56 Bioterrorism and its impact on the PACU
Aerosolization: A gaseous suspension of organisms that contains minute particles.
CBRNE: Chemical, Biologic, Radiologic, Nuclear, Explosive event.
Cohort: Group together with similar likenesses.
Dirty Bomb: A mix of explosives, such as dynamite, with radioactive powder or pellets. The dynamite explodes and carries material into the surrounding area (e.g., radioactive material, biologic agents).
Empiric Treatment: Broad-based antibiotic treatment based on prior experience with the microorganism.
Sepsis: The body’s response to an infection.
Septic Shock: Multiple organ failure resulting from advancement of severe sepsis.
Weapon of Mass Destruction (WMD): A former Soviet Union term that was used to denote nuclear, chemical, and biologic weapons. The term has been broadened to include radiologic weapons. Since the World Trade Center airliner attacks, the term includes any means to cause mass casualties.
Before September 11, 2001, terrorism did not have the full attention of the average American as it does today.1 However, with our past experience and current knowledge, we must be able to define what bioterrorism is and how it impacts the postanesthesia care unit (PACU).
The Centers for Disease Control and Prevention (CDC) define bioterrorism as the intentional release (or threatened release) of viruses, bacteria, or their toxins for the purposes of harming or killing citizens.2 Potential vehicles of releasing the biologic agents include aerosolization, insects, and food and water source contamination.2 As a critical care unit, the PACU will be challenged to adapt usual care to supplement mass casualty victims of bioterrorism. The PACU must prepare immediately for this inevitable role, brainstorming scenarios by participating in mock disaster drills and augmenting staff competencies. The release of biologic weapons is specifically designed to promote or spread fear or intimidation upon an individual, a specific group, or the population as a whole for religious, political, ideological, financial, or personal purposes.3 Overwhelming terror and panic are just two of the psychological goals, with incapacitation and destruction as the ultimate objectives. Deliberate release of biologic agents is a growing and real threat, because the agents are easier to acquire and are more likely to be used. Unlike nuclear, radiologic, or chemical attacks, biologic attacks can be overt or covert and much easier to deploy. Covert attacks offer no immediate effects on victims because of a delay between exposure and onset of illness (incubation period).4 There are several advantages of covert biologic operations including: biologic agents are easier to hide, decreasing the chance of disclosure; biologic agents are cheaper, allowing small radical groups or single individuals access; and release might not be detected until the incubation period is completed, eliminating the “window of opportunity” for postexposure prophylaxis.5
Historical use of bioterrorism
Greek history documents one of the earliest written descriptions of biologic weapons being used. In 184 BC, Hannibal used snakes as a biologic weapon by casting pots of poisonous snakes into the midst of the Pergamene forces, ultimately defeating them. In 300 bc, the Greeks used decaying bodies to pollute the water supply of their enemies.1 In the fourteenth century, bodies infected with plague were catapulted over the walls of cities in an attempt to infect the habitants and attenuate their defenses. Blankets that were once used to wrap smallpox victims were subsequently distributed to Native Americans in an effort to infect and incapacitate them. The use of biologic weapons continued into the 1900s, and stakes became higher as the sophistication of microbiology improved and travel became easier. During World War I, the Germans inoculated horses and cattle with anthrax and glanders before shipping them to France.6 In 1937, Japan started a biologic warfare program code named Unit 731. An investigation after World War II revealed that the Japanese used prisoners of war as research subjects for aerosolized anthrax and also dropped plague-infected fleas over China and Manchuria.6
In 1925, the Geneva Protocol called for the first multilateral agreement for the prohibition of biologic warfare.1 This agreement served to describe biologic warfare, but did not address the prevention of their use. During World War II, there were accusations that the United States used biologic agents against the Eskimos in Canada and released the Colorado beetles on crops in Germany. In 1942 at a small National Guard airfield (Fort Detrick), the United States began a research and development program on the use of biologic agents. This program produced agents and conducted field testing on biologic agents until 1969, when President Richard Nixon stopped all offensive biologic and toxin weapon research and production by executive order. In 1953, the United States initiated a medical defensive program against biologic warfare at the U.S. Army Medical Research Institute of Infectious Disease that continues today.7 Over recent decades, the threat has changed from Cold War scenarios to the asymmetric and terrorist threat.5 In 1978 the toxin “yellow rain,” was used in the assassination of a exiled Bulgarian in London.6 Terrorist plots to use ricin were uncovered in England in January 2003, in a South Carolina postal office, and in the Dirksen Senate Office Building in Washington D.C.6 Lawmakers were directly affected in October 2001 when an anthrax contamination resulted in the closing the Hart Senate Office Building in Washington D.C. shortly after the terrorist attack on September 11, 2001.6 Radical groups or individuals can easily gain access to biologic agents. Iraq had a large biologic weapons program, and in 1995 they admitted to producing and deploying bombs, rockets and aircraft spray tanks containing Bacillus anthracis and botulinum toxin.7 In 1995, a cult in Japan released sarin gas in a Tokyo subway, resulting in significant injury. This same group had additional plans for biologic terrorism involving botulinum toxin, anthrax, and drone aircraft carrying spray tanks.7 They had also traveled to Zaire in 1992 to obtain Ebola virus.7 It is concerning that access to once highly protected biologic weapons is becoming easier for the highest bidder. In the former Soviet Union, one of the former biologic weapons laboratory facilities, highly protected in the 1980s, was left vulnerable with a few guards who had not been paid in months. The location of the smallpox, Ebola, Marburg, and hemorrhagic fever viruses that were stored there remain unknown.7 Today’s global economy, free and mobile society, instant Internet connectivity, and continued research indicate the most worrisome infections have yet to be recognized.6
Bioterrorism agents
The Centers for Disease Control and Prevention (CDC) classifies bioterrorism agents into three groups (Table 56-1). Category A includes high-priority agents that could pose a risk to national security because they can be easily disseminated, result in high mortality rates, have the potential for major public health impact, might cause public panic, and require special action for public health preparedness.8 Category B includes agents that are moderately able to be disseminated, resulting in moderate morbidity and low mortality rates, and require specific enhancements of the CDC’s diagnostic capacity and enhanced disease surveillance.8 Category C is the lowest priority and includes emerging pathogens that could be engineered for mass dissemination in the future because of the availability, ease of production, dissemination, and the high morbidity and mortality rates and major health impact.8
Table 56-1 CDC Categories of Bioterrorism Agents and Diseases
| CATEGORIES | BIOTERRORISM AGENTS AND DISEASES |
|---|---|
| Category A |
CDC, Centers for Disease Control and Prevention; EEE, eastern equine encephalitis, SARS, severe acute respiratory syndrome; VEE, Venezuelan equine encephalitis; WEE, western equine encephalitis.
From Woods JB: USAMRIID’s medical management of biological casualties handbook, ed 6, Fort Detrick, Frederick, Md, 2005, U.S. Army Medical Research Institute of Infectious Disease, available at www.usamriid.army.mil/education/bluebookpdf/USAMRIID%20BlueBook%206th%20Edition%20-%20Sep%202006.pdf. Accessed April 10, 2011.
Anthrax
In the PACU, patients may exhibit a wide variety of conditions and syndromes. Many are related to the respiratory system. For example, anthrax has three identifiable symptom clusters. Bacillus anthracis, a spore-forming bacterium, can lead to inhalational anthrax, which can appear much like a case of influenza, atypical pneumonia, or pneumonic plague. In its classic form, it appears in two phases. The first phase follows an incubation period of up to 6 days and is characterized by a nonspecific syndrome of fever, chills, weakness, muscle pain, headache, dyspnea, nonproductive cough (a diagnostic clue), and abdominal or chest pain. It then progresses to a second phase over 2 or 3 days, with progressive fever, diaphoresis, severe dyspnea, and possibly cyanosis. In 50% of the cases, hemorrhagic meningitis occurs and leads to delirium, meningismus, obtundation, seizures, and coma. An additional diagnostic clue is mediastinal widening, as revealed on chest radiographs or tomographic scan results. The patient may have stridor and subcutaneous edema of the upper thorax or neck. This syndrome can progress to obtundation and coma, with hypothermia, circulatory failure, and death within 2 to 3 days. Prompt treatment with antibiotics may result in survival. Finally, the rarest form of anthrax, gastrointestinal anthrax, occurs when undercooked contaminated meat is consumed. Gastrointestinal anthrax is characterized by acute inflammation of the gastrointestinal tract and can lead to ulcers in the upper tract (oropharynx) or in the terminal ileum or cecum. Presenting symptoms include fever, sore throat, difficulty swallowing, nausea, vomiting, abdominal pain, bloody diarrhea, and total body sepsis. Mortality rates are higher than 50%. The gastrointestinal disease can be confused easily with nonspecific gastroenteritis and other bacterial or viral syndromes.
Smallpox
In 1977, smallpox was eradicated worldwide with routine vaccination not administered since 1972.1 Because of this documented eradication, the reappearance of the disease would be highly indicative of a bioterrorism attack. Smallpox is caused by the variola virus and is highly infectious, spreading from person to person primarily via respiratory tract. The virus can spread through oral secretions, drainage from lesions, and direct contact with contaminated items such as blankets. Five clinical syndromes of smallpox can be observed. The initial symptoms of high fevers, headache, backache, malaise, and vomiting closely resemble other acute viral illnesses, including influenza. During the first 2 to 3 days, the maculopapular rash is almost indistinguishable from chicken pox, except for its centripetal evolution. The rash continues to evolve, and by day 8 or 9 the lesions start to crust and scabs begin to develop. The risk of transmission lasts until all the scabs have fallen off. Smallpox can also take on a hemorrhagic form, which is characterized by diffuse hemorrhagic manifestations and a rapid progression to death. The flat type has a fatality rate of 95% and is characterized by a slow evolution of flat soft focal skin lesions and severe systemic toxicity. The nurse in the PACU is unlikely to encounter smallpox because this contagious systemic viral illness with its characteristic skin rash would likely be treated as an international emergency, with mandatory treatment at home in isolation conditions. Within the hospital setting, patients with smallpox would be under strict airborne isolation in a negative-pressure room with high-efficiency particle air filtration. No proven treatment exists for the disease. Supportive therapy includes hydration and electrolyte replacement for hypovolemic shock. Patients with flat and hemorrhagic types may need mechanical ventilatory support, because the incidence of pulmonary edema is higher. Contacts of cases should be vaccinated within 3 to 4 days, because vaccination can decrease the severity of the disease. Cidofovir, an antiviral agent, has shown effectiveness in laboratory cultures when given in the first 1 or 2 days and is a promising research development.
Severe acute respiratory syndrome
Severe acute respiratory syndrome (SARS) is a viral respiratory illness caused by the coronavirus.9 It was first reported in 2003 in Asia but quickly spread globally. In the following 2 months, the disease spread to more than 24 countries in North America, South America, Europe, and Asia.9 The World Health Organization acknowledged that approximately 8000 people contracted SARS in 2003, with 774 deaths.9 The presenting symptoms are usually fever, headache, an overall feeling of discomfort, and body aches. After 2 to 7 days a dry cough develops, and many patients develop pneumonia. Treatment is based on symptoms. If pneumonia develops, antibiotics may prove effective. SARS is spread from person to person through close contact. Contact and droplet precautions should be used to prevent the spread to other patients and staff members.9
Viral hemorrhagic fevers (ebola, marburg, lasso)
Viral hemorrhagic fever is a group of illnesses caused by distinct families of viruses. In general, the name viral hemorrhagic fever is used to describe a severe multisystem syndrome in which the vascular system is damaged.10 Symptoms include a rapidly escalating illness beginning with fever, fatigue, dizziness, muscle aches, loss of strength, and exhaustion. Severe cases show signs of bleeding under the skin, in internal organs, and from body orifices such as the mouth, ears, or eyes, in addition to nervous system shutdown, shock, coma, and seizure.
Viral hemorrhagic fevers are transmitted to humans from rodents or arthropod vectors. Ebola, Marburg, Lassa, and Crimean-Congo hemorrhagic fever viruses can be transmitted from person to person after the initial person is infected from a rodent or arthropod vector.10 Other vectors spread the disease to animals or livestock. Humans acquire the disease when they care for or slaughter animals.10
Preparedness
The best preparation for an inevitable attack is knowledge and the sharing of that knowledge. With such repugnant, unconventional choices of biologic weapons, is it possible to prepare? Like any mass casualty events, there will be chaos, but using a standard national emergency plan, the state and county health department levels can provide a local response plan. Each hospital is required by The Joint Commission to have an emergency plan that includes bioterrorism. Because the discovery of a biologic attack might be recognized at the hospital emergency department or a physician’s private office, local health care facilities must always maintain an index of suspicion and facilitate quick action. Incidents that would suggest a possible biologic event include: multiple people suddenly becoming ill quickly in a normally healthy population, the epidemic curve rising and falling during a short period of time, an unusual number of people with similar symptoms (especially with fever, respiratory or gastrointestinal complaints), a large number of rapidly fatal cases occurring, or patients exhibiting relatively uncommon symptoms (Table 56-2). The local and state Public Health Departments should be notified immediately.
As with any mass casualty, a single facility might be overwhelmed with patients. The hospital’s emergency plan will delegate roles to accommodate the patient load with properly skilled staff. All elective surgeries will be cancelled, and only emergency surgeries will be performed. Because the PACU is also a critical care unit by definition,11 the perianesthesia nurse’s special capabilities may be required to care for ICU overflow patients and provide beds for patients needing mechanical ventilation and one-on-one patient care. The PACU directors need to ensure that their staff receives the competency training needed to provide for this expanded role. Cross training in the ICU could help to maintain those skills needed to care for the critically ill patient. During mass casualty practices, serious and creative role play can assist in problem solving issues that could be problematic if a real event should occur. Staffing issues, space, and supply acquisition solutions should be considered. The “just in time” mindset for supplies and staff will be a detriment. Minimal staff and supplies will necessitate working with other hospitals and distribution supply houses. All staff members must to be prepared for emergencies and to successfully care for patients. That preparation must occur before a real emergency. The staff members will need to make contingency plans for their own families to decrease the stress during staff recall. Stress will be elevated and workplace violence could be an issue. Staff member concerns for personal safety and that of their family, patients, and family members who are stressed, and lack of preparation and planning can contribute to workplace violence. Recognition and training on workplace violence, “zero tolerance” for workplace violence, and an open door policy for the administration and stress teams will assist to diminish the possibility workplace violence will occur.12
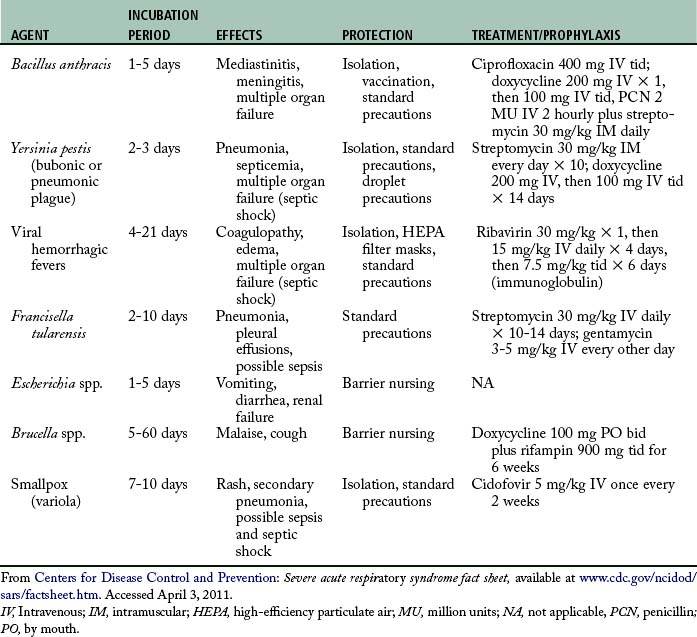
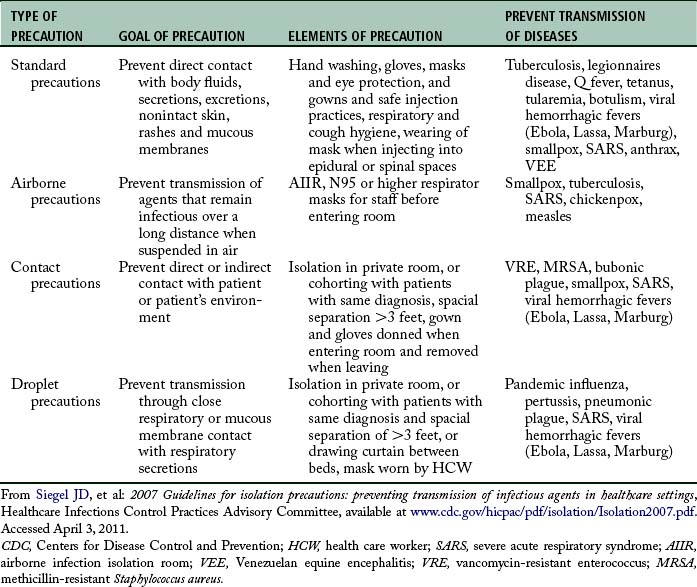
Health care workers must always protect themselves first. The use of appropriate personal protective equipment, appropriate patient isolation, and hand washing when dealing with any patient will protect against most biological agents (Table 56-3). It is important for health care workers to maintain a healthy life style that includes current immunization status (e.g., tetanus, diphtheria, influenza vaccine, polio). In the event of an exposure secondary to caring for victims of a biologic incident, rapid postexposure treatment (prophylactic medications or vaccinations) must be started.
Response
Practice good infection control. The simplest and most effective practice a nurse can have to reduce contamination and spread infection is hand washing. Personal protective equipment (e.g., gown, mask, gloves, hair cover) should be used if an infectious disease is suspected. This is true for any potentially infectious patient or one known to be contaminated with a biologic agent associated with terrorism.13
Decontamination of the patient may be required. If the biologic attack is overt, decontamination should occur. Removing all clothes and sealing them in a plastic bag as well as a shower with soap and large amounts of water are important to dilute and remove biologic agents. Bleach kills the anthrax spores on clothes and objects, but it should not be used on skin. In the event of a covert attack, decontamination is not important because of the time from exposure. The medical facility should quickly attempt to make a presumptive diagnosis and not delay treatment awaiting complete test results. Treatment should begin immediately as it is most effective in the prodromal phase. Empiric treatment of respiratory casualties should be used because they might have anthrax, plague, or tularemia.
Patient treatment should follow the advanced trauma life support protocol, concentrating on airway, breathing, and circulation. New best practice guidelines recommend using the Surviving Sepsis Campaign model for improvement of care using bundles.14 A bundle is a group of therapies that, when implemented together, may result in better outcomes for patients with sepsis than if implemented individually. The individual components included in a bundle are built around best evidence-based practices. Use of the Severe Sepsis Bundles can achieve a 25 percent reduction in mortality due to severe sepsis or septic shock. 14
Source: Levy M: The surviving sepsis campaign, Society of Critical Care Medicine 2010, available at www.survivingsepsis.org/About_the_Campaign/Pages/CommentaryMitchell MLevy,MD,FCCM.aspx. Accessed April 20, 2011.
As seen in Table 56-2, bacterial infections can lead to sepsis quickly, especially anthrax, tularemia, pneumonic plague. Through evidence-based recommendations for sepsis management and treatment, rapid and clearly articulated strategies help to reduce negative outcomes from sepsis. The intention is to apply the bundles 100% of the time within the first 6 hours of identification of severe sepsis.
Isolation for patients can present a problem. Gathering patients with similar symptoms into a separate room or area of a room and separating the infected persons from postoperative patients solves the problem of isolation needs. Manipulation of ventilation and air pressure within smoke compartments can provide a solution for negative pressure rooms. See Table 56-2 for specific requirements for each agent.
Summary
Tremendous resources are being injected into bioterrorism response systems. The Federal Bureau of Investigation), Department of Defense, CDC, Federal Emergency Management Agency, and states and municipalities are all receiving funds to develop their responses. Computerized communications systems, large quantities of antibiotic dose-packs, vaccines, decontamination systems, hazardous materials suits, and biosafety laboratories all can be made available on short notice. These vast resources are only called into play if an alert health professional detects an unusual situation and notifies the local health department. That local health department must have the epidemiologic and laboratory support to confirm or deny the possibility of a threat exposure. The keen clinician can alert the authorities and put the appropriate resources into play.
The old adage applies in this case, as in so many others; “If we fail to plan, then we must plan to fail.”
1. Jones R, VanGilder A. Bioterrorism agents: what the anesthesiologist needs to know, The Internet Journal of Anesthesiology. available at: www.ispub.com/journal/the-internet-journal-of-anesthesiology/volume-16-number-2/bioterrorism-agents-what-the-anesthesiologist-needs-to-know.html, April 5, 2011. Accessed
2. Public Health Response to Biological or Chemical Terrorism: Interim planning guidance for state public health officials, U.S. Department of Health and Human Services. available at: www.bt.cdc.gov/Documents/Planning/PlanningGuidance.PDF, April 10, 2011. Accessed
3. Abraham RB. Practical guidelines for acute care of victims of bioterrorism: conventional injuries and concomitant nerve agent intoxication. Anesthesiology. 2002;97(4).
4. Khan AD, Sage M. Biological and chemical terrorism. strategic plan for preparedness and response. 2000;49(RR04):1–14. available at cdc.gov/mmwr/preview/mmwrhtml/rr4904a1.htm Accessed April 10, 2011
5. Bland SA. Chemical, biological and radiation casualties: critical care considerations. JR Army Med Corps.2009;155(2):122–174.
6. Woods JB, ed. USAMRIID’s medical management of biological casualties handbook, ed 6, Fort Detrick, Frederick, Maryland: U.S. Army Medical Research Institute of Infectious Disease, 2005. available at www.usamriid.army.mil/education/bluebookpdf/USAMRIID%20BlueBook%206th%20Edition%20-%20Sep%202006.pdf Accessed April 10, 2011
7. Henderson DA. Bioterrorism as a public health threat. Emerging Infectious Diseases. 4(3), 1998. available at www.cdc.gov/ncidod/eid/vol4no3/hendrsn.htm Accessed April 15, 2011
8. Centers for Disease Control and Prevention. Bioterrorism agents/disease. available at www.bt.cdc.gov/agent/agentlist-category.asp Accessed April 3, 2011
9. Centers for Disease Control and Prevention. Severe acute respiratory syndrome fact sheet. available at www.cdc.gov/ncidod/sars/factsheet.htm, April 3, 2011. Accessed
10. Centers for Disease Control and Prevention. Viral hemorrhagic fevers fact sheet. available at www.cdc.gov/ncidod/dvrd/spb/mnpages/dispages/Fact_Sheets/Viral_Hemorrhagic_Fevers_Fact_Sheet.pdf, April 20, 2011. Accessed
11. A Joint Position Statement on ICU Overflow Patients developed by ASPAN AACN, and ASA’s Anesthesia Care Team Committee and Committee on Critical Care Medicine and Trauma Medicine. Perianesthesia nursing standards and practice recommendations. available at www.aspan.org/Portals/6/docs/ClinicalPractice/PositionStatement/1012/Pos_Stmt_7_MedSurg_OverflowPts.pdf, April 20, 2011. Accessed
12. A Position Statement on Workplace Violence in the Perianesthesia Settings. Perianesthesia nursing standards and practice recommendations. available at www.aspan.org/Portals/6/docs/ClinicalPractice/PositionStatement/1012/Pos_Stmt_13_Workplace_Violence.pdf, April 20, 2011. Accessed
13. Siegel JD, et al. 2007 Guidelines for isolation precautions: preventing transmission of infectious agents in healthcare settings, healthcare infections control practices advisory committee. available at: www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf, April 3, 2011. Accessed
14. Levy M. The surviving sepsis campaign, Society of Critical Care Medicine 2010. available at www.survivingsepsis.org/About_the_Campaign/Pages/CommentaryMitchellMLevy,MD,FCCM.aspx, April 20, 2011. Accessed
Arnon SS, et al. Botulinum toxin as a biological weapon: medical and public health management. JAMA. 2001;285(8):1059–1070.
Baker D. Chemical and biological warfare agents: the role of the anesthesiologist. Miller RD, ed. Miller’s anesthesia. ed 7. Philadelphia: Churchill Livingstone; 2010.
Candiotti KA, et al. Critical care and trauma emergency preparedness for biological and chemical incidents: a survey of anesthesiology residency programs in the United States. Anesthesia and Analgesia.2005;101:1135–1140.
Centers for Disease Control and Prevention. Emergency preparedness. available at www.bt.cdc.gov, November 29, 2011. Accessed
Clark NP, Rinderknecht JL. Bioterrorism: intentional introduction of animal disease. Rev Sci Tech. 2011;30:131–138.
College of Nurses of Ontario: Infection prevention and control practice standards. available at: www.cno.org, April 5, 2011. Accessed
English JF, et al. Bioterrorism readiness plan: a template for healthcare facilities. APIC Bioterrorism Task Force and CDC Hospital Infections Program Bioterrorism Working Group; 2002.
Foster D. Smallpox as a biological weapon: implications for the critical care clinician. Dimens Crit Care Nurs.2003;22(1):2–9.
Heyman DL, ed. Control of communicable diseases manual. ed 17. Washington, DC: APHA; 2009.
Inglesby TV, et al. Plague as a biological weapon: medical and public health management. JAMA. 2000;283(17):2281–2290.
Inglesby TV, et al. Anthrax as a biological weapon: medical and public health management. JAMA. 1999;281(18):1735–1745.
Karwa M, et al. Bioterrorism: preparing for the impossible or the improbable. Crit Care Med.2005;33(Suppl 1):S75–95.
Schwartz MN. Recognition and management of anthrax: an update. N Engl J Med. 2001;345(22):1621–1626.
Shafazand S, et al. Inhalational anthrax. Chest. 1999;116:1369–1376.
Steinhauer R. Bioterrorism. RN. 2002;65(3):48–55.
Switala CA, et al. Bioterrorism—a health emergency: do physicians believe there is a threat and are they prepared for it. Am J Disaster Med.2011;6:143–152.
Thavaselvam D, Vijayaraghavan R. Biological warfare agents. J Pharm Bioallied Sci. 2010;2:179–188.
Varkey P, et al. Confronting bioterrorism: physicians on the front line. Mayo Clinic Proc. 2002;77(7):661–672.