127 Breast Disorders
• There are very few true breast emergencies, and immediately life-threatening causes such as traumatic breast rupture or necrotizing fasciitis are exceedingly rare.
• Breast pain, particularly if cyclic, is common, and benign causes predominate.
• Breast cancer is a possible diagnosis in any patient with a chief complaint related to the breast, including breast pain or a mass, nipple discharge, or skin lesions.
• Most patients in whom breast cancer is diagnosed have no risk factors except age older than 50 years and female sex, and eight of nine patients have no family history of breast cancer.
• The emergency physician can play a role in reduction of the risk for lymphedema by early and aggressive treatment of even very minor infections and burns.
• Most medications are safe for use while breastfeeding, and the benefits of continuing breastfeeding generally outweigh the potential for harm.
• Few maternal infections, other than human immunodeficiency virus, present a significant risk to the breastfeeding infant.
Acknowledgment and thanks to Dr. Karen Jubanyik for her contribution to the first edition.
Epidemiology
Approximately one half of visits to physicians for breast complaints are for pain. New, palpable masses represent another common breast-related complaint. Although a benign condition will be diagnosed in 9 of 10 premenopausal women with a palpable breast mass, a new mass in a 75-year-old woman is malignant up to 70% of the time. Breast cancer is the most common cause of cancer-related mortality in women worldwide and second only to lung cancer in women in the United States. In 2006, it accounted for one third of all cancer diagnoses in women in the United States.1
Although there are few true breast-related emergencies, perioperative issues represent a second significant group of emergency department (ED) visits. Breast surgery is relatively common in the United States. In addition to the 90,000 mastectomies performed annually, approximately 100,000 cosmetic augmentations and 100,000 reduction mammoplasties take place each year.2 Many patients undergoing breast augmentation, either for reconstruction or cosmesis, experience significant complications and require additional surgery.
Pathophysiology
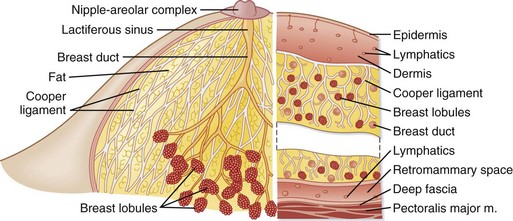
The unique anatomic structure of the breast contributes to the wide variety of pathologic conditions that may occur. Each breast contains approximately 20 glandular units (lobes) composed of glands and adipose tissue (Fig. 127.1). Each lobe drains into a lactiferous duct, which fuses with other ducts to form lactiferous sinuses just below the skin. The lactiferous sinuses store milk during lactation. Disruption (obstruction, infection, inflammation) of the glandular system may occur at any time during a female’s lifetime but predominates between menarche and menopause. The breast’s diffuse vascular network predisposes it to hematogenous spread of malignancy, as well as infection.
Differential Diagnosis and Medical Decision Making
See Box 127.1 for an overview of causes of breast-related complaints.
Mastalgia
Noncyclic mastalgia may be caused by a variety of conditions3 (Box 127.2). It may be constant or intermittent, but it is not associated with the menstrual cycle. Noncyclic mastalgia tends to be unilateral and localized to a discrete area. Women with noncyclic breast pain are generally older than 40 years, and the cause is likely to be related to an anatomic lesion in the breast. It is rare for breast cancer to have pain as the sole initial symptom.4
Mondor disease (Fig. 127.2) is a superficial phlebitis of the lateral thoracic, thoracoepigastric, or superior epigastric vein. It typically occurs in middle-aged women. The condition can be unilateral or bilateral. It is often idiopathic but may be associated with other conditions.5 The classic Mondor cord is 2 to 3 mm in diameter and typically red and tender, tracks from the lateral margin of the breast across the costal margin, and extends from 2 to 30 cm. Any tenderness should resolve within weeks, but the cord may remain palpable for up to 6 months. There is no risk for systemic embolization.
Dermatologic Changes and Discharge
A wide variety of skin conditions can affect the breast, nipple, or both; the most threatening and most common are listed in Box 127.3 and are discussed in the following sections.
Nonpuerperal Mastitis and Abscess
Periductal mastitis may be confused with cellulitis, abscesses, or inflammatory breast cancer. Approximately 90% of nonpuerperal breast abscesses are subareolar.6
Mammary Paget Disease
Paget disease of the nipple (Fig. 127.3, A and B), first described by James Paget in 1874, is a neoplastic condition that accounts for 2% to 4% of breast malignancies. The lesion involves the nipple-areola complex and may spread to the surrounding skin. Patients with early disease may have only a burning and itching sensation around the nipple area. A central palpable breast mass is present in 60% of cases.7 Patients with mammary Paget disease usually undergo mastectomy with either lymph node dissection or sentinal node biopsy.
Skin Necrosis
Warfarin-induced skin necrosis is a rare complication of oral anticoagulant therapy that affects only 0.01% to 0.1% of patients who take the medication.8 The typical patient is a middle-aged, obese woman who recently initiated Coumadin therapy, although cases have been reported occurring well into a year of therapy.
The lesions can be single or multiple and are accompanied by intense pain.
Masses
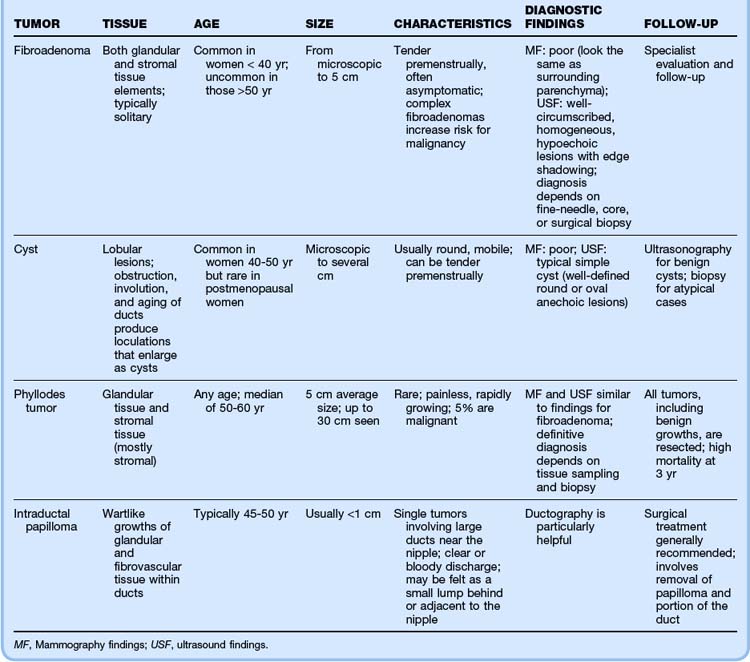
Breast cancer is exceedingly rare in women younger than 20 years and accounts for only a small fraction of a percent of breast disease in women younger than 30 years. Most women younger than 35 years with a solitary painless breast mass will have a fibroadenoma (see Table 127.1 for a comparison of benign breast tumors). Common benign breast masses include fibroadenomas, cysts, phyllodes tumors (malignant 5% of the time), and intraductal papillomas. Other benign tumors found in breast tissue, but not limited to the breasts, include lipomas, hamartomas, hemangiomas, neurofibromas, granular cell tumors, and fat necrosis. None of these conditions appear to increase the risk for subsequent development of breast cancer.
Breast Cancer
Emergency physicians (EPs) are in a unique position to provide education about breast cancer and screening (Box 127.4) to many women who do not have other contact with the health care system,9–11 in particular, minority and lower socioeconomic groups, who have both higher mortality rates and decreased access to preventive services. A female born in the United States today has a 13% probability of breast cancer developing during her lifetime. Most women in whom breast cancer develops have only two risk factors (being female and age older than 50 years).
Box 127.4
American Cancer Society Recommendations for Breast Cancer Screening, 2010
Women 40 years and older should have a screening mammogram every year and should continue to do so for as long as they are in good health.
Breast self-examination (BSE) is an option for women starting in their 20s. Women should be told about the benefits and limitations of BSE. Women should report any changes in their breasts to their health professional right away.
Women in their 20s and 30s should have a clinical breast examination (CBE) as part of a periodic (regular) health examination by a health professional at least every 3 years. After 40 years of age, women should undergo CBE by a health professional every year.
Women at high risk (greater than 20% lifetime risk) should undergo magnetic resonance imaging (MRI) and mammography every year. Women at moderately increased risk (15% to 20% lifetime risk) should talk with their doctors about the benefits and limitations of adding MRI screening to their yearly mammogram. Yearly MRI screening is not recommended for women whose lifetime risk for breast cancer is less than 15%.
From American Cancer Society guidelines for breast cancer screening. Available at www.cancer.org. Revised 2/9/11.
Complications of Breast Cancer
Most patients who are treated for breast cancer undergo surgery that includes some degree of lymph node dissection. Lymphedema affects 10% to 30% of women who undergo axillary lymph node dissection; radiation and infection increase the risk. Lymphedema may range from mild to severe and can develop even years after treatment. Those at risk for the development of lymphedema are encouraged to have blood drawn and intravenous lines placed in the unaffected arm. It is usually permanent, although a few institutions have reported success with autologous lymph node transplantation.12
Women who choose lumpectomy or partial mastectomy usually undergo 6 weeks of external beam radiation therapy. Radiotherapy may also be given in the form of radioactive seeds placed at the tumor site. In another method, a saline-filled balloon is placed in the lumpectomy site and radioactive material is instilled and drained twice daily for 5 days. Regardless of the radiation method, the most common complications are radiation-induced dermatitis13 (90% of patients), which can progress to dry desquamation (50% of patients) in the first few weeks, and moist desquamation (<10% of patients), which appears within 3 to 6 weeks. A corticosteroid cream such as mometasone furoate can be used as prophylaxis or treatment of dry desquamation, preferably in consultation with a medical or radiation oncologist. Wet desquamation, a partial-thickness injury, is best treated with hydrocolloid dressings and should be managed in consultation with a plastic surgeon or radiation oncologist.
Late effects of radiation may develop months or years after therapy. Pneumonitis is typically manifested as cough, fever, and shortness of breath 1 to 10 months after completion of radiation therapy. Radiographic changes, which can start as diffuse haziness and progress to patchy consolidations, are generally confined to the field of radiation. Dermal necrosis is a complication that may develop years after treatment. Radiation-induced brachial plexopathy,14 which may develop up to 30 years after breast cancer therapy, is a permanent debilitating condition that can progress to complete sensory and motor impairment of the ipsilateral upper extremity and chronic neuropathic pain.
Fat Necrosis
The most common long-term complication after trauma to the breast is fat necrosis.15 Fat necrosis is an inflammatory condition that is typically a sequela of trauma, but it may also develop following surgery, infection, or radiation therapy. Women with pendulous breasts seem to be at higher risk for fat necrosis. The pathophysiology is multifactorial but primarily involves the breakdown of fat cells by blood and tissue lipases. Clinically, mammographically, and sonographically, the condition may mimic carcinoma of the breast. Usually, a firm, poorly mobile, nontender mass is present in the superficial subcutaneous tissues. The overlying skin may be erythematous, ecchymotic, or indurated. Axillary lymphadenopathy and nipple retraction may be present. Fat necrosis typically resolves spontaneously but requires biopsy to reliably differentiate it from malignancy.
Perioperative Complaints
More than 2 million women in the United States have undergone breast augmentation. Although 80% of augmentations are performed purely for cosmetic reasons, the 20% representing reconstruction following mastectomy account for a disproportionate percentage of local complications. Roughly 30% will require additional surgeries within 5 years.16
Postoperative pain can be prolonged; 30% to 40% of patients report significant pain 1 year after reduction or augmentation mammoplasty, and the number is higher after mastectomy with reconstruction. Phantom breast pain after mastectomy occurs in up to 12% of patients 1 year after surgery.17
Lactation and Puerperal Changes
Puerperal Mastitis
Puerperal mastitis, or mastitis that develops while breastfeeding, is a common cause of premature cessation of lactation and results in voluntary discontinuation of breastfeeding in up to 25% of patients.18 It develops in about one third of nursing mothers. Eighty percent of cases occur in the first 3 months of lactation. Mastitis can rarely progress to abscess formation; this is significantly more common in the first 6 weeks after birth. Risk factors for puerperal mastitis include older age, primiparity, nipple damage, employment outside the home, ineffective nursing technique, and milk stasis.
Risks Associated with Lactation in Special Circumstances
Breastfeeding is superior to manufactured infant formula for its nutritional, cognitive, emotional, and immunologic benefits. Not all medications contraindicated during pregnancy are similarly dangerous to the nursing infant. Inappropriate cross-referencing of drug information in pregnancy to lactation may result in early cessation of lactation. Similarly, not all maternal infections necessitate cessation of lactation19 (Table 127.2).
Table 127.2 Breastfeeding Recommendations with Selected Maternal Infections
| INFECTION | CLINICAL SIGNIFICANCE AND IMPACT ON BREASTFEEDING |
|---|---|
| CMV | Rarely causes illness in full-term infants because of placentally acquired antibodies |
| Hepatitis A | Found in breast milk but is an unusual mode of transmission; give immunoglobulin to the infant and continue breastfeeding |
| Hepatitis B | Give the infant routine hepatitis B vaccine and immunoglobulin and continue breastfeeding |
| Hepatitis C | Not proved to be transmitted by breastfeeding; continue breastfeeding. |
| VZV | Close contact with a person with acute VZV infection requires VZV immunoglobulin; the infant must avoid an infected person until the lesions crust over; expressed breast milk may be given unless lesions are present on the nipple-areola complex |
| HSV-1 and HSV-2 | Breastfeeding can be continued unless lesions are present on the breast |
| Lyme disease | If organism can be detected in breast milk by PCR but the infant has no signs of clinical illness, continue breastfeeding |
| Syphilis | Delay breastfeeding and express breast milk until maternal therapy has been given for 24 hr; treat the infant empirically |
| TB | Transmission via breast milk is seen only with TB mastitis; if no breast lesions are present, stop breastfeeding for 14 days and give isoniazid to the infant; expressed breast milk may be used |
| Gonorrhea | If the mother is treated with ceftriaxone, continue breastfeeding; if other medications are used, delay breastfeeding for 24 hr |
CMV, Cytomegalovirus; HSV, herpes simplex virus; PCR, polymerase chain reaction; TB, tuberculosis; VZV, varicella-zoster virus.
Data from Lawrence RM, Lawrence RA. Breast milk and infection. Clin Perinatol 2004;31:501–28.
On average, 1% to 2% of a maternal dose of a drug is delivered to the infant, although the amount varies depending on the drug. Because the milk compartment is bidirectional, a drug that peaks in milk after 30 minutes may leave the milk compartment before the next feeding. It is therefore recommended that when possible, a nursing mother take medications immediately after a feeding to decrease the amount delivered to the infant in the next feeding. Little evidence-based data are available to determine which drugs are safe to use in lactation. EPs concerned about the safety of a particular medication in a lactating woman can consult the American Academy of Pediatrics Committee on Drugs.20
Administration of radioactive compounds to a lactating mother may require temporary cessation of breastfeeding (Table 127.3). Expression and discarding of milk for the duration of five half-lives are recommended. When ordering a nuclear medicine study for a lactating woman, the EP should speak directly to the nuclear medicine radiologist to determine whether a radionuclide with a shorter half-life could be used.
Table 127.3 Radioactive Drugs That Require Temporary Cessation of Breastfeeding
| DRUG | TIME OF CESSATION |
|---|---|
| Gallium 67 | 14 days |
| Iodine 125 | 12 days |
| Iodine 131 | 2-14 days, depending on the study |
| Radioactive sodium | 4 days |
| Copper 64 | 50 hr |
| Technetium 99m | 15-36 hr |
| Iodine 123 | 36 hr |
| Indium 111 | 20 hr |
Data from American Academy of Pediatrics Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108:776–89.
Treatment
Mastalgia
Most patients require only mild analgesics, such as acetaminophen or ibuprofen. Discomfort from Mondor disease can also be managed with warm compresses. A number of alternative potential treatment modalities are available to women with cyclic mastalgia21 (Box 127.5). Women with severe cyclic mastalgia, despite treatment with conservative measures, should be referred to an endocrinologist or reproductive specialist. All patients with mastalgia should receive follow-up care.
Box 127.5 Adjuvant Treatment of Cyclic Mastalgia
Improvement in mechanical support with a properly fitting bra and use of a sports bra during exercise
Application of warm compresses or ice packs
Decreasing dietary fat to less than 20% of energy intake
Eliminating caffeine in the diet
Oral contraceptive pills with low estrogen content
Parenteral medroxyprogesterone acetate (Depo-Provera)
Puerperal Mastitis
![]() Patient Teaching Tips
Patient Teaching Tips
Any new breast symptom requires evaluation by a physician; the patient should seek prompt reevaluation if initial treatment of a diagnosed condition is not effective.
Although most causes of breast lumps, skin changes, breast pain, and nipple discharge are benign, many conditions (including malignancy) appear similar on physical examination and even on imaging studies.
Making a definitive diagnosis of any breast condition may require several follow-up outpatient visits and tests.
Patients should be familiar with the American Cancer Society’s recommendations for breast cancer screening for their age group.
Most patients fail to appreciate the significance of the false-negative rate of mammography. Mammograms fail to diagnose breast cancer in up to 15% of cases; therefore, a recent “normal” screening mammogram should not falsely reassure a patient with a suspicious complaint. Tissue sampling is indicated in these situations.
Patients who have undergone surgery or radiation therapy (or both) for breast cancer are at high risk for the development of lymphedema. They should be instructed to avoid compression of the ipsilateral arm and should seek immediate medical care for the treatment of insect bites, burns, lacerations, and infections, all of which increase the risk for lymphedema.
![]() Documentation
Documentation
Meticulous documentation of the physical examination, as well as all results, when evaluating a patient with a complaint related to the breast or when an abnormality is discovered incidentally is a necessity.
Documentation of the physical examination should include the appearance of the breasts, including the nipple-areola complex, with the patient sitting, with the arms raised, and supine. Results of palpating the breast with the patient supine and the ipsilateral hand under the head should be recorded, as well as the results of gentle nipple squeezing.
All abnormalities should be diagrammed and described. Size, mobility, consistency, and symmetry in comparison with the opposite breast are important to document. Lymph nodes should be noted in terms of number, size, consistency, and mobility.
Impeccable documentation is required in cases of suspected intimate partner violence or sexual assault.
When treating a lactating patient, all discussions about the advisability and possible risks associated with continuing breastfeeding should be documented, especially when diagnosing infectious conditions, prescribing medications, and ordering radionuclide imaging.
The history should include attention to current medications, as well as past hormonal therapy, menopausal status, reproductive and breastfeeding history, family history of cancer, radiation exposure, and previous breast problems.
An inclusive differential diagnosis should be documented, specifically listing cancer if it is a possibility. In these cases, documented discussions with the patient should include mention of the physician’s concerns and need for prompt follow-up.
Written discharge instructions should include follow-up plans and phone numbers for referral physicians. Special arrangements may be necessary to ensure timely specialist care. All such efforts should be documented.
Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229–237.
Michie C, Lockie F, Lynn W. The challenge of mastitis. Arch Dis Child. 2003;88:818–821.
Smith RL, Pruthi S, Fitzpatrick L. Evaluation and management of breast pain. Mayo Clin Proc. 2004;79:353–372.
Whitaker-Worth DL, Carlone V, Susser WS, et al. Dermatologic diseases of the breast and nipple. J Am Acad Dermatol. 2000;43:733–751.
1 American Cancer Society. Estimated new cancer cases and deaths by sex for all sites. United States, 2006. American Cancer Society Surveillance Research, 2006.
2 Marotta JS, Widenhouse CW, Habal MB, et al. Silicon gel breast implant failure and frequency of additional surgeries: analysis of 35 studies reporting examination of more than 8000 explants. J Biomed Mater Res. 1999;48:354–364.
3 Santen RJ, Mansel RL. Benign breast disorders. N Engl J Med. 2005;353:275–285.
4 Hartmann LC, Sellers TA, Frost MH, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229–237.
5 Dirschka T, Winter K, Bierhoff E. Mondor’s disease: a rare cause of anterior chest pain. J Am Acad Dermatol. 2003;49:905–906.
6 Versluijs-Ossewaarde FN, Roumen RMH, Goris RJA. Subareolar breast abscesses: characteristics and results of surgical treatment. Breast J. 2005;11:179–182.
7 Lloyd J, Flanagan AM. Mammary and extramammary Paget’s disease. J Clin Pathol. 2000;53:742–749.
8 Whitaker-Worth DL, Carlone V, Susser WS, et al. Dermatologic diseases of the breast and nipple. J Am Acad Dermatol. 2000;43:733–751.
9 American Cancer Society guidelines for breast cancer screening. Available at www.cancer.org Revised 2/9/11
10 Remennick L. The challenge of early breast cancer detection among immigrant and minority women in multicultural societies. Breast J. 2006;12:S103–S110.
11 Euhus DM. Breast cancer prevention in the 21st century: defining the challenge. Breast J. 2006;12:97–98.
12 Becker C, Assouad J, Riquet M, et al. Postmastectomy lymphedema: long-term results following microsurgical lymph node transplantation. Ann Surg. 2006;243:313–315.
13 Harper JL, Franklin LE, Jenretter JM, et al. Skin toxicity during breast irradiation: pathophysiology and management. South Med J. 2004;97:989–993.
14 Schierle C, Winograd JM. Radiation-induced brachial plexopathy: review. Complication without a cure. J Reconstr Microsurg. 2004;20:149–152.
15 Haj M, Loberant N, Salamon V, et al. Membranous fat necrosis of the breast: diagnosis by minimally invasive technique. Breast J. 2004;10:504–508.
16 Gabriel SE, Woods JE, O’Fallon M, et al. Complications leading to surgery after breast implantation. N Engl J Med. 1997;336:677–682.
17 Dijkstra PU, Rietman JS, Geertzen JHB. Phantom breast sensations and phantom breast pain: a 2-year prospective study and a methodological analysis of the literature. Eur J Pain. 2007;11:99–108.
18 Michie C, Lockie F, Lynn W. The challenge of mastitis. Arch Dis Child. 2003;88:818–821.
19 Coutsoudis A. Breastfeeding and HIV. Best Pract Res Clin Obstet Gynaecol. 2005;19:185–196.
20 American Academy of Pediatrics Committee on Drugs. The transfer of drugs and other chemicals into human milk. Pediatrics. 2001;108:776–789.
21 Smith RL, Pruthi S, Fitzpatrick L. Evaluation and management of breast pain. Mayo Clin Proc. 2004;79:353–372.