CHAPTER 19 Bridge Plating of Distal Radius Fractures
Distal radius fractures represent one sixth of all fractures seen and treated in emergency departments.1 The treatment goals for the management of these fractures include restoring congruity to the radiocarpal and distal radioulnar joint (DRUJ) surfaces and maintaining radial length. Currently, there are a number of established surgical options for displaced distal radius fractures as well as newer novel approaches being developed for the surgical management of these injuries.2–13 The choice of surgical technique for reduction and fixation will depend on fracture displacement, joint surface involvement, patient age, bone quality, handedness, occupation, and avocation. Recent advances in the biological and biomechanical understanding of wrist fractures have prompted a more aggressive approach to the fixation of the distal radius. As surgical treatment in general, and plating in particular, ensures more consistent correction of displacement and maintenance of reduction, there has been an increasing trend for operative treatment of these fractures in both the elderly and the young populations. In no area of fracture management has there been such a recent explosion of new treatment modalities as there has been in distal radius fixation.
Two subsets of patients with distal radius fractures continue to represent unique treatment challenges: (1) patients with high-energy wrist injuries with fracture extension into the radial diaphysis and (2) patients with multiple injuries that require load bearing through the injured wrist to assist with mobilization and nursing care. There exist few publications specifically addressing the management of distal radius injuries in the multiply injured patient and/or the problem of distal radius fractures with diaphyseal extension.14,15 High-energy fractures of the distal aspect of the radius with extensive comminution of the articular surface and extension into the diaphysis represent a major treatment challenge. Standard plates and techniques may be inadequate for the management of such fractures.
Patients with multiple injuries, especially those with injuries to the pelvis and lower extremities, require use of the upper extremities for transfers and weight bearing. There exists no evidence that the newer fixation techniques can support such activities. Although it is possible that augmentation of distal radius fixation with a spanning external fixator could improve weight bearing through the upper extremity, this has not been clinically proved. However, it is known that external fixation of fractures presents a set of problems that can be particularly vexing for patients being cared for in intensive care units. These include the burden of pin care and an increased incidence of pin tract contamination and infection.16,17 The ideal fixation device in this setting would assist with and maintain reduction, require no nursing care, and allow the use of the extremity for mobilization.
The use of internal distraction plating or bridge plating for distal radius fractures was first introduced by Burke and Singer.18 The technique was further expanded by Ruch and coworkers, who described the use of a 12- to 16-hole 3.5-mm dynamic compression plate (DCP) (Synthes, Paoli, PA) placed in the floor of the fourth dorsal extensor compartment to span from the intact radius diaphysis to the third metacarpal.14,19 The bridge plating technique provides strong fixation and allows for distraction across impacted articular segments. The technique can be combined with a limited articular fixation approach for those fracture patterns with intra-articular extension. Recently, bridge plating of the distal radius was further refined by Hanel and colleagues.15 The authors described a variant of the bridge plating technique using 2.4-mm AO plates passed extra-articularly through the second dorsal compartment and secured onto the dorsal radial aspect of the radius diaphysis and the second metacarpal. They reviewed the senior author’s experience with bridge plating in a series spanning a 10-year period at a level 1 trauma center. The patients earlier in the series were treated using a 22-hole 2.4-mm titanium mandibular reconstruction plate (Synthes, Paoli, PA) and later in the series with a 2.4-mm stainless steel plate specifically designed for use as a distal radius bridge plate (DRB plate) (Synthes, Paoli, PA). The mandibular reconstruction plate is made of titanium and has square ends and scalloped edges and threaded holes to accept locking screws. The DRB plate that we presently continue to use is made of stainless steel, has tapered ends to facilitate sliding the plate within the extensor compartment, and also has locking screws. The described bridge plating technique is technically easy and achieves the goals of maintenance of fracture reduction, allows weight bearing through the injured extremity, and is associated with few complications (Table 19-1).
TABLE 19-1 Indications for Bridge Plating of Distal Radius Fractures
| Indication | Explanation |
|---|---|
| Metadiaphyseal comminution of the radius | Extensive comminution in metadiaphyseal region is difficult to treat with standard implants used for distal radius fractures. |
| Need for weight bearing through the upper extremity | Patients with associated lower limb injuries may require the need for early weight bearing through the upper extremities. |
| Polytrauma | Nursing care of the multiply injured patient may be easier with spanning internal fixation than with external fixation. |
| Augmented fixation | In osteoporotic bone, bridge plating can be used to augment tenuous fixation. |
| Carpal instability | Carpal instability, particularly radiocarpal, isolated, or in combination with a distal radius fracture, may be held in a reduced position with the help of spanning internal fixation. |
Technique and Surgical Approach
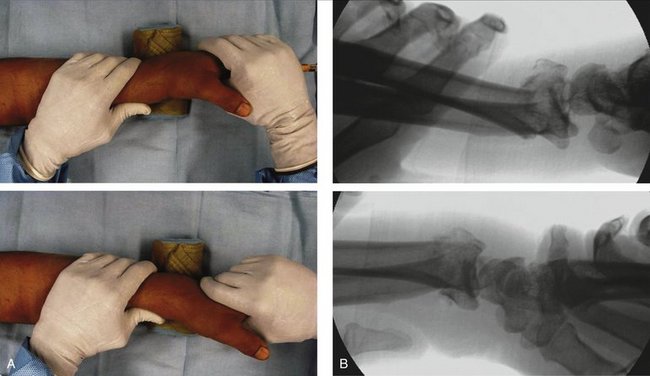
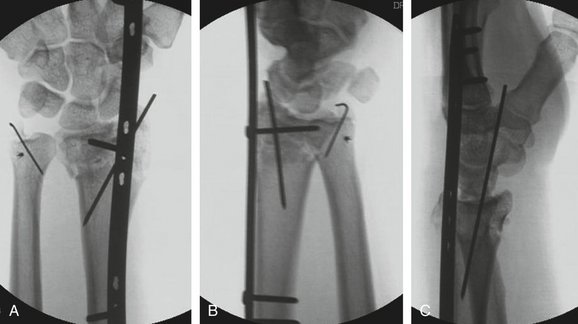
With the patient anesthetized and supine on the operating table, the involved extremity is draped free and centered on a radiolucent hand table. Finger traps are applied to the index and middle fingers, and 4.5 kg of longitudinal traction is applied through a rope and pulley system. Under image intensification, the closed reduction maneuver described by Agee is performed20 (Fig. 19-1). Longitudinal traction is first used to restore length and to assess the benefit of ligamentotaxis for the restoration of articular step-off (Fig. 19-2). Next, the hand is translated palmarly relative to the forearm to restore sagittal tilt and to assess the integrity of the volar lip of the radius (Fig. 19-3). Finally, pronation of the hand relative to the forearm is performed to correct the supination deformity. Once the initial reduction maneuver is completed, the bridge plate is then applied.
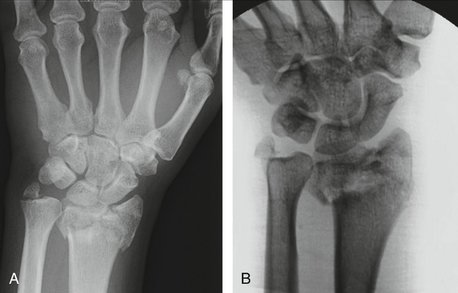
FIGURE 19-2 Anteroposterior radiographs of the wrist. A, Injury film. B, After distraction is applied.
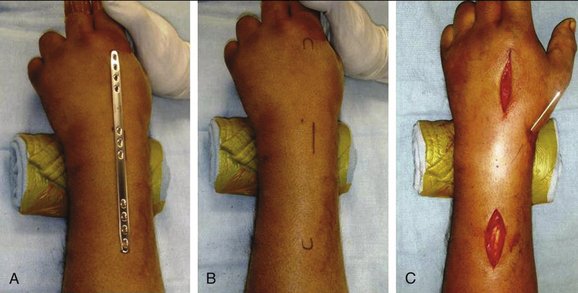
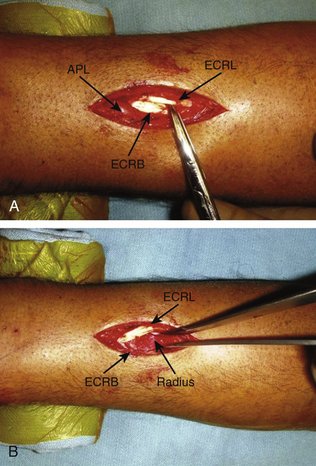
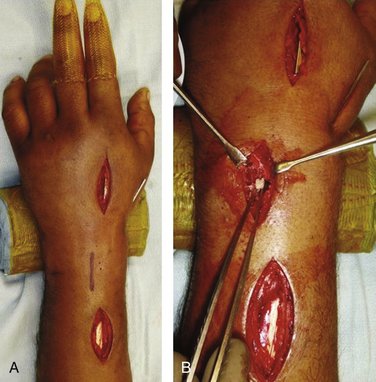
The DRB plate is superimposed on the skin from the radial diaphysis to the distal metadiaphysis of the second metacarpal. The position of the plate is verified with image intensification, and markings are placed on the skin at the level of the proximal and distal four screw holes of the plate (Fig. 19-4). The subcutaneous tissues are infiltrated with 0.25% bupivacaine with epinephrine to promote hemostasis. A 5-cm incision is made at the base of the second metacarpal and continued along the second metacarpal shaft. In the depths of this incision, the insertions of the extensor carpi radialis longus (ECRL) and the extensor carpi radialis brevis (ECRB) are identified as they pass beneath the distal edge of the second dorsal wrist compartment to insert on the second and third metacarpal bases, respectively. A second incision is made just proximal to the outcropper muscle bellies (abductor pollicis longus [APL]) and the extensor pollicis brevis (EPB), in line with the ECRL and ECRB tendons. The interval between the ECRL and ECRB is developed, and the diaphysis of the radius is exposed (Fig. 19-5). The DRB plate is introduced beneath the muscle bellies of the outcroppers extraperiosteally and advanced distally between the ECRL and ECRB tendons (Fig. 19-6). Some resistance may be encountered as the plate emerges distally, but this can usually be easily overcome with gentle manipulation of the plate. Occasionally, the plate will not pass through the compartment. In these cases, a guidewire or stout suture retriever is passed along the compartment from distal to proximal. The plate is secured to the distal end of the wire and delivered into the hand. In the rare instance that these measures fail, a third incision is made directly over the metaphysis of the radius, the proximal one half of the second compartment is incised, and the plate is passed under direct vision. The third, or periarticular, incision may also be used to assess the articular surface, reduce die-punch fragments, and introduce bone graft (Fig. 19-7).
After passing the bridge plate, it is then secured to the second metacarpal by placing a nonlocking fully threaded 2.4-mm cortical screw through the most distal plate hole. The proximal end of the plate is then identified in the forearm. If the radial length has not been restored, then the plate, secured to the second metacarpal, is pushed distally until the length is reestablished and a fully threaded 2.4-mm nonlocking screw is placed in the most proximal plate hole. By using nonlocking screws the plate is effectively lagged onto the intact bone. Plate alignment along the longitudinal axis of the radius is guaranteed by securing the most distal and most proximal screw holes first. The remaining holes are secured with fully threaded locking screws inserted with bicortical purchase (Fig. 19-8).
It has been our experience that as the plate is passed along the radial diaphysis, through the second compartment and along the second metacarpal, extra-articular alignment, radial inclination, volar tilt, and radial length are restored. Intra-articular reduction may be further adjusted by using limited periarticular incisions to allow for direct manipulation of articular fragments, placement of subchondral bone grafts, repair of intercarpal ligament injuries, and augmentation of fracture fixation with Kirschner wires (K-wires) and periarticular plates. Displaced volar medial fracture fragments that are not reduced with this technique require a separate volar incision and appropriate buttress support.
Postoperative Rehabilitation
Digit range of motion exercises start within 24 hours of surgery. Load bearing through the forearm and elbow is allowed immediately, as well as the use of a platform crutch when the patient is physiologically stable. At 1 month postoperatively the platform is removed and weight bearing is allowed through the hand grip of regular crutches. Lifting and carrying is restricted to approximately 4.5 kg until the fracture has healed.
Results
The bridge plating technique for distal radius fractures was reviewed in a retrospective study consisting of 62 consecutive patients treated in this fashion and representing 10-year experience with the technique at a level 1 trauma center.15 Patients managed with bridge plating either for distal radius fractures with extensive metadiaphyseal comminution or patients with distal radius fractures associated with other injuries requiring weight bearing through the affected extremity represented 13% of distal radius fractures requiring operative fixation during this time period. Fracture healing occurred in all 62 patients. In each case radial length was within 5 mm of ulnar-neutral variance, radial inclination was more than 5 degrees, and palmar tilt was at least neutral. There were also no articular gaps or step-offs greater than 2 mm, and the DRUJ was stable in all cases. Similarly, Ruch and coworkers showed 14 of 22 patients obtained excellent radiographic and functional results and another 6 of 22 patients obtained good results in their prospective cohort of patients with comparable pathological processes.14
The plate was removed on average 112 days after placement. One outlying patient had the bridge plate in place upwards of 19 months because he did not wish to take time off work to have the plate removed. The plate in this case eventually failed at 16 months, but the patient continued to work until the broken hardware became increasingly prominent and symptomatic. Finally, at the time of plate removal the patient sustained an ECRL rupture that was treated with ECRL-to-ECRB tenodesis. There were no other documented complications in the series. In addition, there were no cases of excessive postoperative finger stiffness of reflex sympathetic dystrophy. This reflects the overall infrequent complications reported in the literature for bridge plating of the distal radius. In fact, Burke and Singer18 reported no complications and Ruch and associates14 reported no hardware failures and only 3 patients who developed long finger extensor lag of 10 to 15 degrees.
Overall, these results compare favorably with the findings of Burke and Singer18 and Ruch and associates.14 The bridge plates were removed at a mean of 110 days in the Ruch cohort versus 112 days in the senior author’s series. Ruch and associates14 reported 35 degrees of flexion, 45 degrees of extension, 69 degrees of pronation, and 72 degrees of supination at 6 months with a mean grip strength of 41% of the contralateral side. At 1 year, flexion and extension averaged 57 and 65 degrees, respectively; pronation and supination averaged 77 and 76 degrees, respectively; and grip strength improved to 69% of the contralateral side. DASH scores in their study decreased from 33.8 points at 6 months, to 15.4 points at 1 year, and 11.5 points at the time of final follow-up at an average of 24.8 months. Using the rating system of Gartland and Werley21 at 1 year postoperatively, 63.6% of results were graded as excellent, 27.2% were graded as good, and 9.0% as fair. The authors of each of these studies proposed that distraction plating allows fracture reduction and fixation over a broad metadiaphyseal area while effectively diverting compression forces away from the fracture site.
Discussion
Before the introduction of this technique, treatment of these injuries was limited to cast immobilization or external fixation with or without K-wire augmentation. Both of these methods are associated with unacceptably high complication rates. Lafontaine and coworkers showed that the end results of comminuted distal radius fractures treated by closed methods resembled the prereduction radiographs more than any other radiographs during treatment even when the reduction successfully restored wrist anatomy.22 Szabo and Weber reported a greater than 50% complication rate when using external fixation alone, with the most frequent complications being pin tract infections.23 This latter complication becomes an even more frequent occurrence in the patients confined to intensive care units.
The biomechanical stability of spanning plates is strong and predictable. Behrens and Johnson, studying the rigidity of external fixator configurations, demonstrated that rigidity is directly proportional to how close the longitudinal fixator bar is to the bone and the fracture.24 A bridge plate, resting directly against the radius proximally and metacarpals distally, therefore, optimizes the conditions to obtain the strongest possible fixator construct. A DRB plate fixed with a minimum of three screws at either end of the plate confers significantly more stability than would an external fixator used to stabilize a comparable fracture.25
With prolonged immobilization and distraction there may be concerns that wrist stiffness will result and fracture nonunion will occur.14,15 However, in the senior author’s series, there were no nonunions and a functional range of motion was attained within a year of plate removal in all cases.15
The technique described here varies from that described by Burke and Singer.18 The bridge plate used in this description is smaller, using 2.4-mm screws instead of 3.5-mm screws, and is converted to a fixed-angle device by the use of locking screws. The plate is placed in the second dorsal compartment rather than the fourth and secured to the second metacarpal rather than the third metacarpal. Becton and colleagues first suggested this position while presenting a fixation plate specific to the task.26 However, we do not use the implant Becton and colleagues suggested because it is too short for most of the fractures we encounter and cannot be converted to a fixed-angle device. However, similar to Becton and colleagues, we note that the dorsal radial aspect of the radial diaphysis, the floor of the second extensor compartment, and the dorsal radial aspect of the second metacarpal are collinear. Passing a fixation plate along these surfaces through the intact retinaculum of the second dorsal compartment while applying longitudinal traction effectively restores radial length, radial inclination, and volar tilt of the radial styloid and scaphoid facet. Depression fractures of the lunate facet and volar shearing fractures, especially those involving the critical volar ulnar corner of the radius, may require separate manipulation and fixation. Burke and Singer18 cite a significant intra-articular component of the fracture as the major advantage to a fourth dorsal compartment approach in these injuries. However, we use indirect reduction techniques, percutaneous wires, limited dorsal incisions, and open reduction of volar shearing fractures as needed to address the articular component of the fractures and maintain reductions.
Conclusion
The use of bridge plating in the treatment of distal radius fractures avoids the complications of external fixation. A bridge plate can remain implanted for extended periods of time, without deleterious effects on functional outcome. All patients in our series went on to heal with acceptable metadiaphyseal and intra-articular alignment. In patients with multiple traumatic injuries, bridge plating allowed earlier postoperative load bearing across the affected wrist. This enabled independent transfers and the use of ambulatory aids. Application of bridge plates is simple, and surgical time is comparable with the application of an external fixator.
1. Graff S, Jupiter J. Fracture of the distal radius: classification of treatment and indications for external fixation. Injury.. 1994;25:S-D14-S-D25.
2. Drobetz H, Bryant AL, Pokorny T, et al. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction—a biomechanic study in a cadaveric model. J Hand Surg [Am]. 2006;31:615-622.
3. Gradl G, Jupiter JB, Gierer P, Mittlmeier T. Fractures of the distal radius treated with a nonbridging external fixation technique using multiplanar K-wires. J Hand Surg [Am]. 2005;30:960-968.
4. Handoll HH, Madhok R: Surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003; CD003209.
5. Hastings H2nd, Leibovic SJ. Indications and techniques of open reduction, internal fixation of distal radius fractures. Orthop Clin North Am. 1993;24:309-326.
6. Kamath AF, Zurakowski D, Day CS. Low-profile dorsal plating for dorsally angulated distal radius fractures: an outcomes study. J Hand Surg. 2006;31:1061-1067.
7. Konrath GA, Bahler S. Open reduction and internal fixation of unstable distal radius fractures: results using the Trimed fixation system. J Orthop Trauma. 2002;16:578-585.
8. McQueen MM. Non-spanning external fixation of the distal radius. Hand Clin. 2005;21:375-380.
9. McQueen MM, Simpson D, Court-Brown CM. Use of the Hoffman 2 compact external fixator in the treatment of redisplaced unstable distal radial fractures. J Orthop Trauma. 1999;13:501-505.
10. Orbay JL, Touhami A. Current concepts in volar fixed-angle fixation of unstable distal radius fractures. Clin Orthop Relat Res. 2006;445:58-67.
11. Rikli DA, Regazzoni P. The double plating technique for distal radius fractures. Tech Hand Up Extrem Surg. 2000;4:107-114.
12. Schnall SB, Kim BJ, Abramo A, Kopylov P. Fixation of distal radius fractures using a fragment-specific system. Clin Orthop Relat Res. 2006;445:51-57.
13. Tornetta P3rd, Klein DM, Stein AB, McQueen M. Distal radius fracture. J Orthop Trauma. 2002;16:608-611.
14. Ruch DS, Ginn TA, Yang CC, et al. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87:945-954.
15. Hanel DP, Lu TS, Weil WM. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445:91-99.
16. Ahlborg HG, Josefsson PO. Pin-tract complications in external fixation of fractures of the distal radius. Acta Orthop Scand. 1999;70:116-118.
17. Parameswaran AD, Roberts CS, Seligson D, Voor M. Pin tract infection with contemporary external fixation: how much of a problem. J Orthop Trauma. 2003;17:503-507.
18. Burke EF, Singer RM. Treatment of communited distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2:248-252.
19. Ginn TA, Ruch DS, Yang CC, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution: surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1):29-36.
20. Agee JM. Distal radius fractures: multiplanar ligamentotaxis. Hand Clin. 1993;9:577-585.
21. Gartland JJJr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33:895-907.
22. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208-210.
23. Szabo RM, Weber SC. Comminuted intraarticular fractures of the distal radius. Clin Orthop Relat Res. 1988;230:39-48.
24. Behrens F, Johnson W. Unilateral external fixation: methods to increase and reduce frame stiffness. Clin Orthop Relat Res. 1989;241:48-56.
25. Wolf JC, Weil WM, Hanel DP, Trumble TE. A biomechanic comparison of an internal radiocarpal-spanning 2.4-mm locking plate and external fixation in a model of distal radius fractures. J Hand Surg [Am]. 2006;31:1578-1586.
26. Becton JL, Colborn GL, Goodrich JA. Use of an internal fixator device to treat comminuted fractures of the distal radius: report of a technique. Am J Orthop. 1998;27:619-623.