, et al. CT and MRI of pericardial and cardiac neoplastic disease. Cancer Imaging. 2007;7:19–26.
References
1. Freedom, RM, Lee, KJ, Macdonald, C, et al. Selected aspects of cardiac tumors in infancy and childhood. Pediatr Cardiol. 2000;21:299–316.
2. Yinon, Y, Chitayat, D, Blaser, S, et al. Fetal cardiac tumors: a single-center experience of 40 years. Prenat Diagn. 2010;30:941–949.
3. Isaacs, H. Fetal and neonatal cardiac tumors. Pedatr Cardiol. 2004;25:252–273.
4. Tworetzky, W, McElhinney, DB, Margossian, R, et al. Association between cardiac tumors and tuberous sclerosis in the fetus and neonate. Am J Cardiol. 2003;92:487–489.
5. Pipitone, S, Mongiovi, M, Grillo, R, et al. Cardiac rhabdomyoma in intrauterine life: clinical features and natural history. A case series and review of published reports. Ital Heart J. 2002;3:48–52.
6. Kaminaga, T, Takeshita, T, Kimura, I. Role of magnetic resonance imaging for evaluation of tumors in the cardiac region. Eur Radiol. 2003;13(suppl 4):L1–L10.
7. Syed, IS, Feng, D, Harris, SR, et al. MR imaging of cardiac masses. Magn Reson Imaging Clin N Am. 2008;16:137–164.
8. Sugiyama, H, Naito, H, Tsukano, S, et al. Evaluation of cardiac tumors I children by electron-beam computed tomography: rhabdomyoma and fibroma. Circ J. 2005;69:1352–1356.
9. Salanitri, J, Lisle, D, Rigsby, C, et al. Benign cardiac tumours: cardiac CT and MRI imaging appearances. M Med Imaging Radiat Oncol. 2008;52:550–558.
10. Grebenc, ML, Rosado de Christenson, ML, Burke, AP, et al. Primary cardiac and pericardial neoplasms: radiologic-pathologic correlation. Radiographics. 2000;20:1073–1103.
11. Grizzard, JD, Ang, GB. Magnetic resonance imaging of pericardial disease and cardiac masses. Magn Reson Imaging Clin N Am. 2007;15:579–607.
12. Kiaffas, MG, Powell, AJ, Geva, T. Magnetic resonance imaging evaluation of cardiac tumor characteristics in infants and children. Am J Cardiol. 2002;15:1229–1233.
13. De Cobelli, F, Esposito, A, Mellone, R, et al. Images I cardiovascular medicine. Late enhancement of a left ventricular cardiac fibroma assessed with gadolinium-enhanced cardiovascular magnetic resonance. Circulation. 2005;112:e242–e243.
14. Schvartzman, PR, White, RD. Imaging of cardiac and paracardiac masses. J Thorac Imaging. 2000;15:265–273.
15. Mahilmaran, A, Seshadri, M, Nayar, PG, et al. Familial cardiac myxoma: Carney’s complex. Tex Heart Inst J. 2003;30:80–82.
16. Taori, K, Jawale, R, Sanyal, R, et al. Intrapericardial teratoma diagnosed on CT. J Thorac Imaging. 2007;22:185–187.
17. Reddy, SC, Fenton, KM, Gandhi, SK, et al. Intrapericardial teratoma in a neonate. Ann Thorac Surg. 2003;76:626.
18. Patel, A, Rigsby, C, Young, L. Cardiac teratoma of the interventricular septum with congenital aortic stenosis in a newborn. Pedatr Cardiol. 2008;29:1126–1128.
19. Van Beek, EJR, Stolpen, AH, Khanna, G, et al. CT and MRI of pericardial and cardiac neoplastic disease. Cancer Imaging. 2007;7:19–26.
20. Gowda, RM, Khan, IA, Nair, CK, et al. Cardiac papillary fibroelastoma: a comprehensive analysis of 725 cases. Am Heart J. 2003;146:404–410.
21. Sridar, AV, Bulock, F, Hickey, MS, et al. Papillary fibroelastoma of the tricuspid valve presenting as neonatal pulmonary haemorrhage. Acta Paediatr. 2004;93:1254–1256.
22. Sparrow, PJ, Kurian, JB, Jones, TR, et al. MR imaging of cardiac tumors. Radiographics. 2005;25:1255–1276.
23. Gan, C, An, Q, Tao, K, et al. An asymptomatic lipoma of the right atrium in a neonate. J Pediatr Surg. 2008;43:1920–1922.
24. Sánchez Andrés, A, Insa Albert, B, Carrasco Moreno, JI, et al. Primary cardiac tumours in infancy. An Pediatr (Barc). 2008;69:15–22.
25. Barnes, WS, Craft, AW, Hunter, AS, et al. Primary malignant cardiac tumors in children. Pediatr Hematol Oncol. 1986;3:347–351.
26. Romanos-Sirakis, EC, Meyer, DB, Chun, A, et al. A primary cardiac sarcoma with features of a desmosplastic small round cell tumor in an adolescent male. J Pedatr Hematol Oncol. 2010;32:236–239.
27. Patel, J, Melly, L, Sheppard, MN. Primary cardiac lymphoma: B- and T-cell cases at a specialist UK centre. Ann Oncol. 2010;21:1041–1045.
28. Walsh, MA, Carcao, M, Pope, E, et al. Kaposiform hemangioendothelioma presenting antenatally with pericardial effusion. J Pediatr Hematol Oncol. 2008;30:761–763.