CHAPTER 50 Bone-Ligament-Bone Reconstruction
Rationale and Basic Science
Scapholunate dissociation is a vexing problem facing hand surgeons. It is the most common form of carpal instability.1–4 Untreated scapholunate interosseous ligament (SLIL) disruption leads to significant degenerative changes of the carpus.4–8 A multitude of treatment options are described, which suggests that an optimal strategy has yet to be discovered.5,9–41 Partial wrist fusion, although a durable solution, trades off improvements in pain with decreased range of motion and strength.38
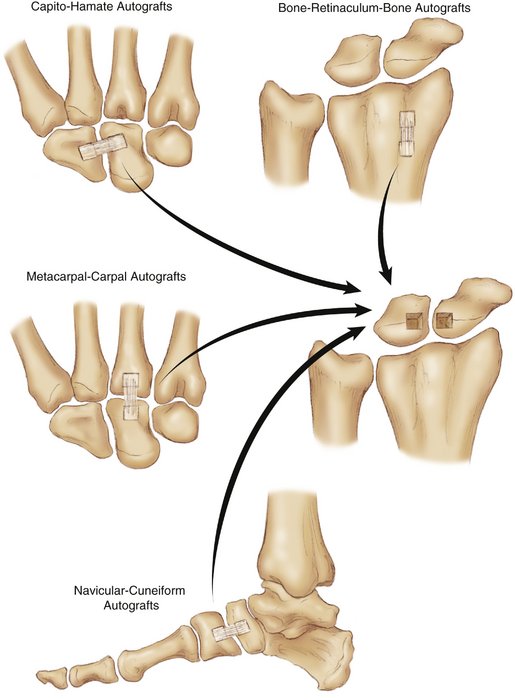
The great strides made in anatomical anterior cruciate ligament reconstruction over the past 30 years have led some hand surgeons to consider a similar model for SLIL reconstruction. Biomechanical studies show that the dorsal portion of the ligament is strongest and most important functionally.8,42–47 The yield strength of the dorsal region was 260N, more than twice that of the palmar region.42 Reconstruction of the dorsal ligament also is appealing given the ease of exposure through a standard dorsal approach. Various composite grafts have been investigated, including bone-retinaculum-bone from the distal radius,30 navicular-cuneiform autograft,27,41 SLIL allograft,5,12 metacarpal-carpal composite,48 and capitohamate ligament,42 in an attempt to match the strength, stiffness, and functionality of the native SLIL (Fig. 50-1).
Navicular-Cuneiform Autografts
Davis and colleagues41 reported on the use of the dorsomedial portion of the navicular–first cuneiform ligament. Although weaker than the SLIL, its minimal donor morbidity made it an acceptable clinical choice. The graft is harvested through a medial incision with posterior retraction of the tibialis anterior. Each bone plug measures 10 × 5 × 5 mm and is secured with small screws. The same group of investigators reported several cases of tissue elongation without loss of angulation.49 Commentary on donor site morbidity has not been published at this point. Svoboda and associates27 reported on the biomechanics of several other bone-tendon-bone complexes in the foot (e.g., tarsometatarsal ligament); however, none of these have been reported in clinical use.
Metacarpal-Carpal Autografts
Metacarpal-carpal grafts have several appealing features. The articulation at the base of the second or third metacarpal is relatively immobile and perhaps expendable. It can be harvested through the same dorsal incision as the reconstruction. These grafts more closely approximate the strength and stiffness of the SLIL than distal radius retinaculum grafts.48 Early results from a small case series are encouraging.50 The two main complications—graft pullout and graft stretching—are similar to reports with other types of bone-tendon-bone grafts. Graft stretching typically occurs after several months, perhaps during the revascularization phase of healing. There is loss of a tight SLIL interval, but the scapholunate angle is usually maintained. Graft pullout is seen more often in cases with poor lunate bone quality. A vascularized third metacarpal-carpal bone graft may have some benefit in these cases.49
Capitohamate Autografts
Berger’s group51 pioneered the use of the capitohamate graft for SLIL reconstruction. There are three capitohamate interosseous ligaments—dorsal, deep, and palmar. The dorsal ligament has a load to failure of 133N. The dorsal ligament is clinically feasible to harvest, and preservation of the deep and palmar ligaments is likely to maintain the capitohamate orientation. Berger supplements the repair with a capsulodesis and pins. Protected motion is started at 4 weeks, and pins are removed at 8 weeks. There are no clinical results published yet on this technique. Berger has commented that he does not perform this reconstruction if the lunate is translated ulnarly more than 50% out of the fossa.49
Authors’ Preferred Technique (Distal Radius Retinaculum Graft)
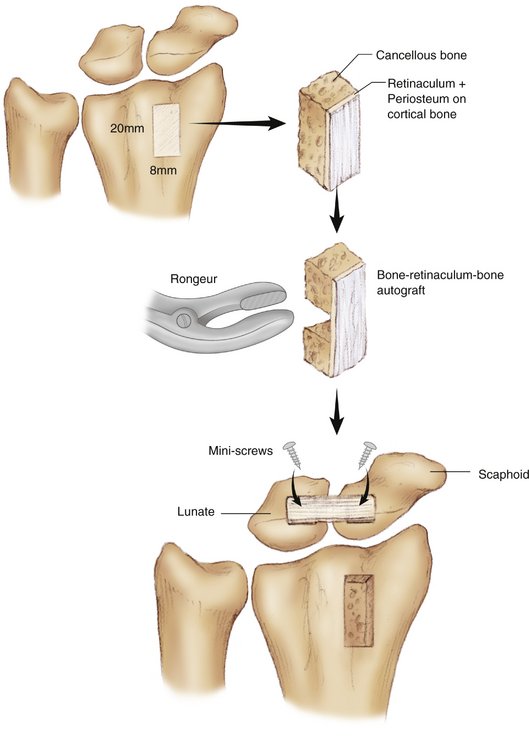
A standard dorsal midline approach is made. The extensor pollicis longus is released on the ulnar side and transposed radially. Using a small osteotome, a single 20 × 8 × 8 mm bone block with the overlying periosteum and retinaculum is harvested from the distal radius near Lister’s tubercle between the second and third compartments (Fig. 50-2). A 2- to 3-mm segment of cancellous and cortical bone is removed from the midportion of the bone block with a fine rongeur. Care is taken not to disrupt the overlying periosteum and retinaculum.
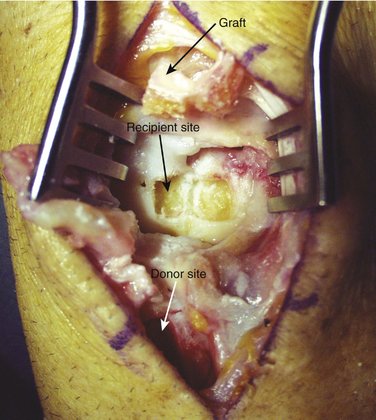
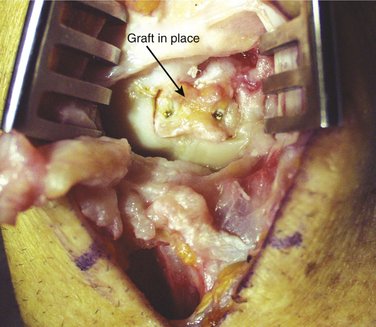
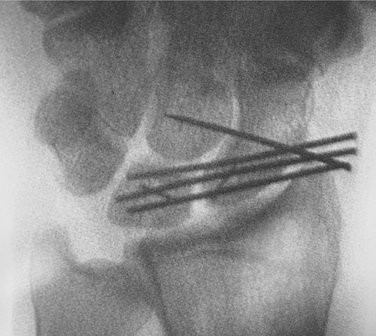
The capsule between the second and fourth compartment is incised longitudinally or via a ligament-sparing incision to expose the scapholunate interval. The wrist is flexed to improve visibility of the joint, and Kirschner wires (K-wires) are placed into the scaphoid and lunate for use as joysticks (Fig. 50-3). After reduction is confirmed on fluoroscopy, two 0.045-inch K-wires are drilled from the scaphoid into the lunate to capture the reduction. The joystick K-wires are removed. With a small osteotome, troughs are cut in the scaphoid and lunate adjacent to the joint, matching the size of the harvested graft (Fig. 50-4). The graft is digitally impacted into the scaphoid and lunate. A 1.3-mm screw is placed into each graft, securing them to the scaphoid and lunate (Fig. 50-5). Intraoperative fluoroscopy is used to check the alignment and placing of the screws and K-wires (Fig. 50-6). The capsule is repaired with imbrication as needed. Short arm spica immobilization in wrist extension is used for 6 weeks.
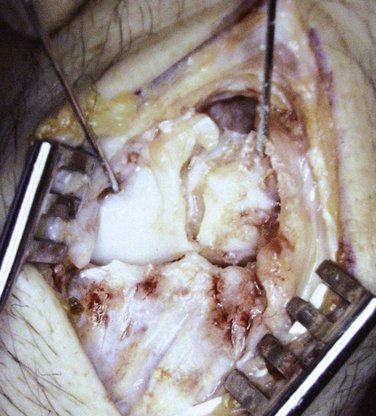
FIGURE 50-3 The use of Kirschner wires as joysticks to reduce the scapholunate interval before transfixing with Kirschner wires is essential.
Harvey and colleagues49 reported on 20 patients with a distal radius bone-retinaculum-bone reconstruction augmented with a Herbert screw, placed percutaneously from the radial side. The screw is removed at 9 to 12 months. One patient had screw pullout with gapping of the scapholunate interval, and another had a fixed dorsal intercalated segment instability deformity. Eighty percent of their first 20 patients returned to their previous occupations.
Results
In 1998, Weiss31 first reported on 19 patients treated with distal radius bone-retinaculum-bone fixation of the SLIL. Three of the five patients in this group with a static deformity went on to further surgery (proximal row carpectomy, radioscapholunate fusion, wrist arthrodesis). In a longer term examination of the 14 patients (15 wrists) with dynamic instability, we report the following results. Five could not be located. Of the remaining nine, three had subsequent surgery (one had proximal row carpectomy, and two had wrist arthrodesis). The reason for failure of these three is unknown. It could be that the ligament reconstruction tears through the soft tissue substance. We have not seen evidence that the bone plugs displace. For the other six, follow-up averaged 8.5 years. Average grip strength was 119 lb. Wrist flexion averaged 49 degrees, and wrist extension averaged 58 degrees (Fig. 50-7). Three patients had no pain, and three had mild pain with activity. All returned to work at their previous occupation. Mayo wrist scores were three excellent, two good, and one fair. The graft does not seem to stretch out over time. The natural history postoperatively is that if the graft remains intact for 6 to 12 months, it will stay so. We have noticed minor degenerative changes (usually around the junction of the scaphoid and lunate with slight spurring), but no loss of height of the radiolunate or radioscaphoid joints.
1. Dobyns J, Linscheid F, Chao E, et al. Traumatic instability of the wrist. Instr Course Lect. 1975;24:182-199.
2. Linscheid R. Scapholunate instabilities (dissociations, subdissociations, distraction). Ann Chir Main. 1984;3:323-330.
3. Mayfield J. Wrist ligamentous anatomy and pathogenesis of carpal instability. Orthop Clin. 1984;15:209-216.
4. Watson HK, Weinzweig J, Zeppieri J. The natural progression of scaphoid instability. Hand Clin. 1997;13:39-49.
5. Ashmead D, Watson H, Damon C, et al. Scapholunate advanced collapse wrist salvage. J Hand Surg [Am]. 1994;19:741-750.
6. Krakauer J, Bishop A, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg [Am]. 1994;19:751-759.
7. Linscheid RL. Scapholunate ligamentous instabilities (dissociations, subdislocations, dislocations). Ann Chir Main. 1984;3:323-330.
8. Viegas SF. The dorsal ligaments of the wrist. Hand Clin. 2001;17:65-75.
9. Augsberger S, Necking L, Horton J, et al. A comparison of scaphoid-trapezium-trapezoid fusion and four bone tendon weave for scapholunate dissociation. J Hand Surg [Am]. 1992;17:360-369.
10. Beredjiklian PK, Dugas J, Gerwin M. Primary repair of the scapholunate ligament. Tech Hand Upper Extrem Surg. 1998;2:269-273.
11. Bickert B, Sauerbier M, Germann G. Scapholunate ligament repair using the Mitek bone anchor. J Hand Surg [Br]. 2000;25:188-192.
12. Coe M, Spitellie P, Trumble T, et al. The scapholunate allograft: A biomechanical feasibility study. J Hand Surg [Am]. 1995;20:590-596.
13. Cohen MS, Taleisnik J. Direct ligamentous repair of scapholunate dissociation with capsulodesis augmentation. Tech Hand Upper Extrem Surg. 1998;2:18-24.
14. Harvey EJ: Hand based autograft replacement of the scapholunate ligament: early clinical outcome. American Society for Surgery of the Hand Annual Meeting, Seattle, WA, 2000.
15. Lavernia CJ, Cohen MS, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg [Am]. 1992;17:354-359.
16. Linscheid RL, Dobyns JH. Treatment of scapholunate dissociation: Rotatory subluxation of the scaphoid. Hand Clin. 1992;8:645-652.
17. Lutz M, Haid C, Steinlechner M, et al. Scapholunate ligament reconstruction using a periosteal flap of the iliac crest: A biomechanical study. Arch Orthop Trauma Surg. 2004;124:262-266.
18. Minami A, Kaneda K. Repair and/or reconstruction of scapholunate interosseous ligament in lunate and perilunate dislocations. J Hand Surg [Am]. 1993;18:1099-1106.
19. Minami A, Kato H, Iwasaki N. Treatment of scapholunate dissociation: ligamentous repair associated with modified dorsal capsulodesis. Hand Surg. 2003;8:1-6.
20. Misra A, Hales P. Blatt’s capsulodesis for chronic scapholunate instability. Acta Orthop Belg. 2003;69:233-238.
21. Muermans S, De Smet L, Van Ransbeeck H. Blatt dorsal capsulodesis for scapholunate instability. Acta Orthop Belg. 1999;65:434-439.
22. Palmer A, Dobyns J, Linscheid F. Management of post-traumatic instability of the wrist secondary to ligament rupture. J Hand Surg. 1978;3:507-532.
23. Saffar P, Sokolow C, Duclos L. Soft tissue stabilization in the management of chronic scapholunate instability without osteoarthritis: a 15-year series. Acta Orthop Belg. 1999;65:424-433.
24. Schweizer A, Steiger R. Long-term results after repair and augmentation ligamentoplasty of rotatory subluxation of the scaphoid. J Hand Surg [Am]. 2002;27:674-684.
25. Shin SS, Moore DC, McGovern RD, et al. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft: A biomechanic and histologic study. J Hand Surg [Am]. 1998;23:216-221.
26. Slater RRJr, Szabo RM, Bay BK, et al. Dorsal intercarpal ligament capsulodesis for scapholunate dissociation: biomechanical analysis in a cadaver model. J Hand Surg [Am]. 1999;24:232-239.
27. Svoboda S, Eglseder W, Belkoff S. Autografts from the foot for reconstruction of the scapholunate interosseous ligament. J Hand Surg [Am]. 1995;20:980-985.
28. Viegas SF, Dasilva MF. Surgical repair for scapholunate dissociation. Tech Hand Upper Extrem Surg. 2000;4:148-153.
29. Watson H, Hempton R. Limited wrist arthrodesis, I: the triscaphe joint. J Hand Surg. 1980;5:320-327.
30. Weiss AP. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft: a new technique. AAOS Trans. 1996;213:169.
31. Weiss AP. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft. J Hand Surg [Am]. 1998;23:205-215.
32. Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg [Am]. 1997;22:344-349.
33. Wintman B, Gelberman R, Katz J. Dynamic scapholunate instability: results of treatment with dorsal capsulodesis. J Hand Surg [Am]. 1995;20:971-979.
34. Wolf JM, Weiss AP. Bone-retinaculum-bone reconstruction of scapholunate ligament injuries. Orthop Clin North Am. 2001;32:241-246.
35. Wyrick JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation. J Hand Surg [Br]. 1998;23:776-780.
36. Zarkadas PC, Gropper PT, White NJ, et al. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg [Am]. 2004;29:848-857.
37. Blatt G. Capsulodesis in reconstructive hand surgery: dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81-102.
38. Kleinman W, Carrol C. Scapho-trapezio-trapezoid arthrodesis for treatment of static and dynamic scapholunate instability: a ten year prospective on pitfalls and complications. J Hand Surg [Am]. 1990;15:408-414.
39. Brunelli F, Spalvieri C, Bremner-Smith A, et al. [Dynamic correction of static scapholunate instability using an active tendon transfer of extensor brevi carpi radialis: preliminary report]. Chir Main. 2004;23:249-253.
40. Brunelli GA, Brunelli GR. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg [Am]. 1995;20(3 Pt 2):S82-S85.
41. Davis CA, Culp RW, Hume EL, et al. Reconstruction of the scapholunate ligament in a cadaver model using a bone-ligament-bone autograft from the foot. J Hand Surg [Am]. 1998;23:884-892.
42. Berger RA, Imeada T, Berglund L, et al. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg [Am]. 1999;24:953-962.
43. Kauer J. Functional anatomy of the wrist. Clin Orthop. 1980;149:9-20.
44. Short W, Werner F, Fortino M, et al. A dynamic biomechanical study of scapholunate ligament sectioning. J Hand Surg [Am]. 1995;20:986-999.
45. Short WH, Werner FW, Green JK, et al. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: part II. J Hand Surg [Am]. 2005;30:24-34.
46. Tang JB, Ryu J, Omokawa S, et al. Wrist kinetics after scapholunate dissociation: the effect of scapholunate interosseous ligament injury and persistent scapholunate gaps. J Orthop Res. 2002;20:215-221.
47. Viegas SF, Yamaguchi S, Boyd NL, et al. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg [Am]. 1999;24:456-468.
48. Harvey E, Hanel D. Autograft replacements for the scapholunate ligament: a biomechanical comparison of hand based autografts. J Hand Surg [Am]. 1999;24:963-967.
49. Harvey EJ, Berger RA, Osterman AL, et al. Bone-tissue-bone repairs for scapholunate dissociation. J Hand Surg [Am]. 2007;32:256-264.
50. Harvey E, Hanel D. What is the ideal replacement for the scapholunate ligament in a chronic dissociation? Can J Plast Surg. 2000;8:143-146.
51. Ritt MJ, Berger RA, Kauer JM. The gross and histologic anatomy of the ligaments of the capitohamate joint. J Hand Surg [Am]. 1996;21:1022-1028.