Chapter 66 Burns and Frostbite
3 How are thermal injuries classified?
 First degree: Thermal injury only affects the epidermis—sunburn.
First degree: Thermal injury only affects the epidermis—sunburn.
 Second degree: Thermal injury affects the epidermis and superficial dermis. The injury results in blistering and mild to moderate edema to the affected area. The wound is painful because of damaged nerves but should heal with simple topical antimicrobials in approximately 14 to 21 days.
Second degree: Thermal injury affects the epidermis and superficial dermis. The injury results in blistering and mild to moderate edema to the affected area. The wound is painful because of damaged nerves but should heal with simple topical antimicrobials in approximately 14 to 21 days.
 Third degree: The thermal injury affects both the epidermis and dermis. A true third-degree thermal injury should be without pain because of the complete destruction of the sensory nerves. However, few thermal injuries are composed of only one class of injury. The majority of deep thermal injuries are a mixture of depths, thus making lack of sensation a poor marker to classify depth of injury. A more specific marker of a third-degree thermal injury is the white and leathery appearance. Healing of a third-degree thermal injury will require excision and grafting.
Third degree: The thermal injury affects both the epidermis and dermis. A true third-degree thermal injury should be without pain because of the complete destruction of the sensory nerves. However, few thermal injuries are composed of only one class of injury. The majority of deep thermal injuries are a mixture of depths, thus making lack of sensation a poor marker to classify depth of injury. A more specific marker of a third-degree thermal injury is the white and leathery appearance. Healing of a third-degree thermal injury will require excision and grafting.
 Fourth degree: Thermal injuries that affect structure deep to the skin–fat, fascia, muscle, and/or bone. Treatment and presentation are similar to those of third-degree thermal injuries.
Fourth degree: Thermal injuries that affect structure deep to the skin–fat, fascia, muscle, and/or bone. Treatment and presentation are similar to those of third-degree thermal injuries.
9 Who should be referred to a verified burn center?
 Partial thickness burns greater than 10% TBSA
Partial thickness burns greater than 10% TBSA
 Burns involving the face, hands, feet, genitalia, perineum, or major joints
Burns involving the face, hands, feet, genitalia, perineum, or major joints
 Third-degree burns in any age group
Third-degree burns in any age group
 Electrical burns, including lightning injury
Electrical burns, including lightning injury
 Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality
Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality
 Any patient with burns and concomitant trauma in which the burn injury poses the greatest risk of morbidity or mortality
Any patient with burns and concomitant trauma in which the burn injury poses the greatest risk of morbidity or mortality
 Burned children in hospitals without qualified personnel or equipment for the care of children
Burned children in hospitals without qualified personnel or equipment for the care of children
 Burn injury in patients who will require special social, emotional, or long-term rehabilitative intervention
Burn injury in patients who will require special social, emotional, or long-term rehabilitative intervention
11 What is burn-induced hypermetabolism?
12 What are the four main advances in burn care that have dramatically reduced mortality over the last 50 years?
 Appropriate resuscitation: Restoration of end-organ perfusion while avoiding overresuscitation.
Appropriate resuscitation: Restoration of end-organ perfusion while avoiding overresuscitation.
 Control of infection: Application of topical antimicrobial agents to prevent wound infections and using systemic antimicrobials only after documentation of invasive wound infection (cellulitis), not colonization, and presence of systemic infection (bacteremia).
Control of infection: Application of topical antimicrobial agents to prevent wound infections and using systemic antimicrobials only after documentation of invasive wound infection (cellulitis), not colonization, and presence of systemic infection (bacteremia).
 Modulation of hypermetabolism: Early and appropriate nutrition, anabolic agents, early occupational and physical therapy.
Modulation of hypermetabolism: Early and appropriate nutrition, anabolic agents, early occupational and physical therapy.
 Early excision and grafting: Protein catabolism progressively worsens with the presence of third-degree thermal injury. The goal is to remove all nonviable tissue within 96 hours to lessen the degree of catabolism.
Early excision and grafting: Protein catabolism progressively worsens with the presence of third-degree thermal injury. The goal is to remove all nonviable tissue within 96 hours to lessen the degree of catabolism.
14 How are electrical injuries treated?
 First, all patients must be evaluated for potential cardiac dysrhythmias; however, if absent, the most recent data would suggest no clinical need for continued cardiac monitoring.
First, all patients must be evaluated for potential cardiac dysrhythmias; however, if absent, the most recent data would suggest no clinical need for continued cardiac monitoring.
 Second, all patients should be suspected of having deep tissue damage, particularly when voltages are greater than 600 V.
Second, all patients should be suspected of having deep tissue damage, particularly when voltages are greater than 600 V.
 Finally, all patients should have a baseline eye examination to rule out cataracts because of the potential for cataract formation after any significant electrical injury.
Finally, all patients should have a baseline eye examination to rule out cataracts because of the potential for cataract formation after any significant electrical injury.
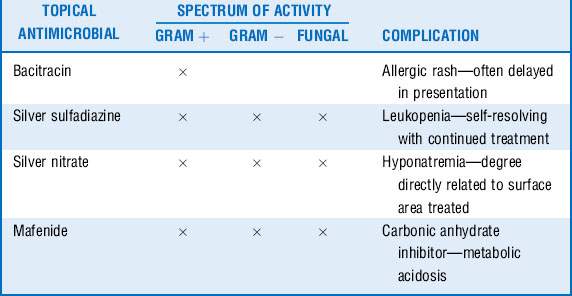
16 What are the known and common complications of topical antimicrobials?
Topical antimicrobial therapy is the mainstay of the treatment for small and large thermal injuries. Although most antimicrobials have a broad range of activity against gram-positive and gram-negative organisms (silver sulfadiazine [Silvadene], silver nitrate, mafenide [Sulfamylon]), some have a narrow spectrum of activity but work well on minor thermal injuries (bacitracin, mupirocin [Bactroban]). As with any pharmacologic agent, a physician must know the indications and potential complications of the agent being prescribed. Although most topical antimicrobials are well tolerated, several have known complications associated with them. See Table 66-1.
Key Points Burns and frostbite
1. Thermal injuries are classified by the extent of damage to the skin’s underlying structure; the physiologic impact is dependent on the extent of second- and third-degree injury.
2. All patients who have a thermal injury should have a complete primary and secondary survey performed with particular attention to airway (potential obstruction) and circulation (potential compartment syndrome).
3. Burn shock is not simply a state of hypovolemia; appropriate resuscitation is mandatory to avoid morbidity and mortality.
4. Burn-induced hypermetabolism is a significant metabolic disturbance following a major thermal injury. Proper nutrition coupled with early excision, grafting, and exercise is the best treatment.
5. Hypocalcemia can develop after exposure to concentrated hydrofluoric acid.
6. Frostbite injuries should be treated with rapid rewarming and potential catheter-directed thrombolysis.
1 American Burn Association. Advanced burn life support providers manual. Chicago: American Burn Association; 2005.
2 Barrow R.E., Jeschke M.G., Herndon D.N. Early fluid resuscitation improves outcomes in severely burned children. Resuscitation. 2000;45:91–96.
3 Bruen K.J., Ballard J.R., Morris S.E., et al. Reduction of the incidence of amputation in frostbite injury with thrombolytic therapy. Arch Surg. 2007;142:546–551.
4 Greenhalgh D.G. Topical antimicrobial agents for burn wounds. Clin Plast Surg. 2009;36:597–606.
5 Hart D.W., Wolf S.E., Chinkes D.L., et al. Effects of early excision and aggressive enteral feeding on hypermetabolism, catabolism, and sepsis after severe burn. J Trauma. 2003;54:755–761.
6 Herndon D.N., Tompkins R.G. Support of the metabolic response to injury. Lancet. 2004;363:1895–1902.
7 Jeschke M.G., Chinkes D.L., Finnery C.C., et al. Pathophysiologic response to severe burn injury. Ann Surg. 2008;248:387–401.
8 Kirkpatrick J.J., Enion D.S., Burd D.A. Hydrofluoric acid burns: a review. Burns. 1995;21:483–493.
9 Klein M.B., Hayden D., Elson C. The association between fluid administration and outcome following major burn: a multicenter study. Ann Surg. 2007;245:622–628.
10 Krammer G.C., Lund T., Beckum O.L. Pathophysiology of burn shock and burn edema. In: Herndon D.N., ed. Total Burn Care. 3rd ed. Philadelphia: Saunders; 2007:93–106.
11 Pham T.N., Gibran N.S., Heimbach D.M. Evaluation of the burn wound: management decisions. In: Herndon D.N., ed. Total Burn Care. 3rd ed. Philadelphia: Saunders; 2007:119–126.
12 Rosen C.L., Adler J.N., Rabban J.T., et al. Early predictors of myoglobinuria and acute renal failure following electrical injury. J Emerg Med. 1999;17:783–789.
13 Sheridan R.L. Comprehensive treatment of burns. Curr Probl Surg. 2001;38:657–756.
14 Sheridan R.L., Ryan C.M., Quinby W.C.Jr. et al: Emergency management of major hydrofluoric acid exposures. Burns. 1995;21:62–64.
15 Sullivan S.R., Ahmadi A.J., Singh C.N., et al. Elevated orbital pressure: another untoward effect of massive resuscitation after burn injury. J Trauma. 2006;60:72–76.