58 Bradyarrhythmias
• Look at the patient first and then the heart rhythm. A “slow heart rate” is relative to the patient’s age, clinical condition, and comorbid conditions.
• Determine whether the cause is extrinsic or intrinsic to the conduction system.
• Assess the functionality of the key elements of the conduction system: sinoatrial and atrioventricular nodes and the infranodal conduction system.
• Know the vascular supply of the conduction system to determine the significance of bradyarrhythmias and conduction blocks in the setting of acute myocardial infarction.
• Identify risk for failure of the conduction system and the “backup”; for example, a stable escape rhythm, atropine, or a pacemaker.
Epidemiology
Bradycardia is a frequent finding in clinical practice, and its significance is dependent on the underlying cause and clinical effects. The baseline heart rate in an individual patient is determined predominantly by the balance between the parasympathetic and sympathetic nervous systems, and a “normal” heart rate has been defined arbitrarily as 60 to 100 beats/min at rest. The heart rate will vary depending on age, physical condition, and time of observation. Normal ranges for a healthy asymptomatic individual will vary from 46 to 93 beats/min in men and 51 to 95 beats/min in women during the day to rates as low as 40 beats/min at night.1 The heart rate should fluctuate with respiration, the Valsalva maneuver, and other vagal influences confirming normal autonomic control of the sinus node. Bradycardia is a frequent finding in trained athletes, in whom heart rates lower than 40 beats/min are often observed at rest.2 Bradycardias of clinical significance increase in frequency with age and in the setting of illnesses or medications affecting the heart and its conduction system.
Pathophysiology
Extrinsic Causes
Clues to an extrinsic cause of a bradyarrhythmia are a history of a new cardioactive medication, conditions that activate vagal tone, and extreme electrolyte imbalances, specifically potassium (Table 58.1). The associated rhythms are typically those that are due to dysfunction of the sinus or atrioventricular (AV) node:
| COMMON | UNCOMMON | |
|---|---|---|
| Drugs |
From Ford M. Clinical toxicology. Philadelphia: Saunders; 2001. pp. 23-5.
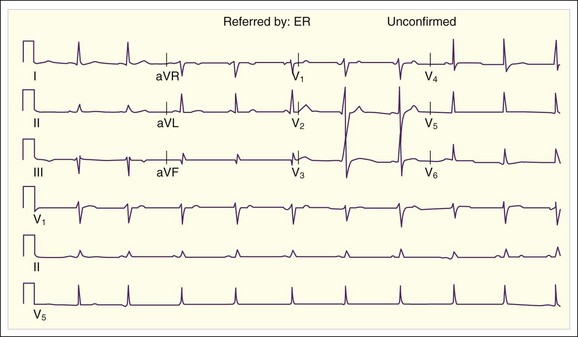
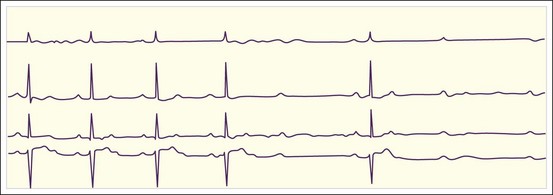
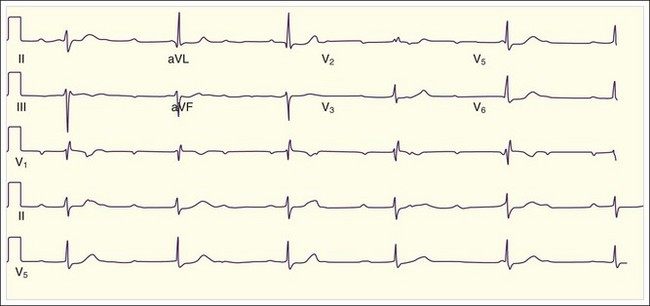
Fig. 58.2 Sinus bradycardia with a ventricular response rate of 59 beats/min.
There is a P wave for every QRS complex and normal PR intervals.
Intrinsic Causes
Certain conditions result in failure of elements of the conduction system because of aging, ischemia or infarction, surgical trauma, or infiltration (Table 58.2). The latter cause encompasses a large group of conditions that include infectious and rheumatologic diseases.3–5 The associated rhythms are typically those that indicate failure of one element of the conduction system rather than failure to generate a rhythm:
| Ischemia and infarction |
MI, Myocardial infarction.
Relative Bradycardia
Relative bradycardia is the presence of a heart rate that is inappropriately slow for the clinical findings. Though often caused by coexisting beta-blocker therapy or age-related blunting of sinus node automaticity, it is also a diagnostic feature of a number of infectious disorders. Relative bradycardia is most useful in differentiating infectious diseases that resemble each other; for example, legionnaires’ disease from Mycoplasma pneumonia and psittacosis or Q fever from tularemia pneumonia.3
Differential Diagnosis and Medical Decision Making
The key to diagnosis and treatment is accurate interpretation of the 12-lead electrocardiogram (ECG). Though not a comprehensive review of all bradycardic rhythms, the following are those commonly encountered.6–8
Second-Degree Heart Block
These heart blocks will be manifested as bradycardia only if the sinus rhythm is slow or a significant percentage of the sinus beats are not conducted.9
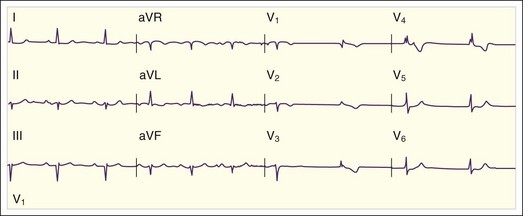
Type I Second-Degree Atrioventricular Block
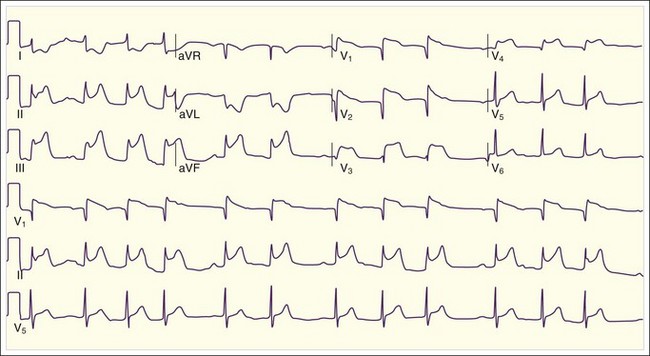
The key ECG feature of a Mobitz type I second-degree AV block (i.e., a Wenckebach block) is progressive lengthening of the PR interval leading to a dropped QRS complex. The PR interval of the first-conducted QRS complex after a nonconducted beat has the shortest or a relatively normal PR interval. These blocks are usually indicative of a medication effect, AV node disease, or ischemia, but the rhythm is rarely the source of the instability10 (Fig. 58.7; also see Fig. 58.4).
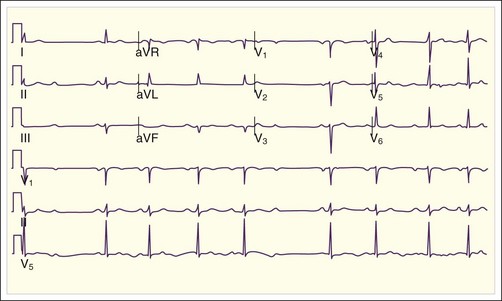
Type II Second-Degree Atrioventricular Conduction Block
Diagnosis of a Mobitz type II heart block is determined by the presence of an intact sinus pacemaker with intermittent failure of conductance to the ventricles. This is due to failure of either the bundle of His or one of the Purkinje fibers. This rhythm is indicative of significant disease of the infranodal conducting system and is likely to progress to a complete heart block. These blocks are often due to myocardial ischemia and are symptomatic (see Fig. 58.5).
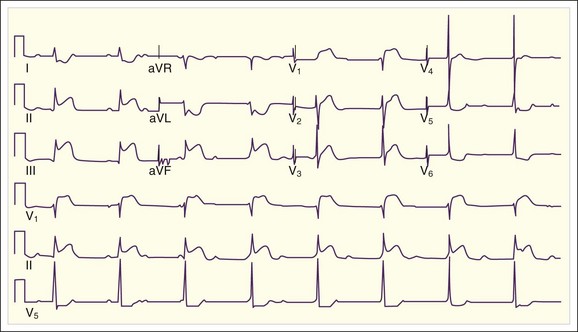
Third-Degree Atrioventricular Block
This rhythm should be considered first in a patient with bradyarrhythmia because it is always clinically significant, often hemodynamically compromising, and unstable (Fig. 58.8; also see Fig. 58.6). The ventricular rate is typically very slow, but the actual rate varies according to the inherent rate of the escape rhythm. In this rhythm there is evidence of independent activity because of no connection between the atria and ventricles. It is important to “march out” the P waves to see if they are regular because some are most likely buried within or are part of the QRS complex or T wave. It should be apparent that there is no fixed relationship between the P waves and the QRS complexes. The QRS complexes can be narrow or wide, depending on the location of the escape pacemaker. Junctional escape pacemakers are faster (50 to 60 beats/min), narrow, and relatively stable in comparison with a ventricular escape rhythm, which is slow (30 to 40 beats/min), wide, and unstable. Often, the most helpful feature of the ECG for this rhythm is that the QRS complexes should be absolutely regular. This is a rhythm initiated by a slower pacemaker exhibiting spontaneous automaticity that has “escaped” the influence of the overriding sinus rhythm. Escape rhythms fire automatically at their inherent rate and are regular. Any irregularity in the escape rhythm suggests a high-grade incomplete AV block or an inherently unstable escape rhythm.
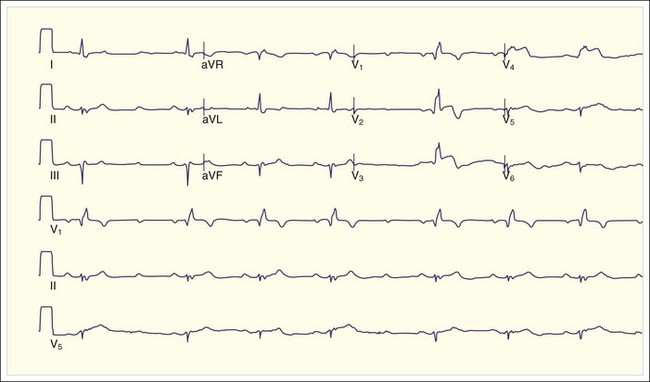
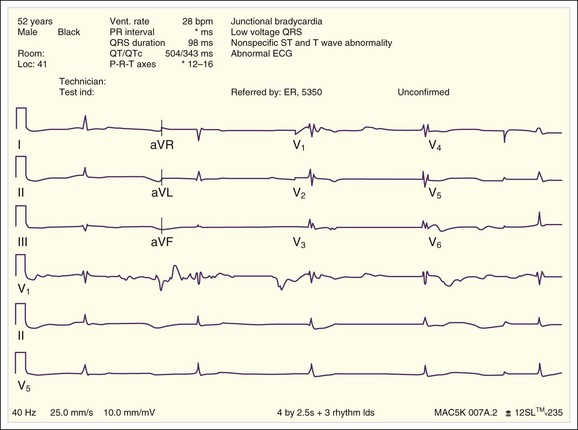
Bradycardia Associated With A Wide QRS Complex
Bradyarrhythmia associated with a “new” widening of the QRS complex suggests a cause that results in diffuse slowing of depolarization and conduction and that usually implicates agents that block the fast sodium channels or their ability to repolarize. This bradycardia is typically seen in patients with poisoning from agents such as tricyclic antidepressants, in patients with hypothermia, or in those with hyperkalemia (Figs. 58.9 and Fig. 58.10).
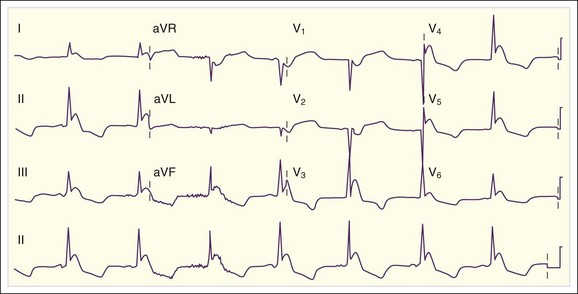
Fig. 58.10 Electrocardiogram showing sinus bradycardia with Osborn waves distorting the QRS complexes.
![]() Facts and Formulas
Facts and Formulas
Sinus bradycardia (adults): Sinus rhythm < 60 beats/min.
Junctional escape rhythm: Ventricular response rate of 40 to 60 beats/min. No P waves. Regular narrow QRS (unless preexisting BBB present).
Idioventricular rhythm: Ventricular response rate of 30 to 45 beats/min. No P waves. Regular wide QRS (usually does not appear as a typical right or left BBB pattern).
Type I second-degree heart block: Sinus rhythm with progressive PR prolongation and a nonconducted beat. The PR interval of the conducted beat following the blocked beat is the shortest interval in the sequence. The QRS complex is usually narrow.
Type II second-degree heart block: Normal sinus rhythm with fixed PR intervals. Random sinus beats are not conducted to the ventricle. The QRS complex is often wide.
Third-degree heart block: Sinus rhythm with P waves visible. The ventricular response rate is regular but slower than the atrial rate with no visible relationship between the P waves and QRS complexes. The QRS rate and width are dependent on the site of the escape rhythm. The junctional escape rate is 40 to 60 beats/min and the QRS complex is narrow. The ventricular escape rhythm is 30 to 45 beats/min and the QRS complex is wide.
![]() Red Flags
Red Flags
Bradycardia is relative. When cardiac stroke volume is normal, perfusion (e.g., blood pressure and cerebral perfusion) can be perfectly adequate even with ventricular response rates in the 30s. When a patient is symptomatic with a bradyarrhythmia, it is often multifactorial in etiology and attention must be paid to optimizing the stroke volume with fluids, reversing the ischemia, or adding inotropic agents in addition to increasing the heart rate.
Bradycardia not associated with hypotension or signs of hypoperfusion may be normal.
Bradycardia not associated with hypotension or signs of hypoperfusion may be an important clue to potentially serious conditions such as elevated intracranial pressure, electrolyte disturbances, or cardiac toxicity from medications.
Bradycardias associated with a wide QSR complex should be reviewed carefully for the presence of a complete heart block or medication or electrolyte effects.
Bradycardia or conduction disturbances in the setting of acute myocardial infarction should be looked for and recognized as a potential clinically significant complication.
Treatment
Prehospital Care
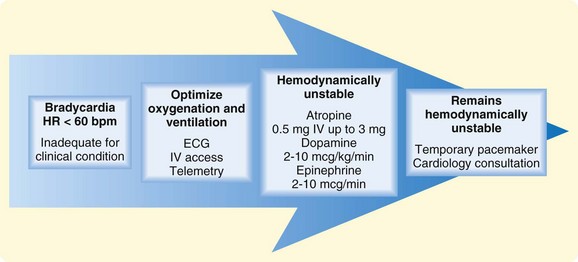
Respiratory disorders and myocardial ischemia are often associated with bradycardia, and prehospital care should focus on optimizing oxygenation, ventilation, and blood pressure and on relieving ischemia if present. Treatment of bradycardia is indicated only for patients who have a bradycardia that is inappropriate for the clinical condition and the patient is symptomatic (Fig. 58.11).
1. Optimize oxygenation (supplemental oxygen) and/or ventilation (continuous positive airway pressure) if needed.
2. Establish intravenous access.
3. Place the patient on telemetry and obtain a 12-lead ECG if possible.
4. If the absolute ventricular response rate is the probable cause of the hemodynamic instability, the following interventions may be helpful:
Hospital Care
1. Optimize oxygenation and ventilation.
2. Establish intravenous access and administer bolus intravenous fluid if the patient is hypotensive without signs of congestive heart failure.
3. Obtain a 12-lead ECG and rhythm strip.
 Sinus bradycardia, type I second-degree heart block, third-degree heart block:
Sinus bradycardia, type I second-degree heart block, third-degree heart block:
 Atropine, 0.5 mg IV up to 3 mg; atropine dosing should be aimed at obtaining the lowest heart rate that will optimize perfusion. In the setting of myocardial ischemia, the clinician must carefully balance the priority of maintaining perfusion to vital organs without exacerbating the myocardial ischemia.
Atropine, 0.5 mg IV up to 3 mg; atropine dosing should be aimed at obtaining the lowest heart rate that will optimize perfusion. In the setting of myocardial ischemia, the clinician must carefully balance the priority of maintaining perfusion to vital organs without exacerbating the myocardial ischemia. Calcium gluconate, 10 mL of a 10% solution IV, may be effective for calcium channel blocker toxicity or hyperkalemia.
Calcium gluconate, 10 mL of a 10% solution IV, may be effective for calcium channel blocker toxicity or hyperkalemia. Type II second-degree heart block, third-degree heart block (particularly with a wide QRS complex):
Type II second-degree heart block, third-degree heart block (particularly with a wide QRS complex):
 Atropine is unlikely to work when the location of the block is in infranodal tissue (e.g., the bundle of His or more distal conduction system) because the blockade is less likely to be reversed with anticholinergic medication. These blocks are preferably treated with temporary pacing or β-adrenergic support as temporizing measures while the patient is being prepared for permanent transvenous pacing.
Atropine is unlikely to work when the location of the block is in infranodal tissue (e.g., the bundle of His or more distal conduction system) because the blockade is less likely to be reversed with anticholinergic medication. These blocks are preferably treated with temporary pacing or β-adrenergic support as temporizing measures while the patient is being prepared for permanent transvenous pacing. Dopamine hydrochloride can be effective in hypotensive, bradycardic patients and can be titrated to more selectively target the heart rate or vasoconstriction. Initial dosing in an unstable patient should start at 2 to 5 mcg/kg/min and be titrated to optimize blood pressure.
Dopamine hydrochloride can be effective in hypotensive, bradycardic patients and can be titrated to more selectively target the heart rate or vasoconstriction. Initial dosing in an unstable patient should start at 2 to 5 mcg/kg/min and be titrated to optimize blood pressure. Epinephrine is a catecholamine with α and β activity and may increase the heart rate and support the blood pressure. The infusion can be initiated at 2 to 10 mcg/min and titrated to patient response. Use of vasoconstrictors requires that the recipient be assessed for adequate intravascular volume and volume status supported as needed.
Epinephrine is a catecholamine with α and β activity and may increase the heart rate and support the blood pressure. The infusion can be initiated at 2 to 10 mcg/min and titrated to patient response. Use of vasoconstrictors requires that the recipient be assessed for adequate intravascular volume and volume status supported as needed.Consultation
Cardiology consultation is recommended for bradyarrhythmias that require pacemaker support and those that are due to failure of the infranodal conduction system or occur in the context of MI. Temporary cardiac pacing (TCP) can be an effective bridge to permanent pacemaker placement. The limited data on the effectiveness of TCP in patients with symptomatic bradycardia show that it is comparable with atropine and dopamine when hospital survival is used as an outcome.11 Its clinical utility is limited by the fact that it is poorly tolerated by awake patients and capture may be unreliable over time. It is reasonable to initiate TCP in unstable patients who do not respond to oxygen, fluids, and pharmacologic interventions as noted earlier. The decision regarding implantation of a pacemaker depends on the underlying cause and the likelihood that the AV block will be permanent. Many conditions affecting the conduction system will predictably resolve, such as electrolyte abnormalities, medication effects, hypothermia, and inferior wall MI, and will require at most TCP. Conversely, pacemaker implantation is indicated, even without hemodynamic instability, for conditions that are likely to progress and place the patient at risk for failure of the conduction system.12,13
MI is associated with significant bradyarrhythmia 25% to 30% of the time.14 The underlying mechanism is either direct ischemic injury to the sinus node, AV node, or conduction system or exaggerated vagally mediated reflexes. The bradyarrhythmias and conduction blocks associated with inferoposterior infarcts are commonly due to vagal reflexes, are responsive to atropine, and are usually transient15,16 (see Figs. 58.7 and 58.8). Sinus bradycardia and AV nodal blockade in the context of an inferior wall MI have been attributed to a higher density of cardiac afferent receptors in the inferoposterior portions of the heart. For hemodynamically compromising bradycardias, atropine is an excellent initial therapy, particularly in the first 6 hours. Doses should be administered in 0.5-mg increments with a maximum dose of 0.04 mg/kg or 3 mg. Doses lower than 0.5 mg should be avoided because of the risk for a paradoxic bradycardic response. When atropine is ineffective, transcutaneous or transvenous pacing is indicated. It is uncommon for type I second-degree and third-degree heart block to be the primary cause of hypotension in a patient with acute MI. Hypotension is usually due to poor stroke volume from the MI, and therapeutic effort should focus on restoring blood flow to the myocardium.
The conduction blocks associated with anterior infarcts typically involve the septum and the bundle branches that run through it. These blocks are not responsive to atropine and generally require permanent pacemaker support. Conduction blocks are typically those that are due to type II second-degree heart block or third-degree heart block. The anterior circulation perfuses the septum containing the His-Purkinje fibers. Ischemia and infarction of the septum may result in failure of one of the fascicles to conduct, usually the right bundle and left anterior fascicle, which lie in the anterior portion of the septum. Fascicular failure alone does not result in bradycardia as long as there is one functioning fascicle in sinus rhythm. Bradycardia may occur with either intermittent failure of the one remaining fascicle to conduct or failure of the bundle of His, which results in a type II second-degree heart block or third-degree heart block. Treatment is placement of a permanent pacemaker.12,13
![]() Priority Actions
Priority Actions
1. Determine whether the patient is hemodynamically compromised by the bradyarrhythmia. If the patient is hypotensive, determine whether it is due to the absolute heart rate or associated conditions that will cause a relative bradycardia to be symptomatic, such as volume loss or left ventricular dysfunction.
2. Establish intravenous access.
3. If it is determined that the absolute ventricular response rate is inappropriate for the clinical condition, the following interventions may be helpful:
4. Indications for temporary transcutaneous pacemaker placement include the following:
Follow-Up, Next Steps in Care, and Patient Education
Admission
![]() Documentation
Documentation
• Determine the clinical significance of the bradycardia. Did the patient pass out or complain of chest pain, exertional fatigue, or dyspnea? Precipitating factors such as nausea, head turning, tight ties, and new medications are important clues to the underlying cause.
• Does the patient have underlying cardiac disease, specifically left ventricular dysfunction, that would contribute to a bradyarrhythmia being symptomatic?
• The medical history should include a detailed medication list and recent dosing history.
• The physical examination may provide clues to the cause of the bradycardia:
• The electrocardiogram and frequently multiple electrocardiograms, particularly when the patient reports symptoms, often specify the diagnosis.
![]() Patient Teaching Tips
Patient Teaching Tips
• Patients with cough, micturition, and bradycardia or syncope should be advised to seek treatment to minimize triggers and to have access to support rails. Patients should lie down when lightheaded and should call 911 for persistent or particularly severe symptoms.
• Patients with carotid sinus hypersensitivity should avoid wearing tight ties and buttoned collars.
• Patients with documented sensitivity to medications that affect the sinus node or the atrioventricular node (or both) should report this fact when being prescribed any new medications.
1 Spodick DH, Raju P, Bishop RL, et al. Operational definition of normal sinus heart rate. Am J Cardiol. 1992;69:1245–1246.
2 Ector H, Bourgois J, Verlinden M, et al. Bradycardia, ventricular pauses, syncope, and sports. Lancet. 1984;2:591–594.
3 Cunha BA. The diagnostic significance of relative bradycardia in infectious disease. Clin Microbiol Infect. 2000;12:633–634.
4 Sondheimer HM, Lorts A. Cardiac involvement in inflammatory disease: systemic lupus erythematosus, rheumatic fever, and Kawasaki disease. Adolesc Med. 2001;12:69–78.
5 Meighem CV, Sabbe M, Knockaert D. The clinical value of the ECG in noncardiac conditions. Chest. 2003;125:1561–1576.
6 DaCosta D, Brady WJ, Edhouse J. ABC of clinical electrocardiography: bradycardias and atrioventricular conduction block. BMJ. 2002;324:535–538.
7 Morrison LJ, Deakin CD, Morley PT, et al. Advanced Life Support Chapter Collaborators. Part 8: advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122(16 Suppl 2):S345–S421.
8 Mangrum MJ, Dimarco J. The evaluation and management of bradycardia. N Engl J Med. 2000;342:703–709.
9 Barold SS, Hayes DL. Second-degree atrioventricular block: a reappraisal. Mayo Clin Proc. 2001;76:44–57.
10 Brady WJ, Harrigan RA. Diagnosis and management of bradycardia and atrioventricular block associated with acute coronary ischemia. Emerg Med Clin North Am. 2001;19:371–383.
11 Barthell E, Troiano P, Olson D, et al. Prehospital external cardiac pacing: a prospective, controlled clinical trial. Ann Emerg Med. 1988;17:1221–1226.
12 Kaushik V, Leon AR, Forrester JS, Jr., et al. Bradyarrhythmias, temporary and permanent pacing. Crit Care Med. 2000;28(Suppl):N121–N128.
13 Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51(21):e1–62.
14 Lamas G, Muller JE, Turi ZG, et al. A simplified method to predict occurrence of complete heart block during acute myocardial infarction. Am J Cardiol. 1986;57:1213–1218.
15 Brady WJ, Swart G, DeBehnke DJ, et al. The efficacy of atropine in the treatment of hemodynamically unstable bradycardia and atrioventricular block: prehospital and emergency department considerations. Resuscitation. 1999;41:47–55.
16 Swart G, Brady WJJ, DeBehnke DJ, et al. Acute myocardial infarction complicated by hemodynamically unstable bradyarrhythmia: prehospital and ED treatment with atropine. Am J Emerg Med. 1999;17:647–652.