CHAPTER 5 Blood gas results
Blood gas report
Each intensive care unit should have an on-site blood gas machine. All give similar results.
The blood gas machine discussed here as an example is the Radiometer ABL 730. For blood gas analysis it measures three blood gas parameters — pH, PaO2 and PaCO2. A printed report from this machine is shown on page 54 as an example. Since, clearly, different machines will give different reports, it is important to be aware of exactly what your unit’s machine measures and reports. The report in the example is divided into eight parts:
Figure 5.1 shows an example from the Intensive Care Nursery (ICN) gas machine at the Royal Brisbane and Women’s Hospital.
Notes on calculated values
Standard bicarbonate, cHCO3−(P,st)c
We suggest using base excess (see below) rather than bicarbonate for these types of interpretations.
Actual bicarbonate
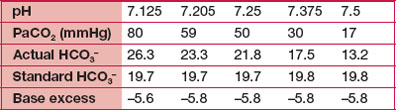
This value varies in proportion with changes in PaCO2, in contrast with the standard bicarbonate which will not change with changes in PaCO2, only with changes in acid or base content of the blood sample. Note in the examples below, all calculated on the same sample of blood, how the actual bicarbonate reflects the PaCO2 changes, while the standard bicarbonate and base excess remain constant.
Base excess
For example, in the first example in Table 5.1 above, with a pH of 7.125, there is only a small metabolic acid contribution to this significant acidosis (BE −5.6). The major contributor to the acidosis is the high PaCO2 of 80 mmHg (i.e. respiratory acidosis). A contrasting pH of 7.125 with a PaCO2 of 40 mmHg has no respiratory contribution, and a major metabolic contribution with a BE of −16. A spontaneously breathing newborn baby with this degree of metabolic acidosis would more likely have a PaCO2 of around 28 mmHg, created by over-breathing in response to the low pH — thus raising the pH to 7.19, a partial ‘respiratory compensation’ for a metabolic acidosis.
Alveolar–arterial difference in partial pressure of oxygen, pO2(A–a)e
This is derived from the alveolar gas equation. A large pO2(A–a) value indicates that there is a lot more oxygen in the alveolus than in the arteries, and the patient has a serious problem getting oxygen into the blood from the alveoli. There is a major ventilation–perfusion (V/Q) mismatch and/or a major gas diffusion problem.
Blood oximetry values
Many preterm infants have a HbF concentration in excess of 90% at birth. Term infants have about 80%. The cHbF drops quickly with transfusion, which is always with adult blood.
Acidosis
In neonatal practice, many instances of respiratory and metabolic acidosis are seen. In treating these, the best principle is to treat respiratory acidosis with respiratory treatments, and treat metabolic acidosis with metabolic management (e.g. administration of alkali, volume expansion for better perfusion). Many times it is appropriate to accept a respiratory acidosis, particularly in an infant with respiratory disease who is spontaneously breathing. Treatment of respiratory acidosis in a ventilated infant will depend on the underlying lung pathology. The principle is to increase alveolar ventilation. See section on conventional mechanical ventilation, page 37.
HCO3− + H+ ↔ H2CO3 ↔ H2O + CO2
must occur for the bicarbonate to ‘mop up’ hydrogen ions. If CO2 cannot be removed there is little point in administering bicarbonate, e.g. if the PaCO2 is >60 mmHg.