32 Breast Block
Placement
Anatomy
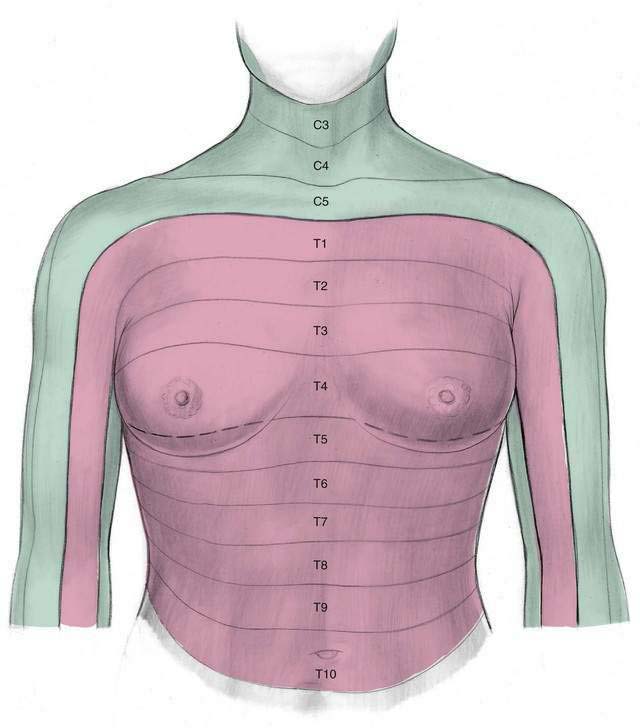
The nerves that must be blocked to carry out the breast block are the second through seventh intercostal (ventral rami for paravertebral) nerves and some terminal branches from the superficial cervical plexus (Fig. 32-1).
Needle Puncture
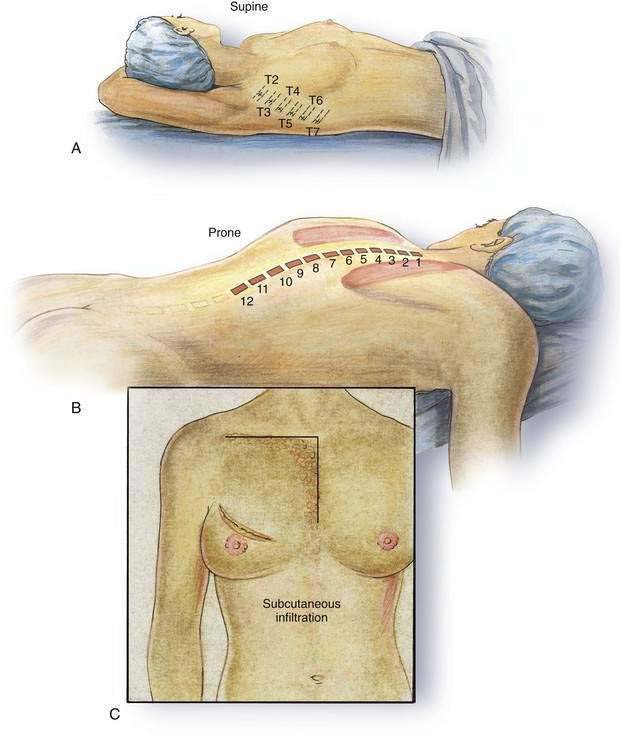
This block can be carried out with the patient in the supine position by performing intercostal nerve block from T2 to T7 in the patient’s mid-axillary line, as shown in Figure 32-2A. Fewer intercostal nerves may be blocked if a limited breast procedure is planned, allowing a more tailored approach. In any event, the patient’s arm should be abducted at the shoulder and placed on an arm board or “tucked under” the head, as shown in Figure 32-2A. The intercostal nerve block can be carried out by using a 22-gauge, short-beveled, 3-cm needle and placing 4 to 5 mL of local anesthetic solution inferior to each rib, after “walking” the needle tip off each rib’s inferior border. If insufficient analgesia is produced, subcutaneous infiltration may have to be added because the lateral cutaneous branches of the intercostal nerve may have been missed. This is possible because the lateral cutaneous nerve may branch more posteriorly in some patients. In addition to the intercostal nerve block, subcutaneous infiltration of local anesthetic must be performed in an “upside-down L” pattern, as shown in Figure 32-2C. This infraclavicular infiltration must be added to interrupt those branches of the superficial cervical plexus that provide sensation to portions of the upper chest wall. Subcutaneous infiltration is also required in the midline to block those intercostal nerve fibers that cross the midline from the contralateral side. Subcutaneous infiltration is facilitated by using a 10- to 12-cm needle.
If a posterior approach to the intercostal nerves (or paravertebral block) is used, the patient must be placed in the prone position and intercostal nerve block carried out by “walking” the needle off, and immediately inferior to, the ribs from T2 through T7 (see Fig. 32-2B). This technique is described in Chapter 33, Intercostal Block. If a paravertebral block is planned, the technique is described in Chapter 37, Paravertebral Block. In any event, if the posterior approach is chosen, the subcutaneous infiltration, as previously outlined, must also be added.
Pearls
Owing to the understandable anxiety that often accompanies breast surgery, patients should understand before undergoing this anesthetic approach that heavy sedation or light general anesthesia (TIVA: total intravenous anesthesia) is most often appropriate in combination with the breast block. Patients who desire to maintain a sense of control during reconstructive or augmentation breast surgery are ideal candidates for a technique in which the loss of control accompanying general anesthesia is avoided. Finally, an emerging trend, thoracic paravertebral blocks (see Chapter 37, Paravertebral Block), are often used effectively in place of the intercostal portion of this nerve block.