42
Calcinosis Cutis and Osteoma Cutis
There are four major forms of cutaneous calcification (calcinosis cutis): (1) dystrophic – locally within sites of pre-existing skin damage; (2) metastatic – due to systemic metabolic derangements; (3) iatrogenic – secondary to medical treatment or testing; and (4) idiopathic. Cutaneous ossification (osteoma cutis) occurs in the setting of several genetic disorders, in a miliary form on the face and within neoplasms and sites of inflammation (secondary).
Calcinosis Cutis
Calcinosis Cutis – Dystrophic
• Often seen in autoimmune connective tissue diseases (AI-CTDs), in particular the limited form of systemic sclerosis (also referred to as CREST syndrome) and childhood dermatomyositis (Figs. 42.1 and 42.2); in the former, hard, skin-colored to white papules overlie the bony prominences of the extremities (upper > lower), whereas in the latter the deposits are often larger and sometimes plate-like.

Fig. 42.1 Dystrophic form of calcinosis cutis. Note the cluster of small white papules in this patient with the limited form of systemic sclerosis (also referred to as CREST syndrome). Courtesy, Janet Fairley, MD.

Fig. 42.2 Radiograph of calcinosis cutis in a patient with generalized morphea. Areas that were previously firm became rock-hard, and lesions of perforating calcinosis cutis (transepidermal elimination) developed on both legs. Courtesy, Jean L. Bolognia, MD.
• Extrusion (transepidermal elimination or ‘perforation’; see Ch. 79) of the calcium deposits appears as a white chalky material and it can be followed by a persistent ulceration.
• Other underlying causes are listed in Table 42.1.
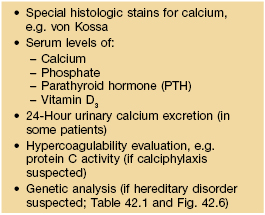
Table 42.1
Disorders of cutaneous calcification.
* Can occasionally occur in the setting of severe primary hyperparathyroidism and, less often, in the absence of a clearly identifiable trigger.
EEG, electroencephalogram; EMG, electromyography; SCC, squamous cell carcinoma.

Fig. 42.3 Dystrophic calcification in an infant at the site of a previous ‘heel stick’ for obtaining blood. Courtesy, Julie V. Schaffer, MD.
• Rx: aggressive treatment of AI-CTDs, when possible, prior to the appearance of calcinosis cutis; excision of symptomatic localized deposits, if feasible; sodium thiosulfate and calcium channel blockers, e.g. diltiazem, may be effective in some patients.
Calcinosis Cutis – Metastatic
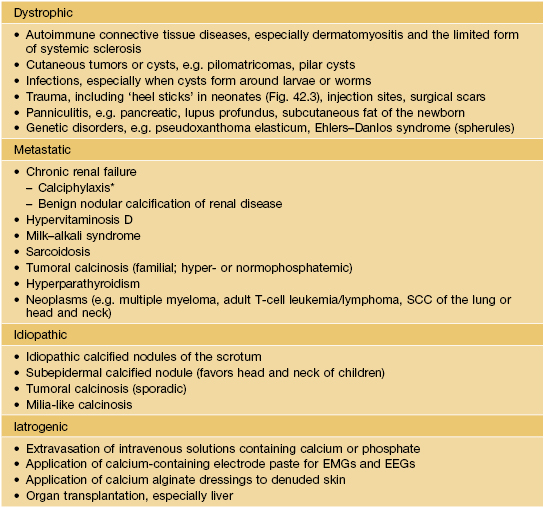
• The most common cause is end-stage renal disease with its associated hyperphosphatemia and decreased 1,25-dihydroxyvitamin D levels (Fig. 42.4).
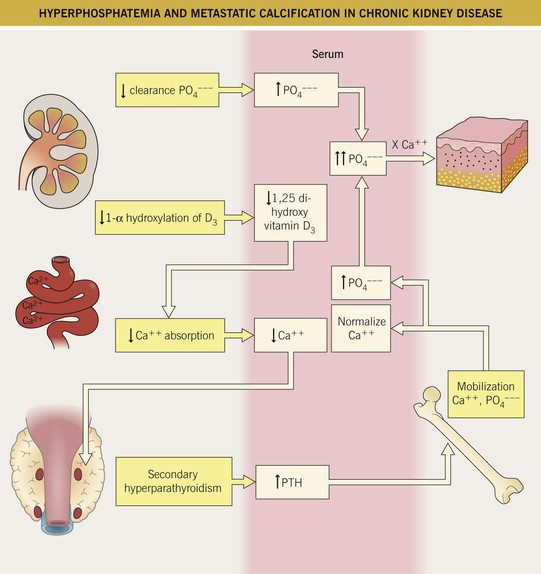
Fig. 42.4 Mechanisms of hyperphosphatemia and metastatic calcification in patients with chronic kidney disease.
• Calciphylaxis is characterized by cutaneous ischemia and necrosis which presents as markedly painful retiform purpura and ulcerations (Fig. 42.5); risk factors include obesity and hypercoagulability (e.g. protein C dysfunction); deposits of calcium within blood vessel walls of the subcutis are usually present, but not always, presumably due to sampling error.


Fig. 42.5 Calciphylaxis in two patients with chronic kidney disease. A, B Characteristic painful reticulated purpuric plaques that can develop ulceration. A, Courtesy, Kalman Watsky, MD.
Calcinosis Cutis – Iatrogenic and Idiopathic
Osteoma Cutis
• Deposition of a protein matrix plus hydroxyapatite (Ca++, PO4– – –) within the skin.
• The four genetic disorders that often have cutaneous or subcutaneous ossification are outlined in Fig. 42.6.
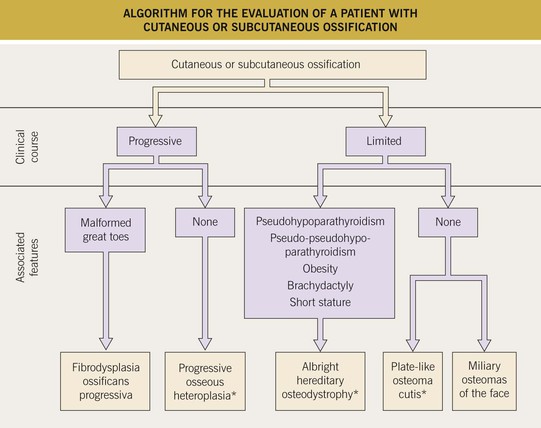
Fig. 42.6 Algorithm for the evaluation of a patient with cutaneous or subcutaneous ossification. *Associated with mutations in GNAS1, which encodes the alpha subunit of the stimulatory G protein that regulates adenyl cyclase activity (thought to be negative regulator of bone formation); clinical phenotype may be a reflection of imprinting.
• Miliary osteomas of the face is a rather common entity; small hard papules, whose color can vary from white or skin-colored to blue (Fig. 42.7), gradually appear on the face of adult women > men; the role of pre-existing acne vulgaris and its treatment with oral antibiotics is debated.


Fig. 42.7 Miliary osteomas of the face. A Small, white, firm papules in a patient without a history of acne. B Multiple blue-colored papules in a patient with a history of acne vulgaris. A, Courtesy, Janet Fairley, MD.
• Ossification can also occur within cysts and tumors (e.g. pilomatricomas, melanocytic nevi) as well as at sites of inflammation; it is often preceded by cutaneous calcification.
The evaluation of a patient with calcinosis cutis or osteoma cutis is outlined in Table 42.2.
For further information see Ch. 50. From Dermatology, Third Edition.