Chapter 381 Bronchomalacia and Tracheomalacia
Chondromalacias of the trachea or of a main bronchus occur when there is insufficient cartilage to maintain airway patency throughout the respiratory cycle and are common causes of persistent wheezing in infancy. Tracheomalacia and bronchomalacia can be either primary or secondary (see Table 381-1 on the Nelson Textbook of Pediatrics website at www.expertconsult.com). Although primary tracheomalacia and bronchomalacia are often seen in premature infants, most affected patients are born at term. Secondary tracheomalacia and bronchomalacia refers to the situation in which the central airway is compressed by adjacent structure (e.g., vascular ring, Chapter 426) or deficient in cartilage due to tracheoesophageal fistula. Laryngomalacia can accompany primary bronchomalacia or tracheomalacia. Involvement of the entire central airway (laryngotracheobronchomalacia) is also seen.
Table 381-1 CLASSIFICATION OF TRACHEOMALACIA
PRIMARY TRACHEOMALACIA
SECONDARY TRACHEOMALACIA
From McNamara VM, Crabbe DC: Tracheomalacia, Paediatr Respir Rev 5:147–154, 2004.
Diagnosis
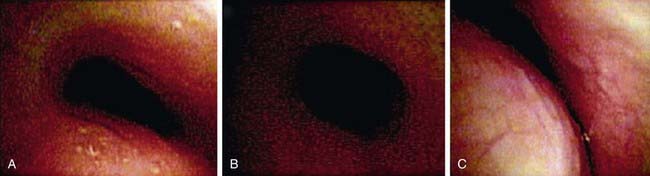
The definitive diagnoses of tracheomalacia and bronchomalacia are established by flexible or rigid bronchoscopy (Fig. 381-1). The lesion is difficult to detect on plain radiographs, but fluoroscopy can demonstrate dynamic collapse and can avoid the need for invasive diagnostic techniques. Pulmonary function testing can show a pattern of decreased peak flow and flattening of the flow-volume loop. Other important diagnostic modalities include MRI and CT scanning. MRI with angiography is especially useful when there is a possibility of vascular ring and should be performed when a right aortic arch is seen on plain film radiography.
Anton-Pacheco JL, Cabezali D, Tejedor R, et al. The role of airway stenting in pediatric tracheobronchial obstruction. Eur J Cardiothorac Surg. 2008;33:1069-1075.
Boogaard R, Huijsmans SH, Pijnenburg MW, et al. Tracheomalacia and bronchomalacia in children: incidence and patient characteristics. Chest. 2005;128:3391-3397.
Carden KA, Boiselle PM, Waltz DA, et al. Tracheomalacia and tracheobronchomalacia in children and adults: an in-depth review. Chest. 2005;127:984-1005.
Masters IB, Chang AB, Patterson L, et al. Series of laryngomalacia, tracheomalacia, and bronchomalacia disorders and their associations with other conditions in children. Pediatr Pulmonol. 2002;34:189-195.
Masters IB, Zimmerman PV, Pandeya N, et al. Quantified tracheobronchomalacia disorders and their clinical profiles in children. Chest. 2008;133:461-467.
McNamara VM, Crabbe DC. Tracheomalacia. Paediatr Respir Rev. 2004;5:147-154.
Yalcin E, Dogru D, Ozcelik U, et al. Tracheomalacia and bronchomalacia in 34 children: clinical and radiologic profiles and associations with other diseases. Clin Pediatr. 2005;44:777-781.