Chapter 13 Brain
Methods of imaging the brain
Imaging the brain’s structure and examining its physiology, both in the acute and elective setting, is now the domain of multiplanar, computer-assisted imaging. The imaging modalities in use today include the following:
COMPUTED TOMOGRAPHY OF THE BRAIN
Indications
Technique
Magnetic Resonance Imaging of the Brain
Indications
MRI is indicated in all cases of suspected intracranial pathology. Techniques in use change with the development of new sequences and higher field strength magnets. The techniques described below are, therefore, only basic indications as to sequences in use. The greatest advantages in the use of MRI are the improved contrast resolution between grey and white matter, brain and cerebrospinal fluid (CSF); the removal of artifact due to bone close to the skull base and in the posterior fossa; and in obtaining multiplanar images for lesion localization.
Technique
IMAGING OF INTRACRANIAL HAEMORRHAGE
COMPUTED TOMOGRAPHY
A conventional study consists of 3-mm sections through the brainstem and posterior fossa, and 7-mm sections through the cerebrum. This is the basic multi-detector CT protocol for brain imaging. This is done without contrast to avoid diagnostic difficulty in deciding whether a parenchymal lesion is due to enhancement or blood. Acute blood is typically hyperdense on CT. An exhaustive differential diagnosis for bleeding in different compartments of the brain can be sourced elsewhere but in general bleeding can be extra-axial (i.e. epidural, subdural, subarachnoid, intraventricular) or intra-axial. Intra-axial bleeding can be due to head trauma, ruptured aneurysms or arteriovenous malformations, bleeding tumours (either primary disease or secondaries), hypertensive haemorrhages (cortical or striatal) or haemorrhagic transformation of venous or arterial infarcts. In the assessment of subarachnoid haemorrhage and ischaemic stroke CTA is becoming increasingly used as the screening modality for deciding further intervention. Neurosurgeons are increasingly using CTA alone as the modality for planning microsurgical clipping, especially in the cases where a haematoma exerting mass effect needs to be evacuated immediately adjacent to a freshly ruptured intracranial aneurysm. In ischaemic stroke CTA can localize an acute embolus and CT perfusion imaging can demonstrate the ischaemic core (irreversibly damaged brain) by calculating the relative cerebral blood volume and the ischaemic penumbra (recoverable brain parenchyma) by evaluating the relative cerebral blood flow (rCBF).
Wada R., Aviv R.I., Fox A.J., et al. CT angiography ‘spot sign’ predicts hematoma expansion in acute intracerebral hemorrhage. Stroke. 2007;38(4):1257-1262.
Westerlaan H.E., Gravendeel J., Fiore D., et al. Multislice CT angiography in the selection of patients with ruptured intracranial aneurysms suitable for clipping or coiling. Neuroradiology. 2007;49(12):997-1007.
Imaging of Gliomas
This is an all-encompassing term for a diverse group of primary brain tumours. This includes astrocytomas, oligodendrogliomas, choroid plexus tumours and ependymomas amongst others. The most commonly presenting tumour, however, is the WHO Grade IV astrocytoma or glioblastoma multiforme. Other brain tumours are derived from neuronal cell lines, mixed glial-neuronal cell lines, the pineal gland and embryonal cell lines, peripheral cranial nerves (such as the vestibular schwannoma), meningeal tumours and lymphoma. Appropriate differential diagnoses can be derived from noting the age of the patient, the tumour location (i.e. supra- or infratentorial, cortex or white matter, basal ganglia or brainstem, intra- or extra-axial), its consistency (i.e. cyst formation, mural nodule) and its enhancement characteristics.
Al-Okaili R.N., Krejza J., Wang S., et al. Advanced MR imaging techniques in the diagnosis of intra-axial brain tumors in adults. RadioGraphics. 2006;26:S173-S189.
Stadlbauer A., Gruber S., Nimsky C., et al. reoperative grading of gliomas by using metabolite quantification with high-spatial-resolution proton MR spectroscopic imaging. Radiology. 2006;238:958-969.
Radionuclide Imaging of the Brain
There are currently two main modalities: regional cerebral blood flow imaging and PET imaging. Thallium imaging is also used in specialist centres for brain tumour assessment and there are niche agents in clinical practice used, for example in the diagnosis of Parkinson’s disease. Conventional radionuclide brain scanning (blood–brain barrier imaging) is essentially never used in modern clinical practice.
Conventional Radionuclide Brain Scanning (Blood–Brain Barrier Imaging)
REGIONAL CEREBRAL BLOOD FLOW IMAGING
Radiopharmaceuticals
The most commonly used agent, HMPAO is a lipophilic complex that crosses the blood–brain barrier and localizes roughly in proportion to cerebral blood flow. It is rapidly extracted by the brain, reaching a peak of 5–6% of injected activity within a minute or so, with minimal redistribution (about 86% remains in the brain at 24 h).
This localizes rapidly in proportion to cellular metabolism rather than blood flow, and the distribution has some differences to that of HMPAO, which may need to be taken into consideration for clinical diagnosis.1,2 It currently has the advantage of greater stability than HMPAO and can be used for up to 6 h after reconstitution, which is of particular benefit for ictal epilepsy studies where an injection is only given once a seizure occurs.
Additional techniques
1 Asenbaum S., Brücke T., Pirker W., et al. Imaging of cerebral blood flow with technetium-99m-HMPAO and technetium-99m-ECD: a comparison. J. Nucl. Med.. 1998;39(4):613-618.
2 Koyama M., Kawashima R., Ito H., et al. SPECT imaging of normal subjects with technetium-99m-HMPAO and technetium-99m-ECD. J. Nucl. Med.. 1997;38(4):587-592.
Positron Emission Tomography
Technique
201THALLIUM BRAIN SCANNING
ULTRASOUND OF THE INFANT BRAIN
Indications
Any suspected intracranial pathology, particularly suspected germinal matrix haemorrhage, extra-axial haematomas and hydrocephalus.
Equipment
4–7-MHz, sector transducer. A 7.5- or 10-MHz transducer to visualize superficial structures.
Methods
Technique
Coronal
CEREBRAL ANGIOGRAPHY
Preparation
When the patient is able to understand what is proposed, a clear explanation should be given, together with presentation of the risks and benefits. Most patients do not require sedation for diagnostic procedures and this would be contraindicated in acute neurological presentations. Children, patients who are excessively anxious, those who cannot cooperate because of confusion, or those who would be managed better during the procedure with full ventilation control are examined under general anaesthesia. Neurointerventional studies are done under general anaesthesia. Groin shaving is now regarded as unnecessary. Patients should not be starved unless general anaesthesia is to be used, but should, nevertheless, be restricted to fluid intake and only a light meal.
Technique
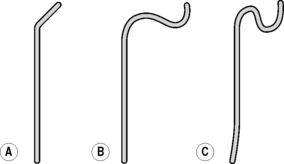
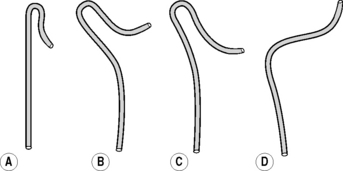
Catheter flushing solutions should consist of heparinized saline (2500 IU l−1 normal saline). Using standard percutaneous catheter introduction techniques, the femoral artery is catheterized. There is a wide range of catheters available and there are proponents of many types. In patients up to middle age without major hypertension, there will be little difficulty with any standard catheter and a simple 4F polythene catheter with a slightly curved tip or 45 ° bend will suffice in the majority. Older patients and those with atherosclerotic disease may need catheters offering greater torque control such as the JB2 or Simmons (Figs 13.1 & 13.2) as appropriate. Catheter control will be better if passed through an introducer set, and this is also indicated where it is anticipated that catheter exchange may be required. Selective studies of the common carotids and the vertebrals are preferable to super selective studies of the internal and external carotids unless absolutely necessary. The following points should be noted: