Chapter 28 Biomechanics of Intratunnel Anterior Cruciate Ligament Graft Fixation
Introduction
In 1983, Lambert1 first introduced the technique of intratunnel anterior cruciate ligament (ACL) graft fixation by securing a vascularized bone–patellar tendon–bone (BPTB) ACL graft with 6.5-mm AO cancellous screws. General acceptance of interference screw fixation of BPTB ACL grafts came about in large part due to the biomechanical study of Kurosaka et al.2 This study demonstrated that fixation of a 10-mm BPTB ACL graft in human cadaveric knees with a custom-designed, headless, 9-mm, fully threaded interference screw had superior strength and stiffness compared with fixation with a 6.5-mm AO cancellous screw, staple fixation, or sutures tied over a button.2 Because of the many biomechanical studies demonstrating superior initial fixation properties and clinical outcomes studies demonstrating a high rate of success, interference screw fixation of BPTB grafts is now considered the standard against which all ACL graft fixation techniques are compared.3,4 Based on the success of interference screw fixation of BPTB ACL grafts, Pinczewski5 in 1993 introduced the use of blunt threaded metal interference screws to fix four-strand hamstring tendon ACL grafts. This fixation technique has subsequently been extended to the use of nonmetallic bioabsorbable interference screws.
In the late 1960s, Morrison,6,7 using force plate and gait analysis, estimated the forces experienced by the ACL during activities of daily living to range from 27 N to 445 N. Noyes et al8 estimated that the ACL is loaded to approximately 454 N during activities of daily living. However, at the present time the forces placed on the ACL with rehabilitation exercises performed in the early postoperative period or during activities of daily living are unknown. In vitro mechanical studies have demonstrated that the initial strength and stiffness of BPTB and four-strand hamstring grafts far exceed the estimated loads on the ACL.8–10 However, compared with ACL grafts, all current ACL graft fixation methods demonstrate inferior initial tensile properties.11 Therefore mechanical fixation of the ACL graft in the bone tunnels is the weak link in the early postoperative period. Consequently, initial graft fixation properties are of great relevance in determining the success of ACL reconstruction in the early postoperative period.
Limitations of Biomechanical Studies
In vitro biomechanical studies are most commonly used to evaluate initial ACL graft fixation properties.12,13 However, in vitro biomechanical studies have inherent limitations. First, the use of different research models and biomechanical testing protocols make it difficult to compare the results of one study with another. Ideally, human specimens are used for biomechanical testing; however, the material properties of cortical and cancellous bone, tendons, and ligaments can vary greatly among specimens. Because of the lack of availability of human cadaveric specimens in the age range of patients typically undergoing ACL reconstruction, specimens from older donors are often used or the same specimen is tested multiple times. As demonstrated by Brown et al,14 the use of specimens from older human donors underestimates the fixation strength of fixation devices that rely on cancellous bone for fixation strength. In this study, the initial fixation strength of BPTB grafts fixed with metal interference screws in the distal femur of bovine cadavers, young human cadavers (mean age 41 years, range 33–52 years), and elderly human cadavers (mean age 73, range 68–81 years) was compared. There was no significant difference in the failure load of the bovine (799 ± 261 N) and young human specimens (655 ± 186 N); however, the failure load of the elderly human specimens (382 ± 118 N) was significantly lower than the young human and bovine specimens. Based on these findings the authors concluded that elderly human cadavers are not an appropriate model for ACL reconstruction fixation studies. Performing multiple tests in the same specimen will introduce carryover effects that may affect the fixation properties of subsequent fixation techniques after the first fixation method has been tested. Beynnon and Amis12 suggest testing male specimens younger than 65 years old and female specimens younger than 50 years old to minimize these problems.
Due to the paucity of suitable human cadaveric specimens, animal models are often used. Animal models have the advantage of eliminating the potential variability introduced because of the large differences in bone mineral density (BMD) that exist in human specimens, and their availability eliminates the need to perform multiple tests using the same specimen. However, because of the differences in BMD and tensile properties of bone that exist between human and animal specimens, the results of biomechanical tests performed using animal models cannot be directly compared with studies performed using human specimens.15 Aerssens et al15 have shown that human female femoral specimens (age range 30–60 years) demonstrate lower BMD and failure stress compared with specimens from dogs, pigs, cows, or sheep. In this study the pig femur came closest to matching the BMD and failure stress of the human femur. Because of the higher BMD and tensile properties of animal specimens, biomechanical tests performed in animal models tend to overestimate initial fixation properties.16,17 This is particularly true for devices such as interference screws and cross-pins that rely on cancellous bone for fixation strength.
Another limitation of in vitro biomechanical studies is that they simulate the time zero period prior to biological fixation of the ACL graft. These studies fail to account for the progressive healing of the ACL graft to the bone tunnel walls, which shifts the weak link from the ACL graft–fixation–bone tunnel interface to the bone–ligament interface and eventually to the intraarticular part of the ACL graft.18 Although the healing response does not affect graft fixation properties in the early postoperative period, bony or soft tissue healing in the bone tunnels will alter graft fixation properties over time. Few studies document the time frame for healing to occur at the ACL graft fixation sites. Based on the studies of Clancy et al18 and Walton,19 it appears that the bone blocks of BTB grafts heal to the bone tunnel wall by 6 weeks. Compared with BTB grafts, soft tissue grafts take longer to heal to bone. In a dog model, Rodeo et al20 demonstrated the formation of Sharpey’s fibers connecting the periphery of a soft tissue graft to the bone tunnel wall at 6 weeks. However, mechanical fixation was not achieved until 12 weeks.
Two types of biomechanical tests are commonly used to evaluate the mechanical behavior of ACL ligament fixation techniques.12,13 The first and most commonly used is the single-cycle load to failure (single LTF) test. Single LTF tests attempt to simulate the response of the graft fixation technique to a sudden mechanical overload event such as a slip or fall. The load-displacement curve can be analyzed to determine the ultimate failure load, yield load, linear stiffness, and displacement at failure. Advantages of single LTF testing are that the weak link in the fixation system can be easily identified, the mode and site of the fixation failure are well defined, and an upper limit of the strength of the graft-fixation construct is established. Because failure testing attempts to replicate traumatic loading conditions, a high rate of elongation, typically 100% per second, is used.
The second testing method involves cyclical loading of the bone–ACL graft–fixation complex. Cyclical testing evaluates the ability of the bone–ACL graft–fixation complex to resist elongation or slippage under repetitive submaximal failure loads over time. Cyclical testing attempts to approximate the loading conditions associated with rehabilitation exercises or activities of daily living in the early postoperative period prior to biological fixation of the graft. Most commonly a load control test is performed, in which the upper and lower loads are controlled and displacement over time of the ACL graft relative to the bone is measured. By determining the distance between markers on the bone and the ACL graft at the beginning and end of the test, elongation or slippage of the ACL graft with respect to the bone can be measured. At the present time there is little agreement on the force limits or the number of cycles that should be performed, making it difficult to compare data among studies. Beynnon and Amis12 have recommended force limits between 150 N and −150 N and 1000 load cycles. One thousand cycles approximates 1 week of flexion-extension loading of the knee.13 The number of cycles is limited by the ability to keep the specimen moist during testing and the thawing of the freeze clamps that are commonly used to grip soft tissue ACL grafts.
Bone Mineral Density
Because intratunnel fixation methods depend on the graft fixation device generating friction between the bone tunnel wall and the ACL replacement graft, BMD is perhaps the most important variable that influences initial fixation strength and stiffness and resistance to slippage during cyclical loading. It is well known that BMD in humans decreases with age and that the BMD of females is less than that of males. Cassim et al21 found that the fixation strength of BPTB grafts fixed with metal interference screws in human specimens with a mean age of 79 years resulted in a 42% decrease in failure load compared with specimens with a mean age of 35 years. There are also significant differences in the BMD of the human distal femur and proximal tibia.22 The BMD of the proximal tibia is significantly lower than that of the distal femur.22 The lower BMD of the proximal tibia, along with the fact that tibial fixation devices must resist shear forces applied parallel to the axis of the tibial bone tunnel, combine to make tibial fixation the weak link in ACL graft fixation.
Although BMD is a critical factor, other variables correlate with initial fixation properties. In a BPTB model, Brown et al14 found that insertion torque, an indirect measure of BMD, was linearly correlated with pullout force but with weak significance. Using elderly human cadaveric knees, Brand et al22 found that BMD measured using dual-energy x-ray absorptiometry and screw insertion torque was strongly correlated to the fixation strength of doubled semitendinosus and gracilis tendons fixed with bioabsorbable interference screws in the distal femur and proximal tibia of human specimens. In this study, the variables of insertion torque and BMD explained 77% of the ultimate failure load observed. The R2 value for the relationship between ultimate failure load and BMD was 0.65, indicating that BMD explained 65% of the ultimate failure load. This study found that BMD of 0.6 gm/cm2 resulted in better initial fixation properties. Using the proximal tibia of human cadaveric specimens (mean age 40 ± 11 years, range 17–54 years) and doubled tibialis tendons fixed with a tapered bioabsorbable screw, Jarvinen et al23 found that insertion torque was linearly correlated to fixation strength (R2 = 0.54) and was the most strongly associated variable in their study for predictors of fixation strength. Unfortunately, despite the correlation, insertion torque was a poor predictor of cyclical loading failure or single LTF. Clearly, other secondary factors influence the properties of intratunnel graft fixation. The remainder of this chapter is aimed at understanding the role and importance of these other variables.
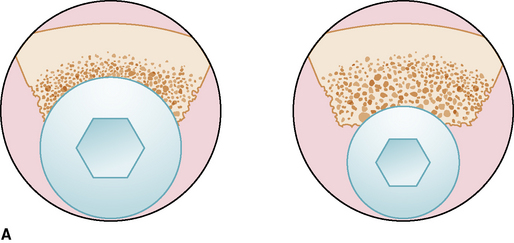
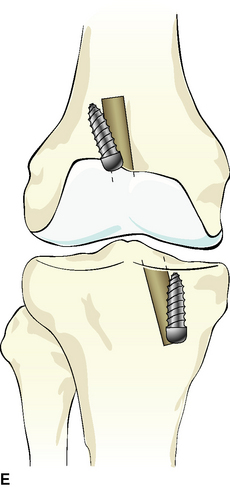
Bone–Patellar Tendon–Bone Fixation
Interference screw fixation of BTB ACL grafts has been well studied and documented over the past 20 years. The fixation properties of interference screw fixation of BTB grafts depend on the generation of friction between the bone block and bone tunnel wall. Friction is generated by compression of the bone block into the bone tunnel wall and engagement of the screw threads into the bone block and bone tunnel wall. As illustrated in Fig. 28-1, factors that influence the initial tensile properties of interference screw fixation of BTB ACL grafts include the following:
Overlap exists between the effects of screw diameter and gap size on initial fixation properties. In the study of Kurosaka et al,2 custom-made 9.0-mm screws demonstrated higher ultimate failure loads compared with 6.5-mm AO cancellous screws. However, the researchers reported that making the size of the patellar and tibial bone blocks close to the size of the bone tunnels was extremely important “in obtaining a solid fixation.”2 Using a porcine experimental model, Reznik et al24 demonstrated that gap size significantly influenced the ultimate failure load of BTB grafts fixed in 10-mm bone tunnels with 7-mm screws. When the gap between the bone block and bone tunnel wall was 4 mm or more, increasing the screw diameter to 9 mm increased the failure load by 97%. However, when the gap was less than 4 mm and a 9-mm screw was used, the results were inferior to those seen with a 7-mm screw and a gap of less than 4 mm. Kohn and Rose,25 using human cadaveric knees (mean age 30 years), reported that both femoral and tibial fixation using 9-mm screws were stronger than with 7-mm screws. Based on their findings, they recommended against using 7-mm screws for tibial fixation.
However, Hulstyn et al,26 using a bovine femur–BPTB–tibia model found no significant difference in fixation strength between 7- and 9-mm screws. Using elderly human cadaveric specimens, Brown et al27 found no significant difference in the fixation strength of BPTB grafts fixed in the distal femur using endoscopically inserted 7-mm screws and 9-mm screws inserted using a rear-entry technique. Brown et al14 also found no difference in femoral fixation between 7- and 9-mm screws. The influence of screw diameter on initial fixation properties is probably most relevant when a significant size discrepancy exists between the bone block and the bone tunnel wall. This difference is often referred to as gap size.
After studying various fixation methods, Kurosaka et al2 hypothesized that the gap size between the bone block and bone tunnel was a critical factor in interference screw fixation. Cassim et al21 demonstrated the interrelationship between gap size and screw diameter in determining fixation strength in BPTB reconstruction. When the gap size was less than 1 mm and a 9- × 30-mm screw was used, the mean ultimate failure load was 1060 N. Butler et al28 found that with a gap size of 3 to 4 mm, increasing the screw diameter size from 7 to 9 mm significantly increased the load at which failure occurred. A number of authors have suggested using larger screws as the gap size increases.29
Screw length probably does not have a large influence on the initial fixation properties of BPTB grafts fixed with interference screws. Brown et al27 found no significant difference in fixation strength between 7- × 20-mm and 7- × 30-mm screws or between 9- × 20-mm and 9- × 30-mm screws fixed in the distal femur of human specimens. Black et al30 compared 9- × 12.5-mm, 9- × 15-mm, and 9- × 20-mm interference screws in a porcine tibia model. No significant difference in insertion torque, failure load, stiffness, or displacement to failure was found between the different lengths of screws. Pomeroy et al31 also found no significant effect of screw length on fixation strength for a given screw diameter. These findings may be explained by the fact that the length of the bone block is limited, and increasing the length of the screw does not lead to an increase in the number of screw threads in contact with the bone block and bone tunnel wall.
Divergence of the interference screw from the bone block and the axis of the bone tunnel can occur with both rear-entry and endoscopic techniques. The incidence of screw divergence is more common with the endoscopic technique (femur > tibia).32 Based on clinical studies, screw divergence less than 30 degrees does not seem to have a significant effect on the clinical outcome.33 Using a porcine model, Jomha et al34 reported no significant difference in femoral fixation strength with endoscopically inserted interference screws with divergence up to 10 degrees. However, there was a significant drop in femoral fixation strength with screw divergence at 20 degrees. Pierz et al,35 using porcine tibiae, demonstrated that interference screws inserted to simulate a rear-entry femoral fixation technique or fixation of a tibial bone block resulted in a significant decrease in fixation strength from 0 to 15 degrees and 15 to 30 degrees of divergence. Interference screws inserted to simulate an endoscopic technique resulted in a significant decrease in fixation strength only at 30 degrees of screw divergence. These authors concluded that optimal interference screw fixation occurs when the screw is placed parallel to the bone block and bone tunnel. Due to the creation of a wedge effect, screw divergence has a lesser effect on endoscopically inserted femoral screws. However, due to the in-line direction of pull, minor degrees of divergence will affect the fixation strength of femoral screws inserted through a rear-entry technique and tibial fixation screws.
Metal interference screws can distort MRI images, lacerate the graft during insertion, and complicate revision ACL surgery. Bioabsorbable interference screws have been proposed as a method to eliminate these potential complications.36 Several biomechanical studies have compared the initial fixation strength of bioabsorbable interference screws and conventional metal interference screws in animal and human cadaveric models. Weiler et al37 used a calf proximal tibia model to test the single LTF of six different biodegradable interference screws compared with that of a titanium interference screw. Five of the six bioabsorbable screws had failure loads and stiffness comparable with the metal screw. Similar results have been reported by Kousa et al,38 who found no significant difference in the tensile properties of BPTB grafts fixed with metal and bioabsorbable screws evaluated by single LTF and cyclical testing in a paired porcine model.
Guidelines and Recommendations for Intratunnel Fixation of Bone–Tendon–Bone Grafts
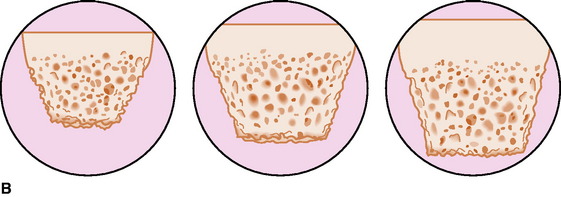
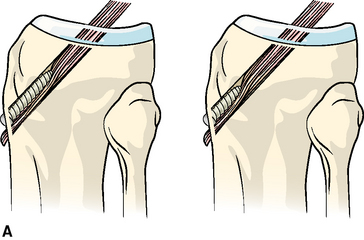
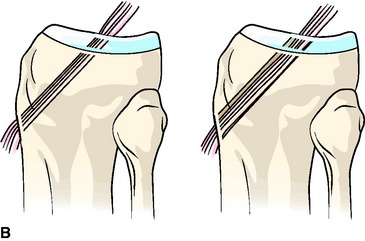
Soft Tissue Grafts
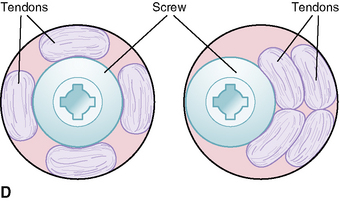
Interference screw fixation of soft tissue grafts depends on many of the same factors as fixation for BPTB grafts; however, the importance of each of these factors differs.39 Similar to BTB grafts, the initial fixation properties depend on the fixation device generating friction between the soft tissue graft and the bone tunnel wall. Friction is generated by compression of the soft tissue graft against the bone tunnel wall. However, because the soft tissue graft is more compressible than the bone blocks of BTB grafts, the amount of compression generated between the screw and bone tunnel wall for a given diameter of screw is less. The amount of friction contributed by engagement of the screw threads in the bone tunnel wall and soft tissue graft is also significantly lower due to the lack of engagement of the screw threads into the soft tissue graft. As illustrated in Fig. 28-2, factors that may contribute to the initial fixation properties of soft tissue grafts with interference screws include the following:
Unlike interference screw fixation of BTB grafts, screw length seems to have a greater effect on the initial fixation properties of soft tissue grafts fixed with interference screws. Because of the lower BMD of the proximal tibia, screw length has a greater influence on tibial fixation properties.22 Screw length may have a more significant effect on the fixation properties of soft tissue grafts because the area over which friction is generated between the bone tunnel wall and soft tissue graft is determined by the screw length rather than by the length of a bone block, which is typically 20 to 25 mm. In a bovine proximal tibia model, Weiler et al40 found that 23-mm screws had lower pullout strengths than 28-mm screws with equivalent diameters. This study also found that increasing screw length had a greater influence on failure load than increasing the screw diameter. Selby et al,41 using human tibias (age range 24–45 years), demonstrated significantly higher ultimate failure loads for 35-mm versus 28-mm screws. Harvey et al42 have investigated the effect of screw length and position using a bovine tibia model under cyclical loading conditions. Although not statistically significant, 45-mm-long metal screws demonstrated less slippage and “more consistent behavior” compared with 25-mm-long screws. Placement of the screw such that it engaged the cortex of the tibia allowed significantly less slippage compared with screw insertion that engaged only cancellous bone. Based on their findings, the authors recommend that the screw head be placed such that it engages the tibial cortex.
Few studies have examined the influence of screw diameter on the initial fixation properties of soft tissue ACL grafts with interference screws. Using human hamstring tendon grafts and bovine proximal tibiae, Weiler et al40 found that increasing the diameter of a 23-mm-long bioabsorbable interference screw from 7 to 8 mm increased the mean pullout force from 367 N to 479 N.
The fit of the soft tissue graft in the bone tunnel appears to have a significant influence on the initial fixation properties of interference screw fixation of soft tissue grafts. Using a human cadaveric model, Steenlage et al43 demonstrated that four-strand hamstring tendon grafts fixed in the distal femur with a bioabsorbable screw resulted in a significantly higher ultimate failure load if the bone tunnel was sized within 0.5 mm of the graft diameter versus within 1 mm of the measured size of the graft.
Because BMD has such a significant effect on the initial tensile properties of interference screw fixation of soft tissue grafts, compaction drilling or bone tunnel dilation has been proposed as a method of creating increased bone density along the bone tunnel walls. It has been speculated that this will lead to an improvement in initial fixation properties. Using human male cadaveric knees, Rittmeister et al44 demonstrated that serial dilation did not improve the initial fixation strength of four-strand hamstring tendon grafts fixed in the tibia with metal interferences screws. Nurmi et al45 investigated the effects of compaction drilling versus conventional drilling on the initial fixation strength of four-strand hamstring tendon grafts fixed with bioabsorbable screws in the proximal tibia of human specimens (mean age 41 ± 11 years, range 17–49 years). The biomechanical testing protocol consisted of cyclical loading followed by a single LTF test. They found no significant difference in initial stiffness or displacement between the two drilling methods during cyclical testing. In the single LTF test, there was no significant difference in yield load, displacement at yield load, or stiffness between the two drilling methods. The authors concluded that compaction drilling does not increase the initial fixation properties of hamstring tendon grafts.
In a second biomechanical study, Nurmi et al46 investigated the effect of tunnel compaction by serial dilators versus conventional drilling on the initial fixation strength of doubled anterior tibial tendons fixed in the proximal tibia of human specimens (mean age 40 ± 11 years, range 17–54 years) using bioabsorbable interference screws. The specimens were tested under cyclical loading followed by a single LTF test. They found no significant difference in stiffness or displacement between the two techniques during cyclical testing. However, the number of failures during cyclical loading of the extraction drilling group was twice that of the serially dilated group. In the subsequent single LTF test, there was no significant difference in failure load or stiffness between the two groups. One of the limitations of this study was that the size of the tibial bone tunnel was not matched to the size of the soft tissue grafts, and a 10-mm-diameter bone tunnel was created in all specimens.
The only study to demonstrate a beneficial effect of tunnel dilation on the fixation strength of soft tissue ACL grafts was performed by Cain et al47 using paired human cadaveric knees (average age 42 years, range 29–47 years). Four-strand hamstring tendon grafts were fixed with bioabsorbable screws in 0.5-mm matched femoral and tibial tunnels. The tibial tunnel was created using smooth tunnel dilators in one knee of the pair and conventional extraction drilling in the opposite knee of the pair. The femur-hamstring ACL graft–tibia complex was tested to failure using anterior tibial translation with the knee positioned in 20 degrees of flexion as previously described by Steiner et al.48 This method of testing attempts to mimic the Lachman test. All specimens failed due to the graft pulling out of the tibial tunnel. However, the ultimate failure load was reported to be significantly higher for the dilated tibial tunnels. Testing methodology makes it difficult to compare the results of this study with earlier studies; however, based on the literature, the benefits of compaction drilling or serial dilation seem to be marginal at best and probably do not justify the extra costs and operating time.
Although it is generally agreed that interference screws should be inserted on the cancellous side of BTB grafts, controversy exists regarding placement of tibial interference screws used to fix multistrand hamstring tendon grafts. Soft tissue grafts may be fixed by inserting the screw on the side (eccentrically) or down the center (concentrically) of the graft strands. Concentric screw placement maximizes contact between the graft strands and the bone tunnel wall, providing a greater surface area for healing. Simonian et al49 investigated the effect of screw eccentric versus concentric placement on initial fixation properties using human hamstring tendon grafts fixed in a polyurethane foam model. There were no differences in the ultimate failure load or slippage between the two screw positions. Shino and Pflaster50 investigated the effect of eccentric versus concentric screw placement on the initial fixation properties of four-strand hamstring tendon grafts fixed in the proximal tibia of paired human cadaveric knees (average age 51 years, range 49–54 years). There were no significant differences in stiffness, yield load, ultimate failure load, or slippage between the two screw positions.
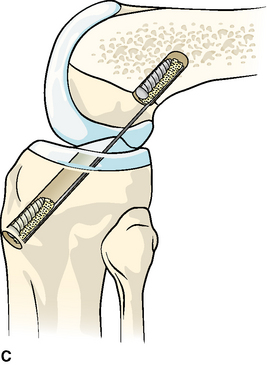
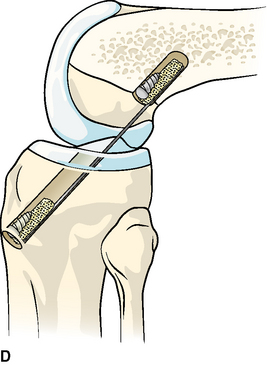
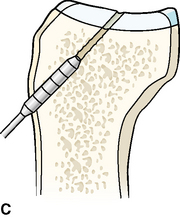
Alternative Intratunnel Tibial Fixation Techniques
The stimulus for the development of alternative intratunnel tibial fixation techniques for soft tissue ACL grafts arose from the desire to decrease slippage and the high rate of fixation failure reported with interference screws under cyclical loading conditions, to eliminate or reduce the need for supplemental tibial fixation, and to improve soft tissue–to-bone healing at the graft fixation sites.39,42,51 The IntraFix (DePuy Mitek, Norwood, MA) was designed to individually capture each of the four strands of a soft tissue graft in a separate compartment using a plastic sheath and to achieve direct compression of each of the graft strands against the bone tunnel wall by the insertion of a tapered screw into the central chamber of the plastic sheath.52 In a porcine tibia model using human hamstring tendon grafts, Kousa et al53 demonstrated that the IntraFix had the highest load failure load (1309 ± 302 N) and stiffness (267 ± 36 N/mm) and the least amount of slippage (1.5 mm) after cyclical loading compared with two cortical fixation techniques and three other interference screw fixation techniques.
The GTS System (Graft Tunnel Solution) (Smith & Nephew Endoscopy, Andover, MA) is an intratunnel tibial fixation technique that positions a poly-L-lactic acid (PLLA)-tapered, fine-pitch screw concentrically within the four-strand soft tissue graft.54 The screw features a tapered design and shorter thread distance, which enhances compression of the soft tissue graft in cancellous bone. The Graft Sleeve is a three-lumen, woven, nonabsorbable polypropylene (PPE) mesh graft sleeve that organizes the four-strand soft tissue graft in the tibial tunnel. The Graft Sleeve prevents graft twisting during screw insertion, which helps maintain equal tension in the four graft strands; maximizes bone-tendon contact, which enhances healing; and provides better compression of each ligament strand against the bone tunnel wall while protecting the graft strands from screw damage. Cyclical testing followed by single LTF testing of the Graft Sleeve and Tapered Screw and IntraFix has been performed using human doubled gracilis and semitendinosus tendon grafts (DGST) in the proximal tibia of calf bone (2 years or younger) with BMD similar to that of the proximal tibia in young humans. There were no significant differences in slippage, ultimate failure load, or stiffness between the two devices.
1 Lambert KL. Vascularized patellar tendon graft with rigid internal fixation for anterior cruciate ligament insufficiency. Clin Orthop. 1983;172:85-89.
2 Kurosaka M, Yoshiya S, Andrish JT. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15:225-229.
3 Steiner ME, Hecker AT, Brown CHJr, et al. Anterior cruciate ligament graft fixation: comparison of hamstring and patellar tendon grafts. Am J Sports Med. 1994;22:240-247.
4 Bach BRJr, Tradonsky S, Bojchuk J, et al. Arthroscopically assisted anterior cruciate ligament reconstruction using patellar tendon autograft. Five-to nine-year follow-up evaluation. Am J Sports Med. 1998;26:20-29.
5 Pinczewski L. Endoscopic ACL reconstruction utilizing a quadrupled hamstring tendon autograft with direct RCI interference screw fixation. Presented at Lecture/Laboratory Session of RCI Screw, Smith & Nephew Donjoy, Columbus, GA, Feb 1996. 1996.
6 Morrison JB. Function of the knee joint in various activities. Biomed Eng. 1969;4:573-580.
7 Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970;3:51-61.
8 Noyes FR, Butler DL, Grood E, et al. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg. 1984;66A:344-352.
9 Cooper DE, Deng XH, Burstein AL, et al. The strength of central third patellar tendon graft: a biomechanical study. Am J Sports Med. 1993;21:818-823.
10 Hamner DL, Brown CH, Steiner ME, et al. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg. 1999;81A:549-557.
11 Brand JC, Weiler A, Caborn DNM, et al. Graft fixation in cruciate ligament reconstruction. Am J Sports Med. 2000;28:761-774.
12 Beynnon BD, Amis AA. In vitro testing protocols for the cruciate ligaments and ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 1998;6(suppl 1):S70-S76.
13 Weiss JA, Paulos LE. Mechanical testing of ligament fixation devices. Techn Orthop. 1999;14:14-21.
14 Brown GA, Pena F, Grontvedt T, et al. Fixation strength of interference screw fixation in bovine, young human, and elderly human cadaver knee: influence of insertion torque, tunnel-bone block gap and interference. Knee Surg Sports Traumatol Arthrosc. 1996;3:238-244.
15 Aerssens J, Boonen S, Lowet G, et al. Interspecies differences in bone composition, density, and quality: potential implications for in vivo bone research. Endocrinology. 1998;139:663-670.
16 Magen HE, Howell SM, Hull ML. Structural properties of six tibial fixation methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med. 1999;27:35-43.
17 Nurmi JT, Sievanen H, Kannus P, et al. Porcine tibia is a poor substitute for human cadaver tibia for evaluating interference screw fixation. Am J Sports Med. 2004;32:765-771.
18 Clancy WGJr, Narechania RG, Rosenberg TD, et al. Anterior and posterior cruciate ligament reconstruction in rhesus monkeys. A histological microangiographic and biomechanical analysis. J Bone Joint Surg. 1981;63A:1270-1284.
19 Walton M. Absorbable and metal interference screws: comparison of graft security during healing. Arthroscopy. 1999;15:818-826.
20 Rodeo SA, Arnoczky SP, Torzilli PA, et al. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg. 1993;75A:1795-1803.
21 Cassim A, Lobenhoffer P, Gerich T, et al. The fixation strength of the interference screw in anterior cruciate ligament replacement as a function of technique and experimental setup. Trans Ortho Res Soc. 1993;18:31.
22 Brand JCJr, Pienkowski D, Steenlage E, et al. Interference screw fixation strength of a quadrupled hamstring tendon graft is directly related to bone mineral density and insertion torque. Am J Sports Med. 2000;28:705-710.
23 Jarvinen TL, Nurmi JT, Sievanen H. Bone density and insertion torque as predictors of anterior cruciate ligament graft fixation strength. Am J Sports Med. 2004;32:1421-1429.
24 Reznik AM, Davis JL, Daniel DM. Optimizing interference fixation for cruciate ligament reconstruction. Trans Orthop Res Soc. 1990;15:519.
25 Kohn D, Rose C. Primary stability of interference screw fixation: influence of screw diameter and insertion torque. Am J Sports Med. 1994;22:334-338.
26 Hulstyn M, Fadale PD, Abate J, et al. Biomechanical evaluation of interference screw fixation in a bovine patellar bone-tendon-bone autograft complex for anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:417-424.
27 Brown CH, Hecker AT, Hipp JA, et al. The biomechanics of interference screw fixation of patellar tendon anterior cruciate ligament grafts. Am J Sports Med. 1993;21:880-886.
28 Butler JC, Branch TP, Hutton WC. Optimal graft fixation—the effect of gap size and screw size on bone plug fixation in ACL reconstruction. Arthroscopy. 1994;10:524-529.
29 Fithian DC, Daniel DM, Casanave A. Fixation in knee ligament repair and reconstruction. Oper Tech Orthop. 1992;2:63-70.
30 Black KP, Saunders MM, Stube KC, et al. Effects of interference fit screw length on tibial tunnel fixation for anterior cruciate ligament reconstruction. Am J Sports Med. 2000;28:846-849.
31 Pomeroy G, Baltz M, Pierz K, et al. The effects of bone plug length and screw diameter on the holding strength of bone-tendon-bone grafts. Arthroscopy. 1998;14:148-152.
32 Lemos MJ, Albert J, Simon T, et al. Radiographic analysis of femoral interference screw placement during ACL reconstruction: endoscopic versus open technique. Arthroscopy. 1993;9:154-158.
33 Dworsky BD, Jewell BF, Bach BR. Interference screw divergence in endoscopic anterior cruciate ligament reconstruction. Arthroscopy. 1996;12:45-49.
34 Jomha NM, Raso VJ, Leung P. Effect of varying angles on the pullout strength of interference screw fixation. Arthroscopy. 1993;9:580-583.
35 Pierz K, Baltz M, Fulkerson J. The effect of Kurosaka screw divergence on the holding strength of bone-tendon-bone grafts. Am J Sports Med. 1995;23:332-335.
36 Barber FA, Elrod BF, McGuire DA, et al. Preliminary results of an absorbable interference screw. Arthroscopy. 1995;11:537-548.
37 Weiler A, Windhagen HJ, Raschke MJ, et al. Biodegradable interference screw fixation exhibits pull-out force and stiffness similar to titanium screws. Am J Sports Med. 1998;26:119-128.
38 Kousa P, Järvinen TL, Kannus P, et al. Initial fixation strength of bioabsorbable and titanium interference screws in anterior cruciate ligament reconstruction: biomechanical evaluation by single cycle and cyclic loading. Am J Sports Med. 2001;29:420-425.
39 Brand JC, Caborn DNM, Johnson DL. Biomechanics of soft-tissue interference screw fixation of anterior cruciate ligament reconstruction. Orthopedics. 2003;26:432-439.
40 Weiler A, Hoffmann RF, Siepe CJ, et al. The influence of screw geometry on hamstring tendon interference fit fixation. Am J Sports Med. 2000;28:356-359.
41 Selby JB, Johnson DL, Hester P, et al. Effect of screw length on bioabsorbable interference screw fixation in a tibial bone tunnel. Am J Sports Med. 2001;29:614-619.
42 Harvey AR, Thomas NP, Amis AA. The effect of screw length and position on fixation of four-stranded hamstring grafts for anterior cruciate ligament reconstruction. Knee. 2003;10:97-102.
43 Steenlage E, Brand JCJr, Johnson DL, et al. Correlation of bone tunnel diameter with quadrupled hamstring graft fixation strength using a biodegradable interference screw. Arthroscopy. 2002;18:901-907.
44 Rittmeister ME, Noble PC, Bocell JRJr, et al. Interactive effects of tunnel dilation on the mechanical properties of hamstring grafts fixed in the tibia with interference screws. Knee Surg Sports Traumatol Arthrosc. 2001;9:267-271.
45 Nurmi JT, Kannus P, Sievänen H, et al. Compaction drilling does not increase the initial fixation strength of the hamstring tendon graft in anterior cruciate ligament reconstruction in a cadaver model. Am J Sports Med. 2003;31:353-358.
46 Nurmi JT, Kannus P, Sievänen H, et al. Interference screw fixation of soft tissue grafts in anterior cruciate ligament reconstruction: part 1. Effect of tunnel compaction by serial dilators versus extraction drilling on the initial fixation strength. Am J Sports Med. 2004;32:411-417.
47 Cain EL, Phillips BB, Charlebois SJ, et al. Effect of tibial tunnel dilation on pullout strength of semitendinosus-gracilis graft in anterior cruciate ligament reconstruction. Orthopedics. 2005;28:779-783.
48 Steiner ME, Hecker AT, Brown CHJr, et al. Anterior cruciate ligament graft fixation: comparison of hamstring and patellar tendon grafts. Am J Sports Med. 1994;22:240-246.
49 Simonian PT, Sussmann PS, Baldini TH, et al. Interference screw position and hamstring graft location for anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:459-464.
50 Shino K, Pflaster DS. Comparison of eccentric and concentric screw placement for hamstring graft fixation in the tibial tunnel. Knee Surg Sports Traumatol Arthrosc. 2000;8:73-75.
51 Magen HE, Howell SM, Hull ML. Structural properties of six tibial fixation methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med. 1999;27:35-43.
52 Sklar JH, Brown CHJr. Soft tissue anterior cruciate ligament reconstruction with the IntraFix tibial fastener. Tech Orthop. 2005;20:283-289.
53 Kousa P, Jarvinen TL, Vihavainen M, et al. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med. 2003;31:182-188.
54 Brown CHJr, Darwich N. Anterior cruciate ligament reconstruction using autogenous doubled gracilis and semitendinosus tendons with GTS sleeve and tapered screw tibial fixation. Tech Orthop. 2005;20:290-296.