Nursing fundamentals textbooks provide comprehensive discussions of measurement of vital signs. Only significant pediatric variations in the measurement of body temperature, pulse, and respirations are presented here.
Measurement of Body Temperature
Rationale
Environmental factors and relatively minor infections can produce a much higher temperature in infants and young children than would be expected in older children and adults. In most cases, an elevated temperature is the result of fever and is one of the most common manifestations of illness in young children. In very young infants, fever might be one of the few signs of an underlying disorder. In toddlers, febrile convulsions can parallel fever and are of particular concern. Ascertaining the absence or presence of fever and determining the cause of fever are important in planning nursing care. Body temperature should be measured on admission to the health care facility, before and after surgery or invasive diagnostic procedures, during the course of an unidentified infection, after fever-reduction measures have been taken, and any time that an infant or child looks flushed, feels warm, is lethargic, looks “glassy-eyed,” or has increased pulse and respirations.
Anatomy and Physiology
Temperature is regulated from within the hypothalamus. During an infection, the body’s normal set point is elevated, and the hypothalamus increases heat production until the body’s core temperature is consistent with this new set point. Shivering and vasoconstriction during the chill phase help the body reach the new set point by conserving and generating heat.
The control of body heat loss improves with age. The ability of muscles to shiver increases with maturity, and the child accumulates greater amounts of adipose tissue necessary for insulation against heat loss. Heat production decreases with age. The infant produces relatively more heat per unit of body weight than older children do, as reflected by the infant’s higher average body temperature (Table 8-1). A variety of other factors also affect the body temperature of the child (Table 8-2).
| Temperature in Degrees | ||
|---|---|---|
| Age | Celsius | Fahrenheit |
| 3 mo | 37.4 | 99.4 |
| 1 yr | 37.6 | 99.7 |
| 3 yr | 37.2 | 99.0 |
| 5 yr | 37.0 | 98.6 |
| 7 yr | 36.8 | 98.3 |
| 9 yr | 36.7 | 98.1 |
| 13 yr | 36.6 | 97.8 |
| Factor | Effect |
|---|---|
| Active exercise | Might temporarily raise temperature |
| Stress, crying | Raises body temperature |
| Diurnal variation | Body temperature is lowest between 0100 and 0400 hours (1:00 and 4:00 AM), highest between 1600 and 1800 hours (4:00 and 6:00 PM) |
| Environment, including clothing, swaddling, and nesting | Body temperature can vary with room temperature, amount and type of clothing |
| Pharmacologic agents (antipyretics, muscle relaxants, vasodilating anesthetic agents) | Decrease body temperature |
Preparation
Ask the parent or child if the child has been febrile, and if so, when the fever began. Inquire whether the onset was abrupt or gradual and whether other symptoms or localizing signs accompany the fever. Most diseases have no particular fever pattern. However, although the rapidity of temperature elevation and response to antipyretics are not indicative of the severity of the disease, knowing the pattern of the fever (onset, magnitude, frequency, recurrence, defervescence or decrease) can be helpful, especially if there are no localizing signs with the fever (Table 8-3).
| Fever Pattern | Associated Etiologies | Additional Characteristics of Fever |
|---|---|---|
| Single spike: refers to a single increase or spike, usually within a 12-hour period or less | Transfusion of blood or blood products | |
| Double quotient: fever in which there are two distinct peaks in a day | Miliary tuberculosis | Fever with general symptoms such as weight loss, malaise, weakness, anemia, pallor, diminished breath sounds, crackles |
| Hectic: involves wide swings in fever, usually with chills and sweating | Bacterial pneumonia | Fever usually quite high, chills, abrupt onset, anorexia, headache, cough, meningeal symptoms |
| Intermittent: fever returns to normal at least once during the day | Bacterial (infective) endocarditis | Low-grade fever with nonspecific symptoms such as malaise, myalgia, headache, diaphoresis, weight loss |
| Hodgkin’s disease | Low-grade fever with enlargement of supraclavicular or cervical nodes, weight loss, night sweats, pruritus, anorexia, nausea | |
| Remittent: fever rises at least 0.6° C (1.0° F) in a 24-hour period and abates but does not return to normal | Viral upper respiratory tract infections | Fever with myalgia, malaise, headache, coryza; slow defervescence |
| Continuous or sustained: little or no variation in temperature | Roseola | Fever above 39° C (102° F) for 3 to 4 days without localizing signs |
| Scarlet fever | High fever with vomiting, headache, chills, malaise, abdominal pain in prodromal stage | |
| Urinary tract infection (children younger than 5 years) | Fever of 39° C (102° F) or higher for 2 days or more, with no respiratory symptoms | |
| Severe acute respiratory syndrome (SARS) | Diarrhea, vomiting, irritability, poor feeding, foul-smelling urine | |
| Fever at or above 38.5° C (101.5° F), cough, malaise, chills or rigor, coryza (younger than 12 years), headache, sputum, myalgia, sore throat, no crackles or wheezing | ||
| Relapsing: recurrent over days and weeks; fever occurs at various intervals after initial episode | Acute rheumatic fever | Low-grade fever with late afternoon spike, polyarthritis, chorea, subcutaneous nodules, erythema marginatum, carditis |
| Infectious mononucleosis | Fever with malaise, sore throat, lymphadenopathy, splenomegaly that can persist for months | |
| Extreme hyperthermia: fever above 41° C (106° F) | Noninfectious origin (neoplastic, trauma, heat stroke, drug fever) HIV |
Guidelines for Measurement of Body Temperature
▪ Select the site for temperature measurement based on the child’s age and condition (Table 8-4), institutional policy, and what might be least traumatic for the child. The tympanic route, for example, has a high level of acceptability by children.
| Site | Age Group | Special Considerations |
|---|---|---|
| Axilla | All age groups, but particularly preschoolers, who tend to fear invasive procedures. Can be used for children for whom the oral route is not possible and for those who would not tolerate the rectal route. |
Measures shell temperature.
Can be taken using standard glass (in rare use), electronic, digital, chemical dot, or infrared thermometers.
Although some sources recommend the monitor mode for electronic thermometers, some evidence also suggests that the predictive mode be used for full-term infants.
Wearable chemical dot thermometers enable continuous reading for as long as 48 hours (must be replaced after 48 hours). Reading might be increased for axillary route.
Might be contraindicated when accuracy is especially critical or in the early stages of a fever when the axilla might not be sensitive to early changes. Accuracy can be affected by increased peripheral circulation.
|
| Rectal | All age groups. Some sources recommend use in children older than 2 years because of risks of breakage and perforation. Some evidence suggests that the rectal route is the most reliable route for measurement of temperature in infants and children, although others recommend its use only when no other route is appropriate (e.g., children who are too young or too agitated to cooperate or follow directions, children who have had oral or axillary surgery). |
Measures core temperature.
Can be taken using standard glass (in rare use), electronic, or chemical dot devices.
Do not force insertion of thermometer.
Do not use if child has diarrhea or rectal irritation, has had anal surgery, has had chemotherapy affecting the mucosa, or if it is possible to use oral or axillary sites. Presence of stool can decrease accuracy (reading might be increased).
|
| Oral | Cooperative 5- and 6-year-old children, school-age children, and adolescents. |
Reflects shell temperature (but might be less accurate in assessment of core temperature than rectal route).
Can be taken using standard glass (rarely used), electronic, digital, or chemical dot thermometry.
Do not use if child is uncooperative or unable to follow directions, is comatose, is seizure prone, has had oral surgery, mouth breathes, or is receiving oxygen therapy.
Electronic thermometry produces acceptable results for the child who keeps mouth open during measurement.
|
| Tympanic | All ages, although several sources suggest that the route is insufficiently sensitive and reliable for the detection of fever in children younger than 3 years and possibly even for children younger than 6 years. |
Considered to measure core temperature.
Easy to use, noninvasive, and quick for young children.
Might be contraindicated in young children and infants because of their small ear canals.
In children 3 years and younger, pull the ear down and back during temperature measurement (for ear-based temperature sensor). Tug not necessary for ear sensor type, which measures heat radiating from ear canal opening. For this type, insert hemispheric probe into opening.
Might be advisable to select another method if precise measurements are necessary or if clinical symptoms suggest fever in the presence of a normal or lower than expected tympanic measurement.
Calibrated to oral or rectal routes.
|
| Skin | All ages |
Measured using plastic strip thermometer.
Variable accuracy.
Beneficial for screening and for at-home use.
|
▪ Standard glass thermometers are not recommended for use because of risk of breakage and inhalation of toxic vapors. Temperature can be taken using electronic, tympanic, digital, and chemical indicator thermometers, as well as skin plastic strips (although these are recommended primarily for screening and at-home use).
▪ Position the child appropriately.
For axillary temperature, hold the child quietly on your lap. Diversions, such as reading, are useful. Hold the child’s arm firmly against the side.
For oral temperature, have the child sit or lie quietly.
For rectal temperature, place younger infants in a side-lying position. Large infants and children can be placed in prone or side-lying positions. If the parent is available, the child can wrap arms around the parent’s neck and legs around the parent’s waist or be placed prone across the parent’s lap.
▪ Always record the route by which the temperature was taken, because the differences between routes cannot be assumed as constant. If possible, consistently use one route, because studies suggest variable differences among the routes. Normal peripheral temperature is usually considered to be 37° C (98.6° F).
▪ In addition to measurement of body temperature, all children should be assessed for:
Signs and symptoms of dehydration, including sunken anterior fontanel (infants younger than 18 months), decreased or absent tearing (children older than 6 weeks), sunken eye orbits, dry or sticky mucous membranes, dry body creases, and poor skin turgor (tenting when pinched)
Flushed appearance
Chills, as evidenced by shivering and piloerection
Restlessness
Lethargy
Skin mottling
Increased pulse, respiratory rates, and blood pressure
Twitching
Seizure activity
Young children might interpret “taking your temperature” as taking something away. Saying “let’s see how warm you are” can avoid this interpretation.
Rationale
The measurement of pulse is a routine part of hospital procedure but should not be underestimated as an easily accessible indicator of the status of the cardiovascular system. Disorders of the cardiovascular system, the effects of fever, and the effects of drug therapies can be monitored through assessment of pulse. The pulse should be routinely monitored during disease processes, during fever, before and after surgery, and whenever a child’s condition deteriorates. A decreased pulse rate is more ominous than tachycardia in a young child following trauma.
Anatomy and Physiology
Approximately 8.5% of the body weight in the neonate is blood volume, compared with 7% to 7.5% in the older child and adult. The heart size increases as the child grows, with a resultant decrease in heart rate. Variations in heart rate are much more dramatic in the child than in the adult. Table 8-5 lists normal pulse rates; Table 8-6, influences on pulse rate; and Table 8-7, deviations from normal pulse patterns.
| Age | Resting (Awake) | Resting (Asleep) | Exercise and Fever |
|---|---|---|---|
| Birth | 100–180 | 80–160 | Up to 220 |
| 1–3 mo | 100–220 | 80–180 | Up to 220 |
| 3 mo to 2 yr | 80–150 | 70–120 | Up to 200 |
| 2 -10 yr | 70–110 | 60–100 | Up to 180 |
| 10 yr to adult | 55–90 | 50–90 | Up to 180 |
| Influence | Effect |
|---|---|
| Medications | Aminophylline, racemic epinephrine, atropine sulfate increase pulse rate. Digoxin decreases pulse rate. |
| Activity | Activity increases pulse rate. Sustained, regular exercise eventually decreases rate. Pulse varies if a child is sleeping, increasing during inspiration and decreasing during expiration (sinus arrhythmia). Crying and feeding increase pulse rate in an infant. |
| Fever | Increases pulse rate by about 10 to 15 beats per degree (in Celsius) temperature increase. High fever accompanied by low pulse and respiratory rates can signal a drug reaction. Low fever with high pulse and respiratory rates can signal septic shock. Tachypnea in children younger than 2 years, with a fever, might be the most sensitive predictor of pneumonia. |
| Apprehension, acute pain | Increases pulse rate. |
| Hemorrhage | Increases pulse rate. |
| Increased intracranial pressure | Decreases pulse rate. |
| Respiratory distress | Pulse rate increases in early distress and decreases in late distress. |
| Pulse | Characteristics and Significance |
|---|---|
| Bradycardia | Slowed pulse rate. |
| Tachycardia | Increased pulse rate. In the absence of apprehension, crying, increased activity, or fever, tachycardia can indicate cardiac disease. |
| Sinus arrhythmia | Pulse rate increases during inspiration, decreases during expiration. Sinus arrhythmia is a normal variation in children, especially during sleep. |
| Alternating pulse (pulsus alternans) | Alteration of weak and strong beats. Might indicate heart failure. |
| Bigeminal pulse | Coupled beats related to premature beats. |
| Paradoxical pulse | Strength of pulse diminishes with inspiration. |
| Thready pulse | Weak, rapid pulse. Might be indicative of shock. Pulse is difficult to palpate; seems to appear and disappear. |
| Corrigan’s pulse (water-hammer pulse) | Forceful, jerky beat caused by wide variation in pulse pressure. |
Preparation
Ask the parent or child about a family history of arrhythmias, atherosclerosis, or myocardial infarction. Ask if the child has known heart disease or has experienced or is experiencing palpitations or arrhythmias. Determine if fever or pain is present, and ask if the child has recently taken medications or substances that might be expected to affect pulse rate.
▪ Measure the pulse when the infant or child is quiet or, preferably, asleep. Because of lability of the pulse, carefully document the child’s activity or anxiety level when the pulse is recorded.
▪ Select the appropriate site. The apical pulse is measured in children younger than 2 years of age because the radial pulse is difficult to locate. The apical pulse should be measured at any age when the radial pulse is difficult to locate, when cardiac disease has been identified, or when the radial pulse is irregular. Radial, femoral, and popliteal pulses should be compared at least once in the young child to detect circulatory impairment.
▪ Listen for the apical pulse at the point of maximal impulse (PMI). This will be found in the fourth intercostal space in children younger than 7 years. In children older than 7 years the apical pulse will be found in the fifth interspace and will be more lateral.
▪ Take radial and apical pulses for 1 full minute because of possible alterations in rhythm. If frequent apical pulses are required, use shorter counting times.
▪ Pulses can be graded (Table 8-8).
| Grade | Meaning |
|---|---|
| 0 | Not palpable. |
| +1 | Thready, weak. Difficult to find. Easily obliterated. |
| +2 | Difficult to find. Pressure might obliterate. |
| +3 | Easy to find. Difficult to obliterate (normal). |
| +4 | Bounding, strong. Cannot be obliterated. |
Measurement of Respirations
Rationale
Assessment of respiration involves external assessment of ventilation. Because the quality and rate of respirations can be affected by disorders in every body system, the character of respirations must be carefully assessed and reported.
Anatomy and Physiology
Infants and young children inhale a relatively small amount of air and exhale a relatively large amount of oxygen. Young children and infants have fewer alveoli and therefore less alveolar surface through which gas exchange can occur. These factors, together with a higher metabolic rate, are influential in increasing respiratory rates in infants and children. Table 8-9 outlines normal respiratory rates, and Table 8-10 outlines influences on respiratory rates.
| Rights were not granted to include this data in electronic media. Please refer to the printed book. |
| Influencing Factor | Effect |
|---|---|
| Age |
Respiratory rate decreases as the child grows older.
The rate tends to increase dramatically in infants and young children relative to anxiety, crying, fever, disease.
The rhythm is irregular in young infants, who experience sharp increases in rate and apneic spells. (Apneic spells of 15–20 seconds or longer are considered pathologic.)
|
| Medications | Narcotic analgesics decrease respiratory rate. Xanthine derivatives can cause an increase in rate. |
| Position | Slumping impedes ventilatory movements. |
| Fever | Respirations increase in rate and depth. |
| Increased activity | Respirations increase in rate or depth. |
| Anxiety or fear | Respirations increase in rate and depth. |
| Pathologic states | Respiratory rate, rhythm, and depth alter as a result of cerebral trauma, respiratory disorders, hemorrhage, anemia, meningitis, cardiac disorders, infectious disorders, and tetanus. |
| Pain | Respiratory rate can decrease or increase. |
Preparation
Ask the parent or child about the use of medications; whether there is difficulty breathing, or apnea (infants); and about the presence of respiratory infections or fever. Inquire about a family history of cardiac or respiratory disorders.
Guidelines for Measurement of Respirations
▪ Assess the infant’s or child’s respirations before beginning more intrusive procedures. If the infant or child is already crying, wait for calmer behavior before assessing respiratory rates.
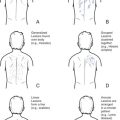
▪ Avoid letting the child know that respirations are being counted; self-consciousness can alter the respiratory rate and depth. Assess the respirations when counting the pulse or performing an assessment of the thorax and lungs. Table 8-11 gives a description of respiratory rhythms.
| Pattern | Description |
|---|---|
| Dyspnea | Difficult or labored breathing; indicated by presence of retractions. |
| Bradypnea | Abnormally slow rate of breathing; rhythm regular. |
 |
|
| Tachypnea | Abnormally fast rate of breathing. |
 |
|
| Hyperpnea | Rapid, deep respirations. |
 |
|
| Apnea | Absence of respirations. |
 |
|
| Cheyne-Stokes respiration (periodic breathing) |
Periods of deep, rapid breathing alternating with periods of apnea.
Commonly seen in infants, and can be seen normally in children during deep sleep. Abnormal causes include drug-induced depression and brain damage.
|
 |
|
| Kussmaul’s respiration |
Abnormally deep breathing. Can be rapid, normal, or slow.
Commonly associated with metabolic acidosis.
|
 |
|
| Biot’s respiration (ataxic breathing) | Unpredictable, irregular breathing. Seen with lower brain damage and respiratory depression. |
 |
▪ When assessing the respirations of infants and younger children, the nurse places fingers or a hand just below the child’s xiphoid process so that the inspiratory rises can be felt. Alternatively, the respirations can be assessed by listening to breath sounds through the stethoscope. In infants, respirations can also be assessed by observing abdominal movements because respirations are diaphragmatic.
▪ Observe a complete respiratory cycle (inspiration plus expiration).
Count respirations for 1 full minute. Respirations of infants and young children can be quite irregular.
While counting, note the depth and rhythm of breathing. Depth is a subjective estimation and is usually noted as shallow, normal, or deep. If unable to label a rhythm, describe it.
▪ Observe the child for:
Cyanosis of the nailbeds, hands, and feet, which might indicate central or peripheral cyanosis. Peripheral cyanosis can be caused by vasoconstriction and is common in the young infant.
Cyanosis of the lips, oral mucosa, and generalized body cyanosis are indicative of central cyanosis. Central cyanosis indicates a significant drop in the oxygen-carrying capacity of the blood.
Restlessness, anxiety, and decreasing levels of consciousness, which can be related to hypoxia.
Related Nursing Diagnoses
Anxiety: related to threat to health status.
Hypothermia: related to cool environment, medication, inadequate clothing, malnutrition, decreased metabolic rate, inactivity.
Hyperthermia: related to illness or trauma, increased metabolic rate, medications or anesthesia, hot environment, dehydration, inappropriate clothing.
Altered tissue perfusion, cardiopulmonary and peripheral: related to hypovolemia, hypoventilation; interruption of flow, venous or arterial; impaired transport of oxygen; exchange problems.
Decreased cardiac output: related to illness or trauma.
Impaired gas exchange: related to alveolar-capillary membrane exchanges, ventilation perfusion imbalance.
Ineffective airway clearance: related to smoking, second-hand smoke, smoke inhalation, airway spasm, retained or excessive secretions, foreign body in airway, infection, allergic airways, asthma.
Altered family processes: related to shift in health status, situational crisis.
Risk for activity tolerance: related to imbalance between oxygen supply and demand.
Knowledge deficit: related to unfamiliarity with information resources.