Chapter 17 Bronchoscopy
1 What is flexible bronchoscopy?
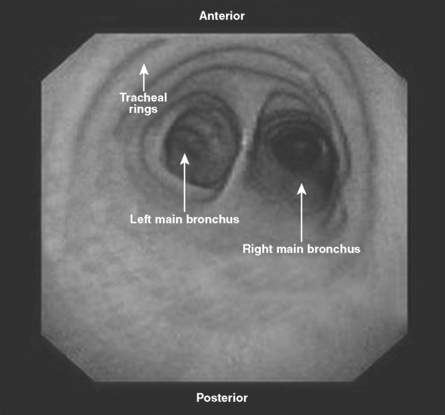
Bronchoscopy literally means “to see the airways.” This procedure allows visualization of the upper airways, trachea, and bronchi. Flexible bronchoscopy uses a small-caliber fiberoptic scope, which is passed through the nose or mouth or through a tracheostomy or endotracheal tube (Fig. 17-1). The bronchoscope is then directed down the trachea to the main carina (Fig. 17-2) and beyond to the regions of interest. In most patients, the airways can be visualized at least to the segmental bronchi.
2 How is flexible bronchoscopy performed?
1. Set up suction equipment and monitoring for cardiac rhythm, blood pressure, and oxygenation saturation. Supplemental oxygen should be provided via nasal cannula or face mask.
2. Numb the patient’s nose and pharynx with topical lidocaine.
3. Control cough and gag with small doses of short-acting narcotic and benzodiazepines.
4. Lubricate the bronchoscope with topical lidocaine jelly. Anesthesia of the posterior pharynx, vocal cords, and carinas is particularly important because advancing the bronchoscope past these areas is most likely to cause the patient to cough.
6 What are the indications for bronchoscopy in the intensive care unit (ICU)?
Bronchoscopy allows inspection of the airways, collection of samples from the lower airways, and performance of various interventions (Table 17-1). In the ICU, it is most commonly used to diagnose infection via bronchoalveolar lavage (BAL) or protected specimen brush. In BAL, the tip of the bronchoscope is wedged into a subsegmental bronchus while aliquots of saline solution (typically 30 mL each) are injected and aspirated into sterile traps. Alveolar contents are collected while the bronchoscope position prevents flooding of other regions of the lung. The protected specimen brush is a sterile brush with a gelatin cap that is inserted into a potentially infected area, agitated, then withdrawn and sent for culture.
| Step | Indication | Goal |
|---|---|---|
| Inspection | Hemoptysis | Localize bleeding |
| Search for endobronchial lesion | ||
| Infection | Identify evidence of inflammation or pus | |
| Aspiration | Look for foreign bodies | |
| Mass | Look for endobronchial masses | |
| Chest trauma | Find evidence of airway injury | |
| Inhalational injury | Find evidence of airway injury | |
| Sample collection | Pulmonary infiltrates (infectious) | Obtain samples for Gram stain, silver stain, bacterial cultures, and viral and fungal studies |
| Pulmonary infiltrates (noninfectious) | Identify alveolar hemorrhage | |
| Check for eosinophilia (analyze cell count and differential) | ||
| Mass or adenopathy | Perform transbronchial biopsy for cytologic or pathologic analysis | |
| Interventions | Hemoptysis | Control bleeding |
| Bronchial obstruction | Remove mucus or foreign bodies | |
| Perform laser removal of masses | ||
| Place stent | ||
| Alveolar proteinosis | Perform lavage | |
| Intubation | Visualize anatomy for tube placement |
7 What other kinds of samples can be collected by bronchoscopy?
 Cytology brush: An abrasive brush is agitated against potentially malignant tissue and then sent for cytologic analysis.
Cytology brush: An abrasive brush is agitated against potentially malignant tissue and then sent for cytologic analysis.
 Transbronchial biopsy: The bronchoscope is advanced into subsegmental bronchi; then biopsy forceps are pushed past distal airways into the pulmonary parenchyma to obtain lung tissue. This technique may be used to diagnose infection (i.e., fungal disease), granulomatous diseases (i.e., sarcoidosis), or malignancy.
Transbronchial biopsy: The bronchoscope is advanced into subsegmental bronchi; then biopsy forceps are pushed past distal airways into the pulmonary parenchyma to obtain lung tissue. This technique may be used to diagnose infection (i.e., fungal disease), granulomatous diseases (i.e., sarcoidosis), or malignancy.
 Transbronchial needle aspiration: A technique used in diagnosis and staging of cancer. A short, rigid needle is thrust through the airway wall, usually near the main carina, into subcarinal or paratracheal lymph nodes. Suction is then applied to aspirate cells, which are sent for cytologic evaluation.
Transbronchial needle aspiration: A technique used in diagnosis and staging of cancer. A short, rigid needle is thrust through the airway wall, usually near the main carina, into subcarinal or paratracheal lymph nodes. Suction is then applied to aspirate cells, which are sent for cytologic evaluation.
9 List the absolute and relative contraindications for bronchoscopy
 Absolute contraindications: These include an inability to maintain a patent airway during the procedure, such as in upper airway obstruction, laryngospasm, or intubation with a small endotracheal tube; an inability to oxygenate or ventilate adequately during bronchoscopy; active cardiac ischemia; malignant arrhythmias; and severe hemodynamic instability.
Absolute contraindications: These include an inability to maintain a patent airway during the procedure, such as in upper airway obstruction, laryngospasm, or intubation with a small endotracheal tube; an inability to oxygenate or ventilate adequately during bronchoscopy; active cardiac ischemia; malignant arrhythmias; and severe hemodynamic instability.
 Relative contraindications: These include poor patient cooperation, elevated intracranial pressure, and severe coagulopathy. Patients with impending respiratory failure or laryngeal edema may undergo bronchoscopy more safely if the airway is secured by elective endotracheal intubation before the procedure.
Relative contraindications: These include poor patient cooperation, elevated intracranial pressure, and severe coagulopathy. Patients with impending respiratory failure or laryngeal edema may undergo bronchoscopy more safely if the airway is secured by elective endotracheal intubation before the procedure.
10 What are the potential complications of bronchoscopy?
Flexible bronchoscopy is generally a safe procedure. However, complications do occur, with an incidence in observational studies of 0.1% for death and 2% to 5% for major complications (Table 17-2). Sources of complication include the bronchoscopic procedure itself and anesthetic or sedative medications.
| Intervention | Potential Complication | Prevention |
|---|---|---|
| Passing bronchoscope through nose | Epistaxis, nasal discomfort | Topical anesthesia and vasoconstriction |
| Passing bronchoscope through pharynx | Gagging, emesis, aspiration | Topical anesthesia, benzodiazepines |
| Passing bronchoscope into trachea | Laryngospasm, cough, laryngeal trauma | Topical anesthesia |
| Bronchospasm | Pretreatment with beta agonists | |
| Bronchoalveolar lavage | Postprocedure fever | Minimize lung contamination by oral secretions |
| Hypoxemia | Supplemental oxygen; good wedge technique | |
| Cytology brush | Endobronchial hemorrhage | Avoid vascular lesions |
| Transbronchial biopsy | Hemorrhage | Avoid vascular lesions |
| Pneumothorax | Avoid distal biopsies; consider fluoroscopy | |
| Topical lidocaine administration | Arrhythmias, seizures | Use < 7 mg/kg (< 25 mL) of 2% lidocaine |
| Conscious sedation | Hypotension | Intravenous access, prehydration in patients with hypovolemia |
| Respiratory depression | Avoid oversedation, stimulate patient |
20 How is bronchoscopy used in performing tracheostomy in the ICU?
Key Points Bronchoscopy
1. Complications of bronchoscopy may occur because of topical anesthesia, sedation, or the procedure itself and include hypoxia, pneumothorax, and hypotension.
2. Bronchoscopy samples can be obtained via BAL, protected brush specimen, cytology brush, or biopsy.
3. Flexible bronchoscopy is most commonly used in the ICU to diagnose and guide antibiotic choices for VAP.
4. Chest physiotherapy appears to be as effective as bronchoscopy in treating atelectasis, although bronchoscopy has a role in retained, inspissated secretions or foreign bodies.
5. Bronchoscopy can be safely performed in patients with mechanical ventilation, including those with acute respiratory distress syndrome.
1 Annema J.T., van Meerbeeck J.P., Rintoul R.C., et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA. 2010;304:2245–2252.
2 Fagon J.Y. Diagnosis and treatment of ventilator-associated pneumonia: fiberoptic bronchoscopy with bronchoalveolar lavage is essential. Semin Respir Crit Care Med. 2006;27:34–44.
3 Kreiker M.E., Lipson D.A. Bronchoscopy for atelectasis in the ICU. A case report and review of the literature. Chest. 2003;124:344–350.
4 Oberwalder M., Weis H., Nehoda H., et al. Videobronchoscopic guidance makes percutaneous dilational tracheostomy safer. Surg Endosc. 2004;18:839–842.
5 Shorr A.F., Susla G.M., O’Grady N.P. Pulmonary infiltrates in the non-HIV-infected immunocompromised patient: etiologies, diagnostic strategies, and outcomes. Chest. 2004;125:260–271.
6 Steinberg K.P., Mitchell D.R., Maunder R.J., et al. Safety of bronchoalveolar lavage in patients with adult respiratory distress syndrome. Am Rev Respir Dis. 1993;148:556–561.
7 Wahidi M.M., Rocha A.T., Hollingsworth J.W., et al. Contraindications and safety of transbronchial lung biopsy via flexible bronchoscopy. A survey of pulmonologists and review of the literature. Respiration. 2005;72:285–295.
8 Wang K.P., Mehta A.C. Flexible Bronchoscopy, 2nd ed. Oxford, United Kingdom: Blackwell Science, 2004.