Chapter 77 Blast injury and gunshot wounds
pathophysiology and principles of management
Widespread terrorist outrages in the recent past have once again served to emphasise that unpredictable events can suddenly deliver numbers of casualties to civilian hospitals, with unfamiliar patterns of injury. An understanding of the pathophysiology of blast injury, and the impact of such events on hospital function, will help medical staff make appropriate management decisions, often under difficult circumstances.1–4
BLAST INJURY
PHYSICS OF EXPLOSIONS5
An explosion is the almost instantaneous release of stored energy. The energy may come from, for example, pressurised gas, a nuclear reaction or stored chemical energy. Thus specific ‘explosives’ are not necessarily required. Explosives are materials that contain stored chemical energy that may be released rapidly. High-performance explosives release this energy by means of a chemical reaction which propagates through the explosive material faster than the speed of sound; thus the detonation velocity is of the order of 8 km/s compared with the speed of sound in air, 0.33 km/s.5 This produces a supersonic shock front (blast wave) with a rapidly expanding cloud of gaseous reaction products which causes damage to structures and people in the vicinity. In effect, there is an extremely rapid increase in atmospheric pressure, ‘positive overpressure’, the duration of which is dependent on the magnitude of the explosive charge. This dies away exponentially and is followed by a negative pressure phase produced by gases forced away from the centre of the blast leaving a vacuum. Blast winds may subsequently move paradoxically towards the explosion as pressures equalise.
CLASSIFICATION OF BLAST INJURY
By convention blast injuries are classified according to which feature of the explosion was involved in wound generation.6,7 In outline:
EXPLOSIVE DEVICES (Table 77.1)
Conventional military anti-personnel devices rely on fragment generation to produce ‘secondary’ injuries. The device’s casing is designed to produce fragments, and may contain preformed fragments or notched wire to increase the fragment load. An 81 mm mortar round contains a small quantity (∼1 kg) of high explosive; the blast itself would only be lethal within 2–3 m, but the fragment cloud generated will seriously injure or kill within a radius of around 85 m. Improvised explosive devices (IED), built by terrorists, contain material (e.g. bolts, nails) to increase secondary injury. Larger devices, such as air-delivered free-fall bombs, missiles or artillery shells, contain sufficient explosive to produce secondary injury by throwing bricks, masonry debris and glass substantial distances. In addition, the blast may collapse physical structures such as walls and buildings.
| Conventional munitions: e.g. grenades, aerial bombs, mortar bombs, rockets | All types of blast injury may occur, but penetrating injuries from multiple fragments predominate. Primary fragments are derived from the munition; preformed within the shell or from the casing when the munition explodes. Other materials (building debris, vehicle components) energised by the blast form secondary fragments. |
| Terrorist devices: typically contain a few kilograms of explosive (NB: Recent attacks have been larger, more sophisticated and specifically designed to maximise casualties) | Although the reported incidence of primary blast injuries varies from 1 to 76%, serious primary blast injury is uncommon and secondary and tertiary injuries predominate. Mortality is low unless the device is large, explodes in a confined space or there is structural collapse. Less than 50% of those presenting to hospital will require admission.2 |
| Antipersonnel landmines: common in developing countries; indiscriminate in action | Patterns of injury:
• Traumatic amputation of foot or leg, due to standing on a buried ‘point detonating’ mine. Mine fragments, grass, soil, parts of shoe and foot are blown upwards with substantial proximal tissue damage and contamination.
|
PRIMARY BLAST INJURY
A blast wave passing through an individual behaves like an acoustic wave, giving up energy at interfaces between materials of differing acoustic quality, causing damage. Air-containing organs – the lungs, the gut and the ears – are particularly vulnerable.8,9 Massive pressure pulses, causing body wall distortion, can tear solid organs from their vascular supplies. Recent work suggests that traumatic amputation is caused by shock wave-induced stress concentrations that fracture the long bones which are subsequently removed by flailing and blast wind effects.10 This explains why amputations are generally not through joints.11
Primary blast injury (PBI) is unusual amongst survivors,12 but very common in those killed immediately.13 The blast wave dies away rapidly with distance, but device fragments and energised debris travel and injure at greater distances. If a casualty is close enough to sustain primary injury there will be overwhelming secondary and tertiary damage. The majority of survivors from an explosion will have sustained secondary or tertiary injuries.12 Military and terrorist devices are specifically designed to maximise casualties by the use of fragments.
THE LUNG
Immediate effects of severe blast exposure may include apnoea and bradycardia.9 The blast wave produces disruption of the alveolar–capillary barrier leading to intra-alveolar haemorrhage that may be massive. This occurs in regions of the chest subjected most directly to the incident blast wave (not by a pressure pulse travelling down the trachea). The wave may ‘echo’ around the pleural cavity, exhibiting interference effects and injuring other regions at points of stress wave concentration. Such regions include the juxtamediastinal tissue and the diaphragmatic recesses. Pulmonary contusions are produced, with associated shunt and reduction in compliance, and pulmonary fat embolism has recently been described.14 The surface of the lung may evolve bullae, which are mechanically weak and may rupture producing pneumothoraces. These may present early or late, perhaps triggered by mechanical ventilation. Damage to hilar structures may be produced by severe and long duration overpressures; pulmonary artery and vein injuries are usually rapidly fatal. A variety of clinical features have been described and these are summarised in Table 77.2. Radiological features are outlined in Table 77.3.
| Symptoms | Dyspnoea |
| Cough – dry to productive with frothy sputum; haemoptysis | |
| Chest pain or discomfort (typically retrosternal) | |
| Signs | Cyanosis |
| Torrential pulmonary haemorrhage | |
| Tachypnoea | |
| Reduced breath sounds, dullness to percussion | |
| Coarse crackles, wheeze | |
| Features of pneumothorax or haemopneumothorax. Subcutaneous emphysema. | |
| Retrosternal crunch (pneumomediastinum) | |
| Retinal artery air emboli |
Table 77.3 Radiological evidence of blast lung
| Diffuse pulmonary opacities or ‘infiltrates’ (typically these develop within a few hours, become maximal at 24–48 hours and resolve over 7 days) |
| Pneumothorax/haemopneumothorax |
| Interstitial (peribronchial) emphysema |
| Subcutaneous emphysema |
| Pneumomediastinum |
| Pneumoperitoneum (usually secondary to perforation of an abdominal viscus, but tension pneumoperitoneum has been ascribed to blast lung) |
Investigations obtained may depend on availability and prioritisation if the casualty burden is high. Chest X-ray (CXR), blood gas analysis and pulse oximetry monitoring are useful. CXR will provide data concerning pneumothorax, pneumomediastinum, subcutaneous and interstitial emphysema and subdiaphragmatic air from visceral perforation. The CXR is a poor modality for quantifying extent of contusion, for which computed tomography (CT) is better.15,16 CT may be unavailable or overwhelmed with demand. In the majority of cases CT will not provide management-altering data. The priority is close clinical observation of conventional parameters to identify the drift toward respiratory failure.
The management of significant PBI is similar to that of any other pulmonary contusion with a number of corollaries from the pathology. PBI renders the lungs prone to development of pneumothorax, and importantly, significant air emboli may be created.17 Historically, continuous positive airway pressure (CPAP) and mechanical ventilation were regarded as so hazardous as to be treatments of last resort. This was due to fear of creating or exacerbating air embolism. Modern strategies based around modest gas exchange targets, with limited volume excursion and pressure change, has ameliorated these concerns.18,19 A variety of non-conventional strategies including hyperbaric chambers, inhaled nitric oxide, high frequency jet ventilation and extracorporeal membrane oxygenation (ECMO) have been tried with varying success. The prognosis for pulmonary function in survivors is generally excellent.20
THE ABDOMEN
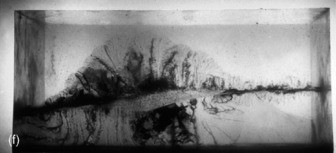
The hollow viscera are at risk of primary blast injury, particularly in cases of immersion blast. Isolated PBI to the gut is unusual in air blast, and generally occurs in the presence of severe secondary and tertiary injuries. At high overpressures, immediate rupture of the gut wall occurs with bleeding and spillage of intraluminal contents into the peritoneal cavity. More commonly, and at lower overpressures, haemorrhage develops within the intestinal wall, ranging from small petechiae to confluent haematomas. These lesions are characterised by varying degrees of vascular damage and thus some will progress to necrosis of the gut wall and late perforation.21
With large numbers of casualties, surgical triage is difficult. Data derived from a pig model provide some guidance as to those contusions at greater risk of late perforation.22 Bowel contusions > 15 mm diameter and colonic contusions > 20 mm diameter were at higher risk and warranted resection; smaller lesions could be treated conservatively. Circumferential lesions and those on the antimesenteric border were also associated with greater evidence of microvascular damage and perforation risk. Subcapsular haematomas, lacerations of solid organs, testicular rupture and retroperitoneal haematomas have all been described. These result from high blast loads and are likely to present early with abdominal signs and cardiovascular instability. In some patients the indications for exploratory laparotomy are obvious; in others PBI to the abdomen represents a diagnostic challenge, since it may be clinically silent until complications are advanced.
TRAUMATIC AMPUTATION
Common in mine injury, traumatic amputation is unusual in blast survivors. It is common in those who are killed immediately or die quickly.13 The amputations do not generally occur through joints.10 That situation is seen in ejecting fast jet pilots exposed to high wind speeds (1100 km/h). The common sites are the upper third of the tibia, and the upper or lower third of the femur. Computer modelling and evidence from isolated animal limb studies10 demonstrate that the blast wave generates stress concentrations at particular points in long bones, causing fractures before displacement occurs. Subsequently, blast wind-induced displacement removes the limb. The implication of this is that any survivors with traumatic amputation, not obviously due to fragment damage, must be regarded as at very high risk for PBI to the lungs and gut, even if not manifest immediately, and observed accordingly.
The surgical strategy is initially one of extensive debridement leaving only viable tissue. The resulting wound is loosely packed and allowed to drain, with planned secondary inspection and soft tissue closure after a few days.24 Bone stock is preserved with the intention that a myoplastic stump can be organised at a later date, but the surgeon must acknowledge that this may be the final stump.25 The vascular damage which occurs under these circumstances is severe, and heroic efforts to revascularise partially amputated limbs may be counterproductive; any venous anastomosis attempted is likely to be precarious, and may jeopardise survival due to prolonged shock.
SPECIAL CIRCUMSTANCES
Under certain circumstances a relatively high incidence of PBI may be encountered, for example if casualties are protected from fatal secondary injury by personal body armour or environmental structures. Alternatively, an explosion in a confining space may produce exacerbation of the overpressure experienced by an individual, by summation of incident blast energy and that reflected from rigid surfaces. Casualties at a distance from the explosion normally considered safe (for primary effects) for a ‘free field’ blast, might experience an enhanced blast effect and be at risk for PBI; survivors may have a high incidence of PBI. This has been well described for terrorist bombs in buses26 and more recently trains.27
Conventional military devices exert their anti-personnel effects by secondary and tertiary action. Fuel-air weapons function by delivering a cloud of fuel vapour over or around a target which, once optimally mixed with air, is then detonated. These devices have a very low integral fragment load, but have an enhanced blast effect experienced throughout the fuel cloud that may cover a wide area; the thermal output is also substantial. Originally designed to assist in mine clearance, these weapons are ideal for attacking enemy troops in trenches or built-up areas.28 The development of these weapons was initially difficult, but most of the technical problems have been overcome, and new generations have appeared. Such devices are reported to have been deployed in recent conflicts, and are available in air-delivered, artillery, tank-mounted and shoulder-launched variants. Now fairly widely available, this class of enhanced blast effect weapon is likely to become an increasing threat. Individuals caught in the centre of the vapour cloud are unlikely to survive, but people at the margins can be predicted to have a high incidence of PBI, significant burns and injuries associated with collapse of buildings.
SECONDARY BLAST INJURY
Surgical strategy hinges around the identification and removal of large pieces of foreign material, or those associated with, or likely to cause, neurovascular compromise.29 Systematic removal of all minute fragments may cause more tissue destruction than might otherwise have occurred.30,31
Modern anti-personnel munitions (grenades, mortar rounds) are designed to incapacitate or kill by delivering high-energy small fragments into the target. Such weapons have caused the majority of wounds to military personnel in recent conflicts.32 Preformed fragments often have a mass of 0.1–0.2 g and an initial velocity of ∼1500 m/s. Because of irregular shape, velocity falls rapidly, but penetration can still occur at substantial distances. Soldiers in field conditions wear clothes contaminated with soil (and Clostridia spp.), and the skin is covered with faecal organisms and pyogenic Streptococci and Staphylococci spp.33 High-energy fragments produce temporary cavities (see below) with negative intracavity pressure. Small fragments shred clothing and contaminated clothing fibres are driven or drawn into the wound. Wounds characterised by cavitation will have contamination distributed throughout a greater volume of tissue than might have been anticipated, or exhibited by lower energy wounds. The benefit of the early administration of antibiotics to prevent or retard the development of infection is well established.
Many of these wounds are to the limbs and these are small and multiple. The orthodox operative doctrine was derived from experiences in World War I where large fragments produced the majority of wounds. Newer weapons producing smaller wounds have caused a re-examination of this philosophy; selected wounds may be managed conservatively with cleansing, closed fracture management, antibiotics and observation, and criteria (Table 77.4) have been published.34–36
Table 77.4 Factors to be considered in the management of small fragment wounds
| Risk factors for infection34 | Criteria where non-operative management may be appropriate30,35,36 |
|---|---|
| Prolonged time between wounding and presentation for treatment | Entry/exit wound < 1 cm |
| No evidence of permanent cavitation within the wound | |
| Lack of prior wound cleansing | |
| Wound size > 1 cm | No neurovascular compromise |
| Failure to comply with wound care instructions | No compartment syndrome |
| Low to medium energy transfer fractures | Stable fracture pattern |
| No signs of infection | |
| Have been treated early with dressings and antibiotics |
High-energy fragments can produce fractures, and can penetrate the body wall and injure the lungs or visceral structures. As the body wall is penetrated, the fragment energy is significantly reduced so that in survivors reaching hospital intracavity damage will tend to be localised.31 Thus, mesenteric and gut perforations tend to be small and discrete. Small bowel wounds can generally be repaired primarily; the management of large bowel wounds remains controversial. There is an increasing enthusiasm for primary resection and repair with or without proximal diversion.37 The pursuit of small fragments, which have transited the colon into the retroperitoneal tissues, may be counterproductive.38
Recent reports after terrorist incidents have highlighted that biological material from fellow victims, or even suicide bombers, may penetrate casualties and present a risk of viral transmission,39 thus vaccination or post-exposure prophylaxis should be considered.
QUATERNARY BLAST INJURY
This classification includes injuries not otherwise classified, and includes superficial flash burns and crush injury from collapsing buildings. Depending on the exact explosives and physical circumstances, burn injuries may impose a substantial challenge, the combination of burns plus secondary injuries posing a very substantial infection risk.40,41
MINES
It has been estimated that around 100 million anti-personnel mines are currently in the ground worldwide and a further 250 million are stockpiled. A mine explodes every 20 minutes, injuring or killing approximately 26 000 people per year, most commonly children and agricultural workers. Many of these people die before reaching medical assistance42 (Table 77.5).
| Activation | Injury pattern | |
|---|---|---|
| Pattern 1 | Mine stepped on | Severe lower limb, perineal and genital injuries |
| Pattern 2 | Device explodes near victim: activated by other victim or an above-ground mine | Less severe lower extremity injuries; injuries to head, chest and abdomen common |
| Pattern 3 | Handling injury | Severe facial and upper limb injury |
An anti-personnel mine is designed to incapacitate and maim rather than to kill – an exception being trip- or command-wire detonated above ground mines (e.g. ‘Claymore’ mines). A small quantity of explosive is detonated by pressure, and device fragments, soil and footwear remnants are forced upwards. The shock wave is concentrated in the tibia which fractures; the subsequent expansion of explosive products opens up tissue planes, causing substantial damage and contamination, and often completes the traumatic amputation. Limbs not amputated at first instance often require surgical amputation due to overwhelming soft-tissue damage. Damage to the contralateral limb is likely to be less severe, but meticulous attention must be paid to avoid complications leading to a second amputation. In addition, up to 5% of casualties suffer ocular injuries, and this figure is higher for handling injuries and above ground mines. Injuries to the perineum, the external genitalia and the rectum are all common. Many patients will require laparotomy for penetrating trauma.43,44
The wounds are heavily contaminated with soil organisms. The surgical strategy consists of:
Primary closure of wounds45 and heroic limb salvage for limited posterior foot injuries46 have been reported. Complication rates are likely to be high under all but the most ideal circumstances, and the expertise and facilities required to attempt this approach safely are not available to the vast majority of those injured.
GUNSHOT WOUNDS
Small arms ammunition can be divided broadly into two types: rifle rounds, which are supersonic, and subsonic handgun or submachine gun rounds. This leads to a superficially attractive classification of gunshot wounds (GSW) into high- or low-velocity wounds. This has now been superseded with the realisation that energy transfer is the important factor. The kinetic energy available is governed by the equation:
PATHOLOGY AND MANAGEMENT OF GUNSHOT WOUNDS
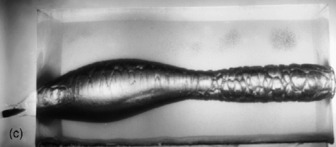
The phenomenon of temporary cavitation is generally a feature of high-velocity rounds.47 The bullet penetrating a casualty is preceded by a shock wave which forces tissue away from its path, producing a temporary cavity, the diameter of which is many times that of the projectile itself (Figure 77.1). The cavity is instantly under negative pressure which draws environmental debris, clothing fragments and resident skin organisms into the casualty, via the entry wound. In addition, the tissue forming the walls and margins of the cavity is damaged and devitalised, forming a substrate for infection with the inoculating organisms. Shock wave and cavitation effects may be responsible for fractures not directly involved with the wound track.47–49 Skeletal muscle is fairly elastic and tolerates cavitation reasonably well, whereas organs constrained by inelastic capsules or bony structures, such as the liver and brain, fare very badly.
Rounds may yaw and tumble prior to or after impact, leading to an unpredictable path through the victim; this is a particular feature of bullets from high-velocity smaller calibre rifles, known as assault rifles. Such injuries commonly involve more than one body cavity. Thus, extensive radiological studies must be performed prior to surgical exploration if at all possible. Occasionally, minute fragments of radio-opaque bullet debris may mark the path of the wound track.50 The presence or absence, and size of any exit wound are an imperfect guide to the magnitude of wound trauma.47 The behaviour of bullets is unpredictable, and attempting to predict this from knowledge of the weapon and firing distance may produce a misleading treatment plan.
The severity of fractures produced by direct impact on bone is governed largely by energy transfer. High-energy weapons such as military and hunting rifles produce fractures with a high degree of comminution, whereas the majority of ballistic fractures due to handguns are minimally fragmented.51,52
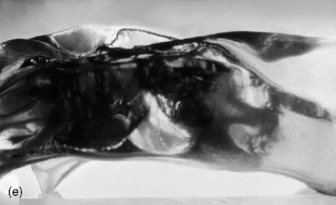
Gunshot wounds become infected quickly due to the effects outlined above. Military surgical doctrine is for extensive wide local excision and delayed primary closure of limb wounds (Figure 77.2). This strategy evolved from conflicts during which both time of wounding to time of surgery intervals were long, and contamination with coliforms and soil organisms was likely. In civilian practice the wounding to treatment interval is usually short, and a less mutilating surgical strategy can sometimes be adopted.53 Under certain circumstances upper limb wounds can be treated on an outpatient basis, with suitable wound cleansing, immobilisation and perhaps an antibiotic prescription.54–56



Both Figure 77.1 and 77.2 courtesy of Professor Jim Ryan, Leonard Cheshire Professor of Conflict Recovery, University College, London.
The majority of casualties surviving to hospital admission will require surgical exploration. The degree of debridement required will be governed by the operative findings and anatomy, rather than assumptions derived from knowledge of the weapon. Under certain circumstances, and with haemodynamically stable patients, penetrating abdominal wounds may be evaluated laparoscopically, potentially avoiding a negative laparotomy.57,58
ANTIBIOTIC CONSIDERATIONS
The combination of a wound, devitalised tissue and foreign material is ideal for the development of infection. Whether or not an infection develops depends on the quantity of bacteria and foreign material inoculated, and the time interval during which the bacteria can divide prior to wound irrigation, surgery or antibiotic administration.59,60 Antibiotics can lengthen the safe period prior to establishment of infection if surgery is to be delayed.61 The mainstay of treatment is surgery but during conflict this may not be available immediately and thus early dressing and antibiotics have an important role. As Clostridia spp. and β-haemolytic Streptococci have caused the majority of infective complications of war wounds, simple benzyl penicillin has been the most valuable first-line prophylactic and therapeutic agent, with strong evidence to support its continued use.33,59 Ballistic fractures carry a significant risk of staphylococcal osteomyelitis and require flucloxacillin. In civilian circumstances the bacterial inoculum is orders of magnitude less. Thus, for simple limb gunshot wounds, if there is minimal inoculated material and the wound is attended to early, a far weaker argument for prophylactic use exists. The optimum duration of postoperative prophylaxis remains unclear;59 evidence exists that even for penetrating hollow viscus injury, a short course may be adequate.62
1 Kluger Y, Peleg K, Daniel-Aharonson L, et al. The special injury pattern in terrorist bombings. J Am Coll Surg. 2004;199:875-879.
2 Arnold JL, Halpern P, Tsai MC, et al. Mass casualty terrorist bombings: a comparison of outcomes by bombing types. Ann Emerg Med. 2004;43:263-273.
3 Shamir MY, Rivkind A, Weissman C, et al. Conventional terrorist bomb incidents and the intensive care unit. Curr Opin Crit Care. 2005;11:580-584.
4 Almogy G, Mintz Y, Zamir G, et al. Suicide bombing attacks: can external signs predict internal injuries? Ann Surg. 2006;243:541-546.
5 Cullis IG. Blast waves and how they interact with structures. J R Army Med Corps. 2001;147:16-26.
6 Zuckerman S. Experimental study of blast injury to the lungs. Lancet. 1940;2:219-224.
7 Krohn PL, Whitteridge D, Zuckerman S. Physiological effects of blast. Lancet. 1942;1:252-258.
8 Horrocks CL. Blast injuries: biophysics, pathophysiology and management principles. J R Army Med Corps. 2001;147:28-40.
9 Guy RJ, Kirkman E, Watkins PE, et al. Physiologic responses to primary blast. J Trauma. 1998;45:983-987.
10 Hull JB, Cooper GJ. Pattern and mechanism of traumatic amputation by explosive blast. J Trauma. 1996;40:S198-205.
11 Hull JB, Bowyer GW, Cooper GJ, et al. Pattern of injury in those dying from traumatic amputation caused by bomb blast. Br J Surg. 1994;81:1132-1135.
12 Brismar B, Bergenwald L. The terrorist bomb explosion in Bologna, Italy, 1980: an analysis of the effects and injuries sustained. J Trauma. 1982;22:216-220.
13 Mellor SG, Cooper GJ. Analysis of 828 servicemen killed or injured by explosion in Northern Ireland 1970–84: the Hostile Action Casualty System. Br J Surg. 1989;76:1006-1010.
14 Tsokos M, Paulsen F, Petri S, et al. Histologic, immunohistochemical and ultrastructural findings in human blast lung injury. Am J Respir Crit Care Med. 2003;168:549-555.
15 Schild HH, Strunk H, Weber W, et al. Pulmonary contusion: CT vs plain radiograms. J Comput Assist Tomogr. 1989;13:417-420.
16 Wagner RB, Jamieson PM. Pulmonary contusion. Evaluation and classification by computed tomography. Surg Clin North Am. 1989;69:31-40.
17 Keren A, Stessman J, Tzivoni D. Acute myocardial infarction caused by blast injury of the chest. Br Heart J. 1981;46:455-457.
18 Sorkine P, Szold O, Kluger Y, et al. Permissive hypercapnia ventilation in patients with severe pulmonary blast trauma. J Trauma. 1998;45:35-38.
19 Avidan V, Hersch M, Armon Y, et al. Blast lung injury: clinical manifestations, treatment and outcome. Am J Surg. 2005;190:945-950.
20 Hirshberg B, Oppenheim-Eden A, Pizov R, et al. Recovery from blast lung injury: one-year follow-up. Chest. 1999;116:1683-1688.
21 Cripps NPJ, Cooper GJ. Intestinal injury mechanisms after blunt abdominal impact. Ann R Coll Surg Engl. 1997;79:115-120.
22 Cripps NPJ, Cooper GJ. Risk of late perforation in intestinal contusions caused by explosive blast. Br J Surg. 1997;84:1298-1303.
23 Garth RJ. Blast injury of the ear: an overview and guide to management. Injury. 1995;26:363-366.
24 Covey DC, Lurate RB, Hatton CT. Field hospital treatment of blast wounds of the musculoskeletal system during the Yugoslav civil war. J Orthop Trauma. 2000;14:278-286.
25 Coupland RM. Amputation for antipersonnel mine injuries of the leg: preservation of the tibial stump using a medial gastrocnemius myoplasty. Ann R Coll Surg Engl. 1989;71:405-408.
26 Pizov R, Oppenheim-Eden A, Matot I, et al. Blast lung injury from an explosion on a civilian bus. Chest. 1999;115:165-172.
27 De Ceballos JP, Turegano-Fuentes F, Perez-Diaz D, et al. 11 March 2004: The terrorist bomb explosions in Madrid, Spain – analysis of the logistics, injuries sustained and clinical management of casualties treated at the closest hospital. Crit Care. 2005;9:104-111.
28 Demonstration of fuel-air weapon available at: http://www.nawcwpns.navy.mil/clmf/faeseq.html
29 Hill PF, Edwards DP, Bowyer GW. Small fragment wounds: biophysics, pathophysiology and principles of management. J R Army Med Corps. 2001;147:41-51.
30 Coupland RM. Hand grenade injuries among civilians. JAMA. 1993;270:624-626.
31 Bowyer GW. Management of small fragment wounds: experience from the Afghan border. J Trauma. 1996;40:S170-72.
32 Patel TH, Wenner KA, Price SA, et al. A US Army forward surgical team’s experience in Operation Iraqi Freedom. J Trauma. 2004;57:201-207.
33 Mellor SG, Easmon CSF, Sanford JP. Wound contamination and antibiotics. In: Ryan JM, Rich NM, Dale RF, et al, editors. Ballistic Trauma. London: Edward Arnold; 1997:61-71.
34 Ordog GJ, Sheppard GF, Wasserberger JS, et al. Infection in minor gunshot wounds. J Trauma. 1993;34:358-365.
35 Ordog GJ, Wasserberger J, Balasubramanium S, et al. Civilian gunshot wounds – outpatient management. J Trauma. 1994;36:106-111.
36 Bowyer GW. Management of small fragment wounds in modern warfare: a return to Hunterian principles? Ann R Coll Surg Engl. 1997;79:175-182.
37 Gonzalez RP, Falimirski ME, Holevar MR. Further evaluation of colostomy in penetrating colon injury. Am Surg. 2000;66:342-346. discussion 346–7
38 Edwards DP, Brown D, Watkins PE. Should colon-penetrating small missiles be removed? An experimental study of retrocolic wound tracks. J Invest Surg. 1999;12:25-29.
39 Wong JM, Marsh D, Abu-Sitta G, et al. Biological foreign body implantation in victims of the London July 7th suicide bombings. J Trauma. 2006;60:402-404.
40 Kennedy PJ, Haertsch PA, Maitz PK. The Bali burn disaster: implications and lessons learned. J Burn Care Rehab. 2005;26:125-131.
41 Silla RC, Fong J, Wright J, et al. Infection in acute burn wounds following the Bali bombings: a comparative prospective audit. Burns. 2006;32:139-144.
42 Coupland RM, Korver A. Injuries from antipersonnel mines: the experience of the International Committee of the Red Cross. BMJ. 1991;303:1509-1512.
43 Bilukha OO, Brennan M, Woodruff BA. Death and injury from landmines and unexploded ordnance in Afghanistan. JAMA. 2003;290:650-653.
44 Centers for Disease Control. Injuries associated with landmines and unexploded ordnance – Afghanistan, 1997–2002. CDC MMWR. 2003;52:859-862.
45 Atesalp AS, Erler K, Gur E, et al. Below-knee amputations as a result of land-mine injuries: comparison of primary closure versus delayed primary closure. J Trauma. 1999;47:724-727.
46 Selmanpakoglu N, Guler M, Sengezer M, et al. Reconstruction of foot defects due to mine explosion using muscle flaps. Microsurgery. 1998;18:182-188.
47 Cooper GJ, Ryan JM. Interaction of penetrating missiles with tissues: some common misapprehensions and implications for wound management. Br J Surg. 1990;77:606-610.
48 Clasper JC, Hill PF, Watkins PE. Contamination of ballistic fractures: an in vitro model. Injury. 2002;33:157-160.
49 Hill PF, Clasper JC, Parker SJ, et al. Early intramedullary nailing in an animal model of a heavily contaminated fracture of the tibia. J Orthop Res. 2002;20:648-653.
50 Ragsdale BD, Sohn SS. Comparison of the terminal ballistics of full metal jacket 7.62-mm M80 (NATO) and 5.56-mm M193 military bullets: a study in ordnance gelatin. J Forensic Sci. 1988;33:676-696.
51 Ragsdale BD, Josselson A. Experimental gunshot fractures. J Trauma. 1988;28:S109-15.
52 Rose SC, Fujisaki CK, Moore EE. Incomplete fractures associated with penetrating trauma: etiology, appearance, and natural history. J Trauma. 1988;28:106-109.
53 Bowyer GW, Rossiter ND. Management of gunshot wounds of the limbs. J Bone Joint Surg Br. 1997;79:1031-1036.
54 Knapp TP, Patzakis MJ, Lee J, et al. Comparison of intravenous and oral antibiotic therapy in the treatment of fractures caused by low-velocity gunshots. A prospective, randomized study of infection rates. J Bone Joint Surg Am. 1996;78:1167-1171.
55 Dickson K, Watson TS, Haddad C, et al. Outpatient management of low-velocity gunshot-induced fractures. Orthopedics. 2001;24:951-954.
56 Byrne A, Curran P. Necessity breeds invention: a study of outpatient management of low velocity gunshot wounds. Emerg Med J. 2006;23:376-378.
57 Miles EJ, Dunn E, Howard D, et al. The role of laparoscopy in penetrating abdominal trauma. JSLS. 2004;8:304-309.
58 Ahmed N, Whelan J, Brownlee J, et al. The contribution of laparoscopy in evaluation of penetrating abdominal wounds. J Am Coll Surg. 201, 2005.
59 Zimmerli W, Waldvogel FA, Vaudaux P, et al. Pathogenesis of foreign body infection: description and characteristics of an animal model. J Infect Dis. 1982;146:487-497.
60 Simpson BW, Wilson RH, Grant RE. Antibiotic therapy in gunshot wound injuries. Clin Orthop Relat Res. 2003;408:82-85.
61 Mellor SG, Cooper GJ, Bowyer GW. Efficacy of delayed administration of benzylpenicillin in the control of infection in penetrating soft tissue injuries in war. J Trauma. 1996;40:S128-134.
62 Kirton OC, O’Neill PA, Kestner M, et al. Perioperative antibiotic use in high-risk penetrating hollow viscus injury: a prospective trial of 24 hours versus 5 days. J Trauma. 2000;49:822-832.