Chapter 68 Burn Injuries
Epidemiology
Approximately 1.2 million people in the USA require medical care for burn injuries each year, with 51,000 requiring hospitalization. Approximately 30-40% of these patients are younger than 15 yr, with an average age of 32 mo. Fires are a major cause of mortality in children, accounting for up to 34% of fatal injuries in those younger than 16 yr. Scald burns account for 85% of total injuries and are most prevalent in children younger than 4 yr. Although the incidence of hot water scalding has been reduced by legislation requiring new water heaters to be preset at 120°F, scald injury remains the leading cause of hospitalization for burns. Steam inhalation used as a home remedy to treat respiratory infections is another potential cause of burns. Flame burns account for 13%; the remaining are electrical and chemical burns. Clothing ignition events have declined since passage of the Federal Flammable Fabric Act requiring sleepwear to be flame-retardant; however, the U.S. Consumer Product Safety Commission has voted to relax the existing children’s sleepwear flammability standard. Approximately 18% of burns are the result of child abuse (usually scalds), making it important to assess the pattern and site of injury and their consistency with the patient history (Chapter 37). Friction burns from treadmills are also a problem. Hands are the most commonly injured sites, with deep 2nd-degree friction injury sometimes associated with fractures of the fingers. Anoxia, not the actual burn, is a major cause of morbidity and mortality in house fires.
Review of the history usually shows a common pattern: scald burns to the side of the face, neck, and arm if liquid is pulled from a table or stove; burns in the pant leg area if clothing ignites; burns in a splash pattern from cooking; and burns on the palm of the hand from contact with a hot stove. However, “glove or stocking” burns of the hands and feet, single-area deep burns on the trunk, buttocks, or back, and small, full-thickness burns (cigarette burns) in young children should raise the suspicion of child abuse (Chapter 37).
Prevention
The aim of burn prevention is a continuing reduction in the number of serious burn injuries (Table 68-1). Effective first aid and triage can decrease both the extent (area) and the severity (depth) of injuries. The use of flame-retardant clothing and smoke detectors, control of hot water temperature (thermostat settings) within buildings, and prohibition of cigarette smoking have been partially successful in reducing the incidence of burn injuries. Treatment of children with significant burn injuries in dedicated burn centers facilitates medically effective care, improves survival, and leads to greater cost efficiency. Survival of at least 80% of patients with burns of 90% of the body surface area (BSA) is possible; the overall survival rate of children with burns of all sizes is 99%. Death is more likely in children with irreversible anoxic brain injury sustained at the time of the burn.
Acute Care, Resuscitation, and Assessment
Indications for Admission
Burns covering >10-15% of total BSA, burns associated with smoke inhalation, burns resulting from high-tension (voltage) electrical injuries, and burns associated with suspected child abuse or neglect should be treated as emergencies, and the child hospitalized (Table 68-2). Small 1st- and 2nd-degree burns of the hands, feet, face, perineum, and joint surfaces also require admission if close follow-up care is difficult to provide. Children who have been in enclosed-space fires and those who have face and neck burns should be hospitalized for at least 24 hr for observation for signs of central nervous system (CNS) effects of anoxia from carbon monoxide poisoning and pulmonary effects from smoke inhalation.
First Aid Measures
Acute care should include the following measures:
Emergency Care
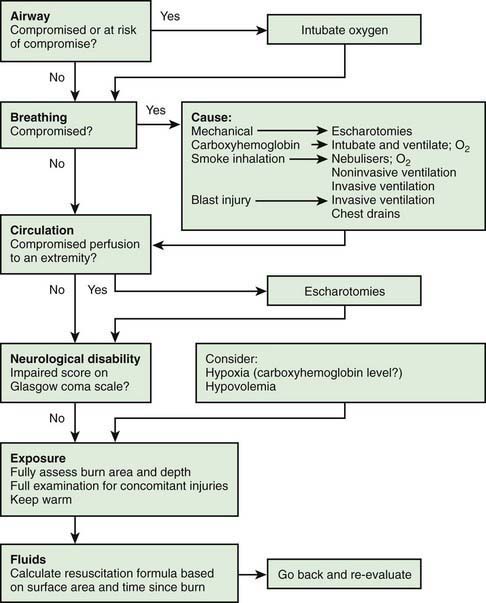
Life support measures are as follows (Table 68-3):
Classification of Burns
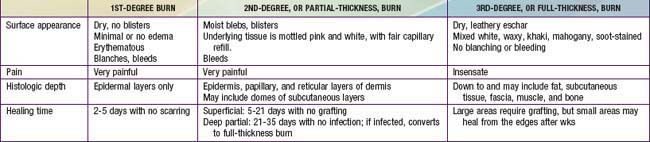
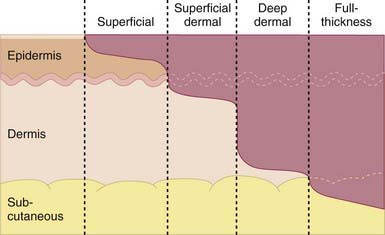
Proper triage and treatment of burn injury require assessment of the extent and depth of the injury (Table 68-4 and Fig. 68-2). 1st-degree burns involve only the epidermis and are characterized by swelling, erythema, and pain (similar to mild sunburn). Tissue damage is usually minimal, and there is no blistering. Pain resolves in 48-72 hr; in a small percentage of patients, the damaged epithelium peels off, leaving no residual scars.
Estimation of Body Surface Area for a Burn
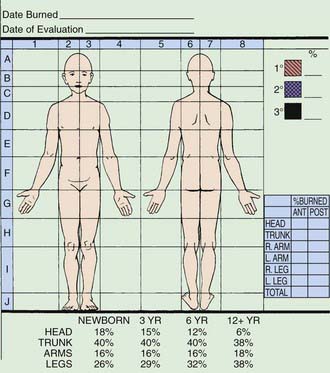
Appropriate burn charts for different childhood age groups should be used to accurately estimate the extent of BSA burned. The volume of fluid needed in resuscitation is calculated from the estimation of the extent and depth of burn surface. Mortality and morbidity also depend on the extent and depth of the burn. The variable growth rate of the head and extremities throughout childhood makes it necessary to use BSA charts, such as that modified by Lund and Brower or the chart used at the Shriners Hospital for Children in Boston (Fig. 68-3). The rule of nines used in adults may be used only in children older than 14 yr or as a very rough estimate to institute therapy before transfer to a burn center. In small burns, <10% of BSA, the rule of palm may be used, especially in outpatient settings: The area from the wrist crease to the finger crease (the palm) in the child equals 1% of the child’s BSA.
Treatment
Outpatient Management of Minor Burns
A patient with 1st- and 2nd-degree burns of <10% of BSA may be treated on an outpatient basis unless family support is judged inadequate or there are issues of child neglect or abuse. These outpatients do not require a tetanus booster (unless not truly immunized) or prophylactic penicillin therapy. Blisters should be left intact and dressed with bacitracin or silver sulfadiazine cream (Silvadene). Dressings should be changed once daily, after the wound is washed with lukewarm water to remove any cream left from the previous application. Very small wounds, especially those on the face, may be treated with bacitracin ointment and left open. Debridement of the devitalized skin is indicated when the blisters rupture. A variety of wound dressings/wound membranes are available (e.g., AQUACEL Ag dressing [ConvaTec USA, Skillman, NJ] in a soft feltlike material impregnated with silver ion) may be applied to 2nd-degree burns and wrapped with a dry sterile dressing; similar wound membranes provide pain control, prevention of wound desiccation, and reduction in wound colonization (Table 68-5). These dressings are usually kept on for 7-10 days but are checked twice a week.
Table 68-5 PARTIAL LISTING OF SOME COMMONLY USED WOUND MEMBRANES—SELECTED CHARACTERISTICS
| MEMBRANE | CHARACTERISTIC(S) |
|---|---|
| Porcine xenograft |
The depth of scald injuries is difficult to assess early; conservative treatment is appropriate initially, with the depth of the area involved determined before grafting is attempted (Fig. 68-4). This approach obviates the risk of anesthesia and unnecessary grafting.
Fluid Resuscitation
For most children, the Parkland formula is an appropriate starting guideline for fluid resuscitation (4 mL lactated Ringer solution /kg/% BSA burned). Half of the fluid is given over the 1st 8 hr, calculated from the time of onset of injury; the remaining fluid is given at an even rate over the next 16 hr. The rate of infusion is adjusted according to the patient’s response to therapy. Pulse and blood pressure should return to normal, and an adequate urine output (>1 mL/kg/hr in children; 0.5-10 mL/kg/hr in adolescents) should be accomplished by varying the IV infusion rate. Vital signs, acid-base balance, and mental status reflect the adequacy of resuscitation. Because of interstitial edema and sequestration of fluid in muscle cells, patients may gain up to 20% over baseline (pre-burn) body weight. Patients with burns of 30% of BSA require a large venous access (central venous line) to deliver the fluid required over the critical 1st 24 hr. Patients with burns of >60% of BSA may require a multilumen central venous catheter; these patients are best cared for in a specialized burn unit. In addition to fluid resuscitation, children should receive standard maintenance fluids (Chapter 53).
Prevention of Infection and Surgical Management of the Burn Wound
Mortality related to burn injury is associated not with the toxic effect of thermally injured skin, but with the metabolic and bacterial consequences of a large open wound, reduction of the patient’s host resistance, and malnutrition. These abnormalities set the stage for life-threatening bacterial infection originating from the burn wound. Wound treatment and prevention of wound infection also promote early healing and improve aesthetic and functional outcomes. Topical treatment of the burn wound with 0.5% silver nitrate solution, silver sulfadiazine cream, or mafenide acetate (Sulfamylon) cream or topical solution aims at prevention of infection (Table 68-6). These 3 agents have tissue-penetrating capacity. Regardless of the choice of topical antimicrobial agent, it is essential that all 3rd-degree burn tissue be fully excised before bacterial colonization occurs and that the area be grafted as early as possible to prevent deep wound sepsis. Children with a burn of >30% of BSA should be housed in a bacteria-controlled nursing unit to prevent cross-contamination and to provide a temperature- and humidity-controlled environment to minimize hypermetabolism.
| AGENT | EFFECTIVENESS | EASE OF USE |
|---|---|---|
| Silver sulfadiazine | Broad spectrum | Closed dressings |
| Silvadene cream | Good penetration | Changed twice daily |
| Residue must be washed off with each dressing change | ||
| Mafenide acetate | Broad spectrum, including Pseudomonas |
Topical Therapy
Topical therapy is widely used and is effective against most burn pathogens (see Table 68-6). A number of topical agents are used: 0.5% silver nitrate solution, sulfacetamide acetate cream or solution, silver sulfadiazine cream, and Accuzyme ointment or AQUACEL Ag+. Accuzyme is an enzymatic debridement agent and may cause a stinging feeling for 15 min after application. Preferences vary among burn units. Each topical agent has advantages and disadvantages in application, comfort, and bacteriostatic spectrum. Sulfacetamide acetate is a very effective broad-spectrum agent with the ability to diffuse through the burn eschar; it is the treatment of choice for injury to cartilaginous surfaces, such as the ears. The carbonic anhydrase inhibition activity of sulfacetamide may cause acid-base imbalance if large surface areas are treated, and adverse reactions to the sulfur-containing agents may produce transient leukopenia. This latter reaction is mostly noted with the use of silver sulfadiazine cream when applied over large surface areas in children younger than 5 yr. This phenomenon is transient, self-limiting, and reversible. No sulfa-containing agent should be used if the child has a history of sulfa allergies.
Inhalational Injury
Inhalational injury is serious in the infant and child, particularly if pre-existing pulmonary conditions are present (Chapter 65). Mortality estimates vary, depending on the criteria for diagnosis, but are 45-60% in adults; exact figures are not available in children. Evaluation aims at early identification of inhalation airway injuries. These may occur from (1) direct heat (greater problems with steam burns), (2) acute asphyxia, (3) carbon monoxide poisoning, and (4) toxic fumes, including cyanides from combustible plastics. Sulfur and nitrogen oxides and alkalis formed during the combustion of synthetic fabrics produce corrosive chemicals that may erode mucosa and cause significant tissue sloughing. Exposure to smoke may cause degradation of surfactant and decrease its production, resulting in atelectasis. Inhalation injury and burn injury are synergistic, and the combined effect can increase morbidity and mortality.
Signs of CNS injury from hypoxemia due to asphyxia or carbon monoxide poisoning vary from irritability to depression. Carbon monoxide poisoning may be mild (<20% HbCO), with slight dyspnea, headache, nausea, and decreased visual acuity and higher cerebral functions; moderate (20-40% HbCO), with irritability, agitation, nausea, dimness of vision, impaired judgment, and rapid fatigue; or severe (40-60% HbCO), producing confusion, hallucination, ataxia, collapse, acidosis, and coma. Measurement of HbCO is important for diagnosis and treatment. The PaO2 value may be normal and the HbCO saturation values misleading because HbCO is not detected by the usual tests of oxygen saturation. Carbon monoxide poisoning is assumed until the tests are performed, and it is treated with 100% oxygen. Significant carbon monoxide poisoning requires hyperbaric oxygen therapy (Chapter 58).
School Reentry and Long-Term Outcome
Major advances have made it possible to save the lives of children with massive burns; whereas some children have had lingering physical difficulties, most have a satisfactory quality of life. The comprehensive burn care that includes experienced multidisciplinary aftercare plays an important role in recovery. Long-term complications of burns are listed in Table 68-7.
Table 68-7 COMMON LONG-TERM DISABILITIES IN PATIENTS WITH BURN INJURIES
DISABILITIES AFFECTING THE SKIN AND SOFT TISSUE
ORTHOPEDIC DISABILITIES
METABOLIC DISABILITIES
PSYCHIATRIC AND NEUROLOGIC DISABILITIES
LONG-TERM COMPLICATIONS OF CRITICAL CARE
PRE-EXISTING DISABILITIES THAT CONTRIBUTED TO THE INJURIES
Modified from Sheridan RL, Schultz JT, Ryan CM, et al: Case records of the Massachusetts General Hospital: weekly clinicopathological exercises: case 6-2004: a 35-year-old woman with extensive, deep burns from a nightclub fire, N Engl J Med 350:810–821, 2004.
Special Situations
Electrical Burns
A more serious category of electrical burn is the high-tension electrical wire burn, for which children must be admitted for observation, regardless of the extent of the surface area burn. Deep muscle injury is typical and cannot be readily assessed initially. These injuries result from high voltage (>1,000 V) and occur particularly at high-voltage installations, such as electric power stations or railroads; children climb an electric pole and touch an electric box out of curiosity or accidentally touch a high-tension electric wire. Such injuries have a mortality rate of 3-15% for children who arrive at the hospital for treatment. Survivors have a high rate of morbidity, including major limb amputations. Points of entry of current through the skin and the exit site show characteristic features consistent with current density and heat. The majority of entrance wounds involve the upper extremity, with small exit wounds in the lower extremity. The electrical path, from entrance to exit, takes the shortest distance between the 2 points and may produce injury in any organ or tissue in the path of the current. Multiple exit wounds in some patients attest to the possibility of several electrical pathways in the body, placing virtually any structure in the body at risk (Table 68-8). Damage to the abdominal viscera, thoracic structures, and the nervous system in areas remote from obvious extremity injury occurs and must be sought, particularly in injuries with multiple current pathways or those in which the victim falls from a high pole. Sometimes arcing occurs and results in concurrent flame burn and clothing fire. Cardiac abnormalities, manifested as ventricular fibrillation or cardiac arrest, are common; patients with high-tension electrical injury need cardiac monitoring until they are stable and have been fully assessed. Higher-risk patients have abnormal electrocardiographic findings and a history of loss of consciousness. Renal damage from deep muscle necrosis and subsequent myoglobinuria is another complication; such patients need forced alkaline diuresis to minimize renal damage. Aggressive removal of all dead and devitalized tissue, even with the risk of functional loss, remains the key to effective management of the electrically damaged extremity. Early debridement facilitates early closure of the wound. Damaged major vessels must be isolated and buried in a viable muscle to prevent exposure. Survival depends on immediate intensive care, whereas a functional result depends on long-term care and delayed reconstructive surgery.
| CLINICAL MANIFESTATIONS | MANAGEMENT | |
|---|---|---|
| General | — | Extricate the patient; perform ABCs of resuscitation; immobilize the spine |
| History: voltage, type of current | ||
| Complete blood count with platelets, electrolytes, blood urea nitrogen (BUN), creatinine, glucose | ||
| Cardiac | Dysrhythmias: asystole, ventricular fibrillation, sinus tachycardia, sinus bradycardia, premature atrial contractions (PACs), premature ventricular contractions (PVCs), conduction defects, atrial fibrillation, ST-T wave changes |
Modified from Hall ML, Sills RM: Electrical and lightning injuries. In Barkin RM, editor: Pediatric emergency medicine, St Louis, 1997, Mosby, p 484.
Lightning burns occur when a high-voltage current directly strikes a person (most dangerous) or when the current strikes the ground or an adjacent (in-contact) object. A step voltage burn is observed when lightning strikes the ground and travels up one leg and down the other (the path of least resistance). Lightning burns depend on the current path, the type of clothing worn, the presence of metal, and cutaneous moisture. Entry, exit, and path lesions are possible; the prognosis is poorest for lesions of the head or legs. Internal organ injury along the path is common and does not relate to the severity of the cutaneous burn. Linear burns, usually 1st- or 2nd-degree, are in the locations where sweat is present. Feathering or an arborescent pattern is characteristic of lightning injury. Lightning may ignite clothing or produce serious cutaneous burns from heated metal in the clothing. Internal complications of lightning burns include cardiac arrest caused by asystole, transient hypertension, premature ventricular contractions, ventricular fibrillation, and myocardial ischemia. Most severe cardiac complications resolve if the patient is supported with cardiopulmonary resuscitation (Chapter 62). CNS complications include cerebral edema, hemorrhage, seizures, mood changes, depression, and paralysis of the lower extremities. Rhabdomyolysis and myoglobinuria (with possible renal failure) also occur.
Ali SN, O’Toole G, Tyler M. Milk bottle burns. J Burn Care Rehabil. 2004;25:461-462.
Arnoldo B, Purdue GF, Kowalske K, et al. Electrical injuries: a 20-year review. J Burn Care Rehabil. 2004;25:479-484.
Bracco D, Eggimann P. Prophylaxis with systemic antibiotics in patients with severe burns. BMJ. 2010;340:487-488.
Chen EH, Sareen A. Do children require ECG evaluation and inpatient telemetry after household electrical exposures? Ann Emerg Med. 2007;49:64-67.
Collier ML, Ward RS, Saffle JR, et al. Home treadmill friction injuries: a five-year review. J Burn Care Rehabil. 2004;25:441-444.
Enoch S, Roshan A, Shah M. Emergency and early management of burns and scalds. BMJ. 2009;338:937-941.
Garrel D. Burn scars: a new cause of vitamin D deficiency. Lancet. 2004;363:259-260.
Hart DW, Wolf SE, Ramzy PI, et al. Anabolic effects of oxandrolone after severe burn. Ann Surg. 2001;233:556-564.
Herndon DN, Hart DW, Wolf SE, et al. Reversal of catabolism by beta-blockade after severe burns. N Engl J Med. 2001;345:1223-1229.
Herndon DN, Tompkins RG. Support of the metabolic response to burn injury. Lancet. 2004;363:1895-1902.
Hohlfeld J, de Buys Roessingh A, Hiti-Burri N, et al. Tissue engineered fetal skin constructs for paediatric burns. Lancet. 2006;366:840-842.
Juurlink DN, Buckley NA, Stanbrook MB, et al: Hyperbaric oxygen for carbon monoxide poisoning, Cochrane Database Syst Rev (1):CD002041, 2005.
Kai-Yang L, Zhao-Fan X, Luo-Man Z, et al. Epidemiology of pediatric burns requiring hospitalization in China: a literature review of retrospective studies. Pediatrics. 2008;122:132-142.
Lowell G, Quinlan K, Gottleib LJ. Preventing unintentional scald burns: moving beyond tap water. Pediatrics. 2008;122:799-804.
Musgrave MA, Fingland R, Gomez M, et al. The use of inhaled nitric oxide as adjuvant therapy in patients with burn injuries and respiratory failure. J Burn Care Rehabil. 2000;21:551-557.
Orgill DP. Excision and skin grading of thermal burns. N Engl J Med. 2009;360:893-900.
Sanghavi P, Bhalla K, Das V. Fire-related deaths in India in 2001: a retrospective analysis of data. Lancet. 2009;373:1282-1288.
Sheridan RL. Thermal injuries. In: McInerny TK, Adam HM, Campbell DE, editors. American Academy of Pediatrics pediatric textbook of pediatric care. Elk Grove Village, IL: American Academy of Pediatrics, 2008.
Sheridan RL, Hinson M, Liang MH, et al. Long-term outcomes of children surviving massive burns. JAMA. 2000;283:69-73.
Singer AJ, Dagum AB. Current management of acute cutaneous wounds. N Engl J Med. 2008;359:1037-1046.
Stoddard FJ, Usher CT, Abrams AJ. Psychopharmacology in pediatric critical care. Child Adolesc Psychiatr Clin North Am. 2006;15:611-655.
Wiechman SA, Patterson DR. Psychosocial aspects of burn injuries. BMJ. 2004;329:391-393.
Volinsky J, Hanson J, Lustig J. Lightning burns. Arch Pediatr Adolesc Med. 1994;148:529-530.
Walker A. Emergency department management of house fire burns and carbon monoxide poisoning in children. Curr Opin Pediatr. 1996;8:239-242.
Wolf SE, Thomas SJ, Dasu MR, et al. Improved net protein balance, lean mass, and gene expression changes with oxandrolone treatment in the severely burned. Ann Surg. 2003;237:801. 10; discussion 810–811
Young AE, Thornton KL. Toxic shock syndrome in burns: diagnosis and management. Arch Dis Child Edu Pract Ed. 2007;92:ep97-ep100.