CHAPTER 13 BLAST INJURIES
Blast injury is unique in that it combines the mechanisms of several categories of injury, including blunt, penetrating, and thermal. This results in a wide range of overt and occult injury patterns making the diagnosis and treatment of specific injuries difficult.1 However, like most problems in medicine, a basic knowledge of and methodical approach to the problem can save lives. The use of explosives can be traced to the use of black powder by the Chinese in the 10th century. In the 1800s other explosive substances were invented, including nitroglycerin, trinitrotoluene (TNT), and dynamite. Explosives have been used in every major conflict by the United States since the American Revolution. Blast injury was first described in World War I and at that time was primarily thought to involve the lung. In World War II, blast injury to the bowel was seen due to an increase in casualties of underwater explosions. The treatment of blast injury advanced during the Korean War. In Vietnam, blast injuries were seen, but the predominant injuries were due to high-velocity gunshot wounds.2,3
The Israelis had the greatest experience with blast injury during the latter quarter of the 20th century, and have reported extensively on the subject.4 Examples of recent domestic terrorist attacks that resulted in significant destruction and casualties include the 1993 bombing of the World Trade Center, the 1995 bombing of the Alfred P. Murrah Federal Building in Oklahoma City, and the bombing of the Centennial Park in Atlanta (1996).5,6 Many casualties of the September 11, 2001 attacks occurred as result of blast effect and structural collapse.7
The use of improvised explosive devices (IEDs) by insurgents has become the predominant weapon against coalition troops in Iraq. A recent article reviewed the injuries of wounded soldiers returning to Walter Reed Army Medical Center from March to July 2003. Of 294 casualties seen, 31% sustained blast injuries.8 Another study focused on 18 blast-injured patients evaluated at a forward resuscitative surgical hospital. A significant proportion of these casualties presented with penetrating head injuries, severe lung injuries, and multiple open fractures. This study characterizes the lethal effects of blast.1
MECHANISMS OF INJURY AND INJURY PATTERNS IN EXPLOSIONS
Explosions produce specific injury patterns and the potential to cause life-threatening multisystem or multidimensional injuries. These patterns are the result of the composition and type of bomb, the delivery method, the distance between the victim and the blast, whether the blast occurred in a closed or open space2 and surrounding environmental barriers or hazards. Blast injury is a general term that refers to the biophysical and pathophysiological events and the clinical syndromes that occur when a living body is exposed to blast of any origin. Explosions are caused by a rapid chemical conversion of a solid or liquid into a gas with resultant energy release. Explosives are either high or low order. High-order explosives are designed to detonate quickly, generate heat and loud noise, fill the space with high-pressure gases in 1/1000th second, and produce a supersonic overpressurization shock (the increased pressure above normal atmospheric pressure from a blast) that expands from the point of detonation outward in a pressure pulse. The level of overpressure depends on the following: (1) the energy of the explosion, (2) the distance from the point of detonation, (3) the elapsed time since the explosion, and (4) the measurement technique. Blast strength is described as the ratio of overpressure to ambient pressure. The blast wave (positive wave) moves in all directions away form the explosion, exerting pressures of up to 700 tons (Figure 1). Shock waves possess the quality of brisance (shattering effect). The displaced air then compresses and forms a vacuum returning to the point of detonation (negative wave). The negative phase is not considered to result in blast injury. High-order explosives include TNT, C-4, Semtex, nitroglycerin, dynamite, and ammonium nitrate fuel oil. Low-order explosives produce a subsonic explosion without overpressurization wave. Energy is released slowly and burns by a process of deflagration. Low-order explosives include pipe bombs, gun powder, Molotov cocktails, and pure petroleum-based bombs. Explosives have several effects: the blast pressure wave as described previously, the fragmentation effect, the blast wind, the incendiary thermal effect, secondary blast pressure effects, and ground and water shocks for explosions that occur below ground or water.9
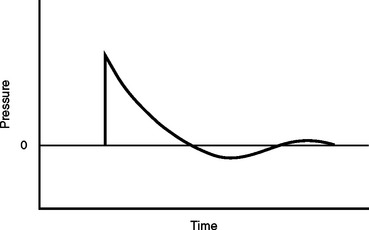
Figure 1 Propagation of blast wave over time.
(Data from Jensen JH, Bonding P: Experimental pressure induced rupture of the tympanic membrane in man. Acta Otolaryngol 113:62–67, 1993.)
Fragmentation effect occurs from projectiles included in the container, projectiles produced from the destruction of the container, and from objects surrounding the detonator and target. These projectiles can travel up to 2700 feet per second. The blast wind is created by the motion of air molecules responding to pressure differentials generated by the blast. These winds may be as high as those seen in hurricanes but are not sustained. The incendiary thermal effect is different for high- and low-order explosives. High-order explosives produce higher temperatures for shorter periods of time, usually resulting in a fireball at the time of the detonation. Low-order explosives have a longer thermal effect and cause secondary fires. Secondary blast pressure effects are caused by the blast wave’s reflection off surfaces prolonging and magnifying the effect, particularly in enclosed spaces. Greater transfer of energy to the body occurs. Underground and underwater explosions propagate the shock waves farther and with more force than air.10
Bombs are weapons and defined as any container filled with explosive material whose explosion is triggered by a clock or other timing device. Terrorist bombs, IEDs, are usually custom-made, may use a number of designs or explosives, and are of two types: conventional (filled with chemical explosives containing the compounds of hydrogen, oxygen, nitrogen, and carbon) or dispersives (filled withchemical or other projectiles such as nails, steel pellets, screws, and nuts) designed to disperse. Nuclear devices rely on nuclear fission or fusion. Explosions can produce unique patterns of injury. They have the potential to inflict multisystem life-threatening injuries on many persons simultaneously. The injury patterns following such events are a product of the composition and amount of the materials involved, the surrounding environment, and the delivery method, the distance between the victim the blast, and any intervening protective barriers or environmental hazards. Because explosions are relatively infrequent, blast-related injuries can present unique triage, diagnostic, and management challenges to providers or emergency care personnel.11
BLAST INJURY: CLINICAL ASPECTS
Blast-related injuries are now very common and have become a threat for populations all over the world. Powerful explosions that result in different tissue and air interactions have the potential to inflict complex and unique injuries. Severely injured patients from explosions often sustain combined blunt, penetrating, and burn injuries.12 Therefore, knowledge of the mechanisms of blast effect and early recognition of the potential injuries are of paramount importance in the management of blast-injured patients. The injury patterns vary depending on setting (open or closed space), amount of explosive, and chemical properties of the explosive.13 Explosions in confined spaces are significantly more deadly and associated with high incidence of primary blast injuries than those in open air. Improvised explosive devices are accompanied by heavy shrapnel that result in various injury patterns involving more body regions and increase severity. This makes management of blast injuries more challenging.4 According to their underlying mechanisms, blast injury is classified into four categories: primary, secondary, tertiary, and quaternary (Table 1).14 Quinary blast injury also has recently been described.
| Type of Blast Injury | Features |
|---|---|
| Primary | Caused by barotrauma |
| Affects gas-filled structures including tympanic membrane, lungs, bowel | |
| Secondary | Caused by flying debris and fragments |
| Responsible for most of casualties | |
| Causes multiple injuries | |
| Tertiary | Caused by collapse and fragmentation of buildings |
| Causes severe fractures and amputations | |
| Quaternary | Includes all explosion-related injuries |
| Affected by patient’s premorbidities | |
| Quinary | Hyperinflammatory state |
| Toxins in explosives |
Primary Blast Injury
Primary blast injury causes barotrauma. The organs most vulnerable to primary blast injury are the gas-filled, namely the ear, lung, and gastrointestinal tract. The eardrum, the most frequently injured structure, may rupture at pressure as low as 2 psi (pounds/square inch).15 High overpressure may cause more significant injury to the ear such as dislocation and fracture of the ossicles of the middle ear, cochlear damage, and traumatic disruption of the oval or round window and subsequent permanent hearing loss.
The most common manifestations of ear blast injury are tinnitus, deafness, and vertigo. The fact that tympanic membrane injury occurs at low pressure and much more pressure is needed to damage other structures make tympanic membrane perforation an indicator of blast injury.
The anatomical structure of the lungs is characterized by large surface area with low tensile strength. This makes the lung very susceptible to primary blast injury, and injury to the lung may be the most fatal. The incidence of blast lung injury is unknown. In a study by Brismar and Bergenwald,16 8.4% of patients admitted after a blast were diagnosed with lung injury. Hadden et al.17 in a study from Northern Ireland reported that only 2 of 250 admitted patients (0.8%) suffered from primary blast lung injury; on the other hand, histopathologic evidence consistent with primary blast lung injury was found in 45% of the victims who died at the scene. A high proportion of primary blast lung injury occurs in explosions in enclosed space. In a study of 55 survivors after a terrorist bus bombing, Katz et al.18 found that 38% of patients had primary blast lung injury. Primary blast lung injury occurs at air pressure of 1100 kpcal (kilopascals) (Figure 2). The pressure differentials disrupt the alveolar walls and the alveolar-capillary membrane, and damage airway epithelium, producing a stripped-epithelium lesion. This results when bronchiolar epithelium is stripped from the basal membrane.19 As a result of these widespread structural disturbances, hemorrhage, pulmonary contusion, pneumothorax, hemothorax, pneumomediastinum, and subcutaneous emphysema can occur. Intrapulmonary hemorrhage and edema are major factors in the development of initial respiratory insufficiency from primary blast lung injury.20 Some experience apnea, bradycardia, and hypotension as immediate responses to blast injury of the lung. The diagnosis of primary blast lung injury is based on clinical manifestations, such as dyspnea, hypoxia, and hemoptysis. A chest x-ray may show the characteristic bihilar “butterfly” pattern representing underlying pulmonary contusion.21,22 A tear that may occur between the alveoli and the wall of the venule can create alveolo-venous fistulae, the major prerequisite for another life-threatening condition—arterial air embolism. This is a principal cause of early mortality.18
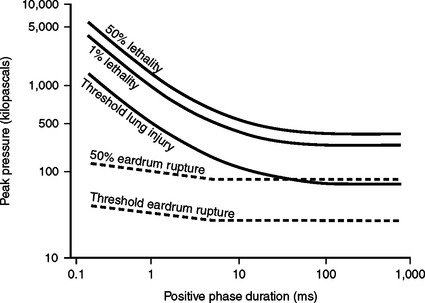
Figure 2 Tolerance and lethality of blast wave.
(Data from Jensen JH, Bonding P: Experimental pressure induced rupture of the tympanic membrane in man. Acta Otolaryngol 113:62–67, 1993.)
The blast lung severity score was introduced to estimate the severity of blast lung injury. The score is based on hypoxemia (PO2/FiO2 ratio), chest x-ray abnormalities, and presence of bronchopleural fistulae or pnemothorax. Severe blast lung injury is defined as a PO2/FiO2 ratio of less than 60 mm Hg, bilateral lung infiltrates, and bronchopleural fistulae, moderate as a PO2/FiO2 ratio of 60–200 mm Hg, diffuse lung infiltrates with or without pneumothorax; and mild blast lung injury as a PO2/FiO2 ratio of more than 200 mm Hg, localized lung infiltrates, and no pneumothorax.23 Pizov et al.20 studied 15 survivors of a bus explosion diagnosed with blast lung injury. Ten patients were intubated for respiratory failure within 2 hours after the explosion. Six patients with a moderate blast lung injury severity score required mechanical ventilation. Four patients who sustained severe lung injuries were managed with positive pressure ventilation immediately after the event. Out of the four with blast injury to the lung, three died. In conclusion, primary blast lung injury is life-threatening. The treatment of blast lung injury is challenging. Symptoms can manifest early resulting in immediate onset of pulmonary dysfunction, or the patient may have a less dramatic course of pulmonary insufficiency developing several days after the explosion.
Exposure to extreme blast overpressure may produce injury to the abdominal viscera. The colon is the organ most commonly affected by primary blast injury. Intestinal damage may present as free bowel perforation, hemorrhage, serosal hematoma, and mesenteric shear injuries. Intestinal perforation may occur immediately after blast exposure or develop as a result of mesenteric ischemia, infarct, and bowel contusion in hours to days after the event.17,21 Insidious manifestations of symptoms and the presence additional life-threatening injuries make abdominal injury difficult to recognize. Blast abdominal injury should not be overlooked in patients with abdominal pain, nausea, vomiting, and hematemesis. Lacerations and hemorrhage of solid organs such as liver, kidney, and spleen may occur with powerful explosions. Other injuries caused by primary blast effect include facial fractures, brain concussion, cerebral air embolism, and eye trauma. Traumatic limb amputations from blast phenomena are a hallmark of severe blast injury.24 The blast waves run along the long bones, creating a powerful shearing force. The long bones fracture into multiple fragments and then soft tissue is avulsed by the primary blast wave.25 Mellor et al.26 reported on 52 victims who sustained traumatic limb amputations, of whom only nine survived.
Secondary Blast Injury
Secondary blast injuries are caused by flying debris, and bomb fragments penetrating multiple body regions are responsible for a great proportion of casualties. Mallonee and colleagues27 studied the Murrah Building explosion in Oklahoma City, and reported that most common injuries were penetrating injuries to the extremities (74%), head and neck (48%), face (45%), and chest (35%). Penetrating injuries from fragments of the weapon and debris are the leading cause of death and injury. Suicide bombs used by terrorists contain large amounts of metal objects. It has been shown that missiles with irregular shapes have inherent ballistic instability and tend to have greater kinetic energy, causing more severe tissue destruction than symmetric missiles.28 These factors explain why multiple body regions are involved in a large number of casualties.
Tertiary Blast Injury
Tertiary blast injuries are caused by collapse and fragmentation of buildings, vehicles, and other objects. The collapse of buildings and other structures is characterized a large number of casualties and carries a high fatality rate. During the terrorist bombing of the Murrah Building in Oklahoma City, 88% of 361 people who were inside the building were injured. People located at the sites of structural collapse were significantly more likely to die (153/175, 87%) than those in the noncollapsed region of the building (10/186, 5%). Survivors who were located in the collapsed region of the building were significantly more likely to require hospitalization (82%), than those in the noncollapsed area. Collapse and fragmentation of these structures cause a wide range of blunt trauma injuries, multiple penetrating injuries, and crush syndrome.5
Tertiary blast injuries can also occur when the victims themselves become airborne by the blast wave and collide with nearby objects. These blast victims usually are very close to the explosion source and therefore sustain multiple injuries. Any body part may be affected and open fractures, traumatic limb amputations, and brain injuries may occur.29
Quaternary Blast Injury
Quaternary blast injuries may affect any part of the body and include all explosion-related injuries and conditions not due to primary, secondary, and tertiary blast effects. Quaternary blast injuries include burns, inhalation lung injury, and asphyxia caused by inhalation of incomplete combustion of explosion materials (e.g., carbon monoxide, cyanide), toxic dust, gas, and radiation exposure. Quaternary blast injury may involve exacerbation of chronic disease (including asthma, diabetes, hypertension, coronary artery disease, mental health issues, and substance abuse) as well as new behavioral problems. Materials used in incendiary bombs can cause severe burns. Burns sustained by victims of confined-space explosions affect a larger body surface area than those of open-space explosions.24
Quinary Blast Injury
A fifth category of blast injury has recently been described in blast injury victims. It occurs commonly after attack with incendiary devices. This type of blast injury is characterized by a “hyperinflammatory state” similar to systemic inflammatory response syndrome. This hyperinflammatory state cannot be explained by injuries that result from the other types of blast injury.4 Some clinicians hypothesize that quinary blast injury is due to toxic substances that are liberated by explosives which are inhaled or absorbed by skin and mucus membranes. Pentaerythritoltetranitrate (PETN), a vasodilator, is implicated as one such toxin. This form of blast injury is poorly understood but is increasingly identified in this cohort.30
Multidimensional Injury Pattern
The classical approach to managing blast injury patients has changed, and patients are now viewed as having a “multidimensional injury pattern.” This new concept was adopted largely from the experience of trauma surgeons treating victims of blast injury in Israel.30 The multidimensional injury pattern view relates different types of blast injury (primary, secondary, tertiary, etc.) with various mechanisms of injury (blunt, penetrating, thermal, radiation, etc.) and the organs injured (lung, ear, brain, gastrointestinal tract, etc.). Studies have shown that these types of injuries have higher morbidity and mortality when compared with non–blast-related trauma. The majority of these patients have multiple severe injuries and require management in an intensive care setting.4 The management of these patients requires a multidisciplinary approach, and can easily overwhelm local medical resources in a mass casualty situation.
TREATMENT OF BLAST INJURIES
The rate-limiting step in the management of blast injuries is the diagnosis of each specific injury, while treatment is straightforward. Patients found to have pneumothorax or hemothorax that result from a blast will often require chest tube thoracostomy. The presentation may be more subtle, and patients may present with subcutaneous emphysema, mediastinal air on chest radiograph, or delayed pneumothorax. Pulmonary contusion can be treated with supplemental oxygen and incentive spirometry; but patients with severe blast lung injury and hypoxemia need mechanical ventilation. The mode of ventilation should be tailored, and depends on the degree of hypoxia, presence of the bronchopleural fistulae, and injuries to the other organs. Generally, ventilation should use limited peak inspiratory pressure because of high risk of air embolism and pneumothorax. High-frequency ventilation provides adequate oxygenation with low airway pressure, and is recommended for ventilation of patients with bronchopleural fistulae.31
Clinical signs of arterial air embolism include air seen on retinoscopy, cardiac dysrhythmias or signs of ischemia, neurologic defects, livedo reticularis, and blanching tongue. Air emboli form when air escapes from a pulmonary laceration into the arterial tree. The treatment for air emboli is largely supportive. The patient should be monitored for signs of cerebral and cardiac ischemia. Hyperbaric oxygen therapy has been shown to be beneficial in animal studies, but its efficacy in humans has yet to be determined.12
Significant blast injury to the gastrointestinal tract will almost always require exploration. These injuries may be obvious on presentation or can be detected by CT scan or diagnostic peritoneal lavage. Bowel injuries resulting in perforation and extensive mesenteric and intramural hematomas will require resection. The amount of bowel destruction can be impressive.32 All blast injury victims should be screened for hearing loss. Debris and foreign material must be removed from the external auditory canal. Small to moderate perforations of the tympanic membrane should heal spontaneously. Large perforations may require patching or tympanoplasty.33
Explosions in closed spaces or that result in structural collapse have higher mortality and injury rates.9 Arnold and colleagues,34 in an epidemiological review of terrorist bombings that produced 30 or more casualties, found that 1 in 4 victims died immediately in structural collapse, 1 in 12 in confined-space bombings, and 1 in 25 in open-air bombings. Bus bombings in the Israeli experience resulted in the highest mortality rate.
There is a triphasic distribution of mortality related to blast injury: (1) high immediate mortality rate, (2) a low early emergency department mortality rate, and (3) a late (in-hospital) mortality rate. Injury patterns causing death can be classified as the following: complete disruption of bodies, 14%; multiple injuries, 39%; head and chest injuries, 21%; head injuries, 12%; and chest injuries, 11%. Hidden injuries such as air emboli and cardiac dysrhythmias may account for fatalities in which no other cause of death is found. Injury patterns are varied as well. Structural collapse victims sustained more inhalational and crush injuries (secondary, quaternary injuries) and fewer primary blast injuries. Confined-space bombings resulted in more primary and quaternary blast injuries, while open-air bombing led to higher rates of ballistic soft tissue injuries or more secondary blast injuries.35
1 Nelson TJ, Wall DB, Stedje-Larsen ET, et al. Predictors of mortality in close proximity blast injuries during Operation Iraqi Freedom. J Am Coll Surg. 2006;202:418-422.
2 H Oxendine The history of explosives. University of Vermont, Environmental Safety Website, January 13, 2000. Available at: www.esf.uvm.edu/sirippt/blast1/index.htm
3 E Thall: Explosives. Florida Community College at Jacksonville. Available at: www.mooni.fccj.org/∼ethall/explode/explode.htm
4 Kluger Y, Peleg K, Daniel-Aharonson L, et al. The special injury pattern in terrorists bombing. J Am Coll Surg. 2004;199(6):875-879.
5 Teague DC. Mass casualties in the Oklahoma City bombing. Clin Orthop Relat Res. 2004;422:78-81.
6 Felicano DV, Anderson GV, Rozycki GS, et al. Management of casualties from the bombing of the Centennial Olympics. Am J Surg. 1998;176:538-543.
7 Quenemoen LE, Davis YM, Malilay J, et al. The World Trade Center bombing: injury prevention strategies for high rise buildings. Disasters. 1996;20(2):125-132.
8 Montgomery SP, Swiecki CW, Shriver CD. The evaluation of casualties from Operation Iraqi Freedom to return to continental United States from March to June 2003. J Am Coll Surg. 2005;201:7-13.
9 Avidan V, Hersch M, Armon Y, et al. Blast lung injury: clinical manifestations, treatment and outcome. Am J Surg. 2005;190(6):927-931.
10 Arnold JL, Halpern P, Tsai MC, Smithline H. Mass casualty terrorist bombings: epidemiological outcomes, resource utilization and the time course of emergency needs. Prehosp Disaster Med. 2003;18(3):220-260. (review)
11 Lucci EB. Civilian preparedness and counter-terrorism: conventional weapons. Surg Clin N Am. 2006;86:579-600.
12 Stuhmiller JH, Phillips YY, Richmond DR. The physics and mechanisms of primary blast injury. In: Bellamy RF, Zajtchuk R, editors. Textbook of Military Medicine Part I. Conventional Warfare: Ballistic, Blast and Burn Injuries. Washington, DC: Office of the Surgeon General, 1989.
13 Horrocks CL. Blast injuries: biophysics, pathophysiology and management principles. J R Army Med Corps. 2001;147(1):28-40. (review)
14 Emergency War Surgery. In: Burris DG, Fitzhrans JB, Holcomb JB, et al, editors. The Third United States Revision. Washington, DC: Borden Institute, 2004.
15 Phillips YY. Primary blast injuries. Ann Emerg Med. 1986;15:1446-1450.
16 Brismar B, Bergenwald L. The terrorist bomb explosion in Bologna, Italy, 1980: an analysis of the effects and injuries sustained. J Trauma. 1982;22:216-220.
17 Hadden MA, Rutherford WH, Merrett JD. The injuries of terrorist bombing: a study of 1532 consecutive patients. Br J Surg. 1978;65:525-531.
18 Katz E, Ofek B, Adler J, et al. Primary blast injury after a bomb explosion in civilian bus. Ann Surg. 1989;209:484-488.
19 Brown R, Cooper G, Maynard R. The ultrastructure of rat lung following acute primary blast injury. Int J Exp Pathol. 1993;74:151-162.
20 Pizov R, Oppenheim-Eden A, Mator I, et al. Blast injury from explosion on a civilian bus. Chest. 1999;115:165-172.
21 Gutierrez de Ceballos JP, Fuentes FT, Diaz DP, et al. Casualties treated at the closest hospital in the Madrid, March 11, terrorist bombings. Crit Care Med. 2003;33:S107-S112.
22 de Candole CA. Blast injury. CMAJ. 1967;96:207-214.
23 Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir. Crit Care Med. 1994;149:818-824.
24 Leibovici D, Gofrit O, Stein M, et al. Blast injuries: bus versus open-air bombings—a comparative study of injuries in survivors of open-air versus confined-space explosions. J Trauma. 1996;41(6):1030-1035.
25 Hull JB. Traumatic amputation by explosive blast: pattern of injury in survivors. Br J Surg. 1992;79:1303-1306.
26 Mellor SG, Cooper GJ. Analysis of 828 servicemen killed or injured by explosion in Northern Ireland 1970–1984: the Hostile Action Casualty System. Br J Surg. 1989;77:1006-1010.
27 Mallonee S, Shariat S, Stenies G, et al. Physical injuries and fatalities resulting from the Oklahoma City bombing. JAMA. 1996;276:382-387.
28 Cooper GJ, Maynard RL, Cross NL. Casualties from terrorist bombing. J Orthop Trauma. 1983;23:955-967.
29 DePalma RG, Burris DG, Champion HR, et al. Blast injuries. N Engl J Med. 2005;352(13):1335-1342. (review)
30 Mayo A, Kluger Y. Terrorist bombing. World J Emerg Surg. 2006;1:33. Available at www.wjes.org/content/1/1/33
31 Wanek S, Mayberry JC. Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin. 2004;20(1):171-181. (review)
32 Sharma OP, Oswanski MF, White PW. Injuries to the colon from blast effect and penetrating extraperitoneal thoraco-abdominal trauma. Injury. 2004;35(3):320-324.
33 Cripps NP, Glover MA, Guy RJ. The pathophysiology of primary blast injury and its implications for treatment. Part II: The auditory structures and the abdomen. J R Nav Med Serv. 1999;85(1):13-24. (review)
34 JL Arnold, P Halpern & MC Tsai, et al: Mass casualty terrorist bombing: a comparison of outcomes by bombing type. Ann Emerg Med 43(2): 263–273
35 Jensen JH, Bonding P. Experimental pressure induced rupture of the tympanic membrane in man. Acta Otolaryngol. 1993;113:62-67.







