CHAPTER 67 Brachioplasty
Physical evaluation
• Evaluate the extent of adiposity and skin excess of the arm, axilla and lateral chest.
• Estimate the degree of upper arm tapered sagging along the posterior margin from the axilla and the elbow towards the most hanging center.
• Search for the inferior dislocation of the posterior axillary fold (PAF). The ptotic PAF broadens the attachment of the arm to the chest, simulating a wing. The loosely suspended PAF contrasts to the tightly adherent deep axillary dome and elongated anterior axillary fold.
• Analyze the enlarged and deep axilla. It may be more than twice normal, which we call hyperaxilla.
• Determine if the anterior axillary fold (AAF) is the flattened and elongated. The descended breast accentuates the AAF deformity.
• Consider the lateral chest skin laxity leading into mid-torso transverse rolls.
• The ideal candidate has ptotic skin that more than doubles the expected width of the upper arm.
• Oversized, obese arms should be identified and treated with liposuction. Brachioplasty may follow.
Technical steps
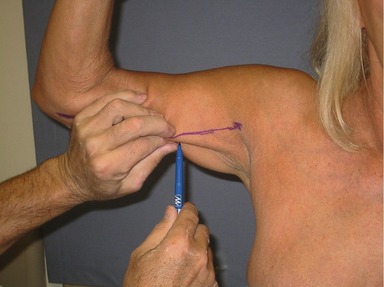
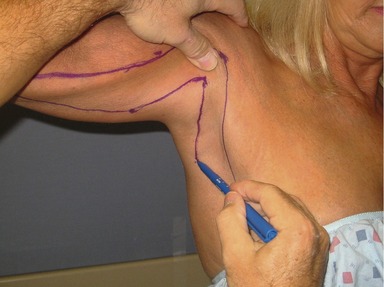
With the patient sitting, the arm and forearm are abducted 90 degrees with the palm forward. Dot the mid-point of the arm slightly posterior to the medial bicipital groove. An anterior line is drawn from the medial elbow through this dot to the deltopectoral groove across the dome of the axilla (Fig. 67.1). By gathering and pinching excess skin and fat posterior to the initial mark, the width of mid-arm excision is determined and a second dot is made near the posterior border (Fig. 67.2). A straight line is drawn from that point to meet the medial elbow termination of the first line (Fig. 67.3). Then by pinching posterior arm skin towards the superior axilla, a critical point is picked and marked along the inferior border of the medial arm that can be advanced to the deltopectoral groove at the proximal termination of the anterior line (Fig. 67.4). Approximation of these points should raise the posterior axillary fold, and equalize the lengths of the anterior and posterior lines. The line then acutely angles to descend inferiorly through the axilla, skirting the posterior axillary fold (Fig. 67.5). A parallel line descends from the deltopectoral groove through the axilla (Fig. 67.6). The distance between these last two lines removes the excess skin of the axilla and lateral chest.
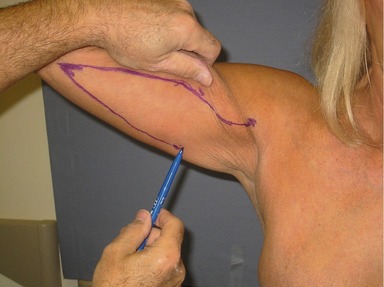
Fig. 67.3 A straight line is drawn from that point to meet the medial elbow termination of the first line.
The operation
With the patient supine, the arms are abducted about 80 degrees on arm boards. Arm intravenous infusion is avoided. The width of resection is rechecked. About 100 mL of saline with 1 mg of epinephrine and 20 mL of 1% xylocaine per liter are infused.
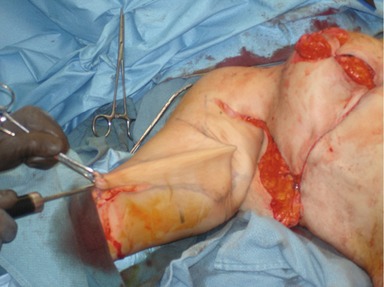
A deep suture advances the PAF triangular flap to the deltopectoral groove. The anterior and posterior arm and chest incisions and are then aligned with towel hooks according to the hatch marks (Fig. 67.7). Only minor adjustments in incision length need be made, and if the excision was inadequate more skin can be removed. A continuous horizontal running 2-0 gauge braided absorbable suture approximates the subcutaneous fascia (Fig. 67.8). A second smaller caliber continuous monofilament intradermal closure follows. Dermal glue completes the operation, and drains are used. The operative time for both arms is approximately 90 minutes. The arms are wrapped in gauze and an ace wrap.
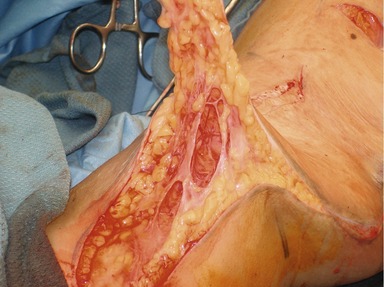
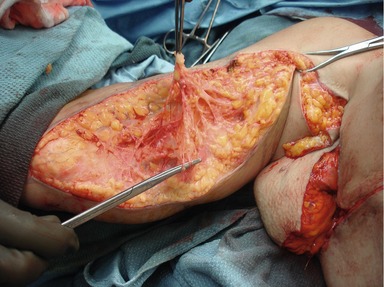
For the last 20 cases, aggressive liposuction by ultrasonic assisted lipoplasty has removed most fat under and preliminary to resection of the arm hemiellipse. The skin is not resected until there is a depression under the pattern and the suction cannula can be visualized subdermal. Limited lipoplasty may be performed elsewhere (Fig. 67.9). Then the medial arm skin is sharply resected like a composite skin graft with adherent web like network of connective tissue and vessels (Fig. 67.10). Bleeding is minimal.
Once the skin is removed the subcutaneous fascial network with accompanying vasculature and sensory nerves are seen (Fig. 67.11). When the liposuction is precise, the retained edge of subcutaneous tissue remains intact for closure.
The next six figures are multiple pre- and postoperative views of a 59-year-old, 5 ft 6 in woman who lost 150 pounds after gastric bypass surgery. Two years previously she had a Wise pattern breast reduction. She had a total body lift (fleur de lys abdominoplasty, lower body lift, medial thighplasty and mons plasty) that included bilateral L brachioplasties (Fig. 67.12). Minor revision surgery around her breasts improved their definition from the chest wall. VASER® Ultrasonic Assisted Lipoplasty was liberally used throughout, with 250 mL removed from each arm with her brachioplasty modified as shown in Figs 67.10–67.12. Her result is seen 10 weeks later, with healing of all skin closures. Her new arm size is harmonious with her body. There is no redundant skin of her arm, axilla and lateral chests, and normal and pleasing contours are seen throughout her arms and torso.
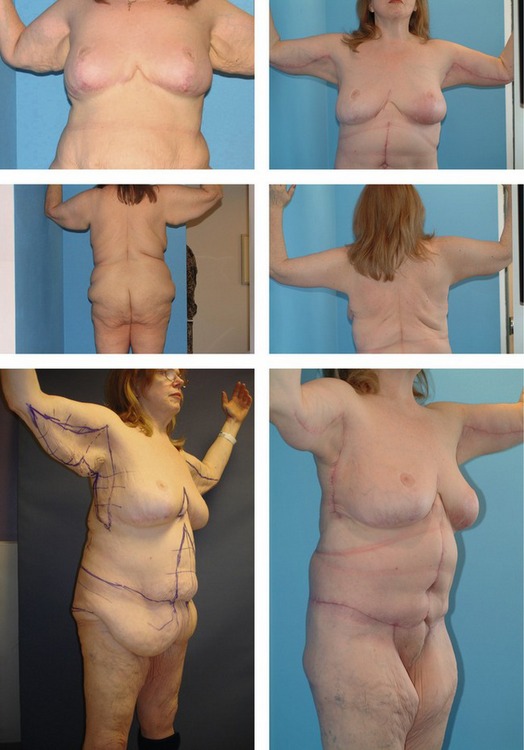
Fig. 67.12 Pre- and postoperative views of a 59-year-old, 5 ft 6 in woman who lost 150 pounds after gastric bypass surgery. The patient had a Wise pattern breast reduction and a total body lift (fleur de lys abdominoplasty, lower body lift, medial thighplasty and mons plasty) that included bilateral L brachioplasties.
Complications
Debridement in the axilla and secondary closure was needed in three patients. Another patient required skin grafting for delayed healing of axillary and hip wounds. Further limited skin reduction after a year was performed in two patients.
Pearls & pitfalls
Pearls
• The ideal candidate has ptotic skin that more than doubles the expected width of the upper arm.
• Oversized, obese arms should be identified and treated with liposuction. Brachioplasty may follow.
• In the authors’ last 20 cases, aggressive liposuction by ultrasonic assisted lipoplasty has removed most fat under and preliminary to resection of the arm hemiellipse.
Pitfalls
• Due to the extensive skin excision in liposuction, there must be a commitment to the breadth of excision based on the preoperative markings. Therefore one should be conservative on the breadth of excision and consider further edgewise excision or avoid radical liposuction. Since radical liposuction reduces damage to the lymphatics, avoiding that step increases the risk of lymphoceles and lymphedema.
• The V advancement flap is vulnerable to tip necrosis, which delays healing and can lead to widened and constricting scars.
• In smaller axillas or if there is delayed healing, the axillary inverted V closure may not sufficiently interrupt the scar, which will result in contracture and restricted arm movement. The secondary Z-plasty inferior to the axilla will solve that problem.
• There is a visible scar which may widen along the inner aspect of the arm and be visible in many arm positions. I favor this position to the posterior scar, which often hypertrophies and even if it does not, imparts a tight and restrictive sensation. A posterior scar tends to flatten the tapering appearance along the posterior aspect of the central arm.
Summary of steps
1. Determine the role of liposuction and the relationship of the brachioplasty to anticipated upper body contouring.
2. Use appropriate anatomical landmarks and pinching of tissues and superior advancement of the posterior axillary fold when drawing the surgical markings.
3. The long hemiellipse lies along the inferior medial arm, and lateral chest ellipse descends vertically and inferior to the axilla.
4. The two ellipses are connected by a transaxillary chevron.
5. The L drawing should be accurate for surgery.
6. Thorough liposuction beneath the area to be excised will leave behind desirable connective tissue and vasculature
7. Excise the excess skin within the perimeter markings with limited removal of additional subcutaneous tissue.
8. Advance the triangular flap that contains the posterior axillary fold and secure with a braided absorbable stitch to superior axillary fascia.
9. Align the closure with towel clips, using the premarked hatch marks.
10. Close the subcutaneous layer with a horizontal running 2-0 braided absorbable suture.
11. Close the dermis with a horizontal running 3-0 monofilament absorbable suture.
Abramson DL. Minibrachioplasty: Minimizing scars while maximizing results. Plast Reconstr Surg. 2004;114:1631–1634.
Baroudi R. Dermolipectomy of the upper arm. Clin Plast Surg. 1975;2:485–491.
Hurwitz DJ, Agha-Mohammadi S. Post bariatric surgery breast reshaping: The spiral flap. Ann Plast Surg. 2006;56:481–486.
Hurwitz DJ, Holland SW. The L brachioplasty: An innovative approach to correct excess tissue of the upper arm, axilla and lateral chest. Plast Reconstr Surg. 2006;117:403–411.
Juri J, Juri C, Elias J. Arm dermolipectomy with a quadrangular flap and “T” closure. Plast Reconstr Surg. 1979;64(4):521–525.
Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96:912–920.
Pascal JF. Brachioplasty. Aesthet Plast Surg. 2005;29:423–429.
Pitanguy I. Correction of lipodystrophy of the lateral thoracic aspect and inner side of the arm and elbow. Clin Plast Surg. 1975;2:477–483.
Regnault P. Brachioplasty, axilloplasty, and pre-axilloplasty. Presented at VII International Congress of the Confederation of Plastic and Reconstructive Surgery, Rio de Janiero May 20–25, 1979. Abstract in Transaction of the Seventh International Congress of Plastic and Reconstructive Surgery, São Paulo. Cartgraft, 1979, p. 639.
Richards ME. Minimal-incision brachioplasty: A first-choice option in arm reduction surgery. Aesthet Surg J. 2001;21:301–310.
Strauch B. A technique of brachioplasty. Plast Reconstr Surg. 2004;113:1044–1052.
Temourian B. Rejuvenation of the upper arm. Plast Reconstr Surg. 1998;102:545–552.