Usually simple in appearance, but may rarely have internal debris, blood products, etc.
• MR: Usually well-defined fluid collection, which is T2WI hyperintense and T1WI hypointense
 in the surgical bed.
in the surgical bed.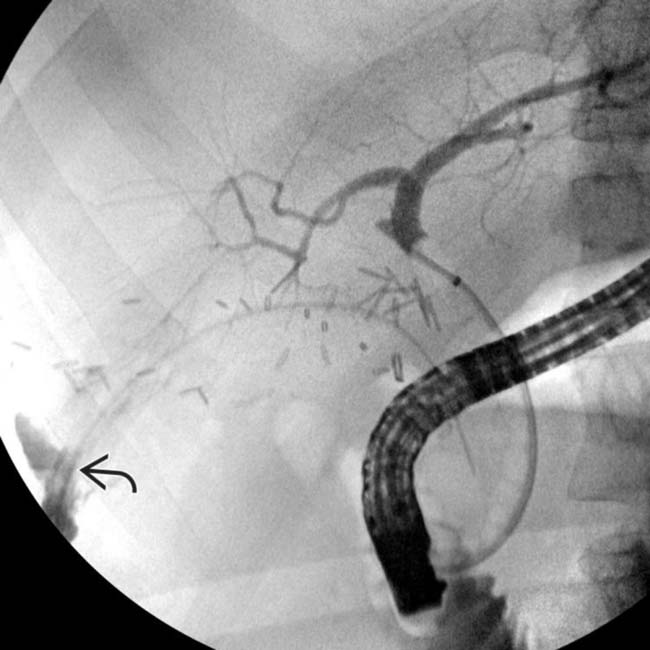
 of contrast into the biloma from the right hepatic lobe bile duct distribution. Unlike other imaging modalities, ERCP can definitively identify an active bile leak and confirm that a fluid collection represents a biloma.
of contrast into the biloma from the right hepatic lobe bile duct distribution. Unlike other imaging modalities, ERCP can definitively identify an active bile leak and confirm that a fluid collection represents a biloma.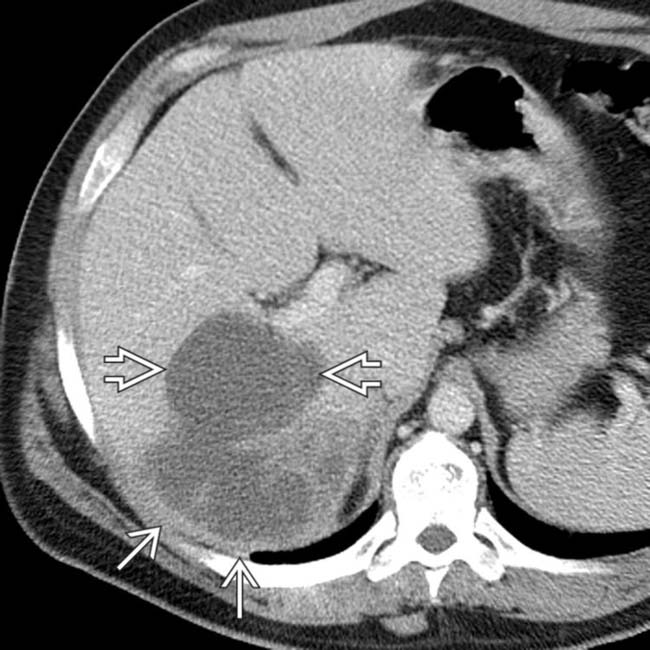
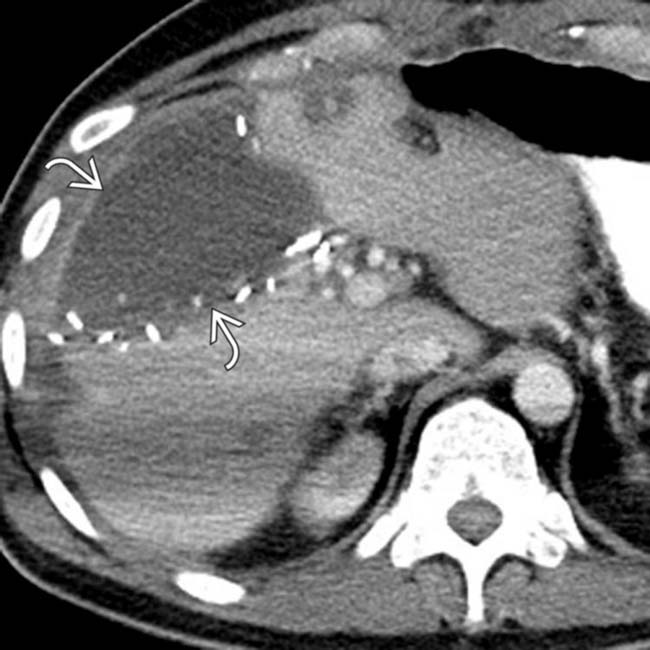
 and surrounding devascularized, infarcted liver
and surrounding devascularized, infarcted liver  .
.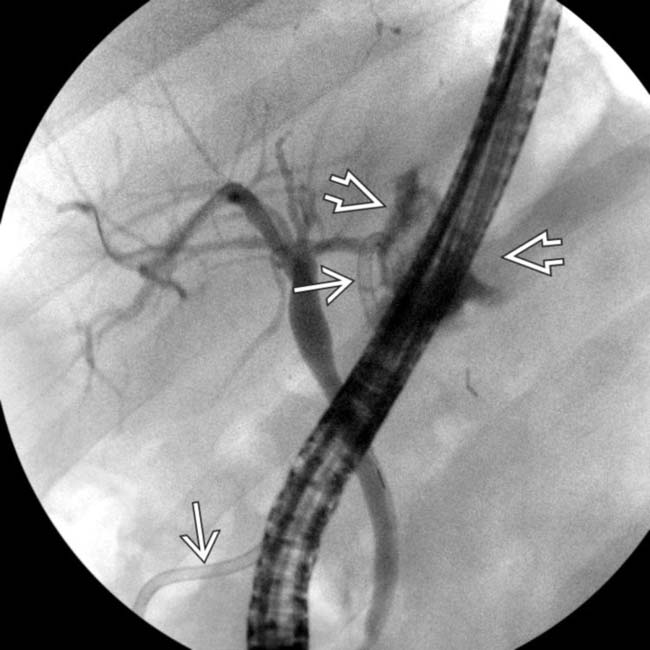
 into the biloma, and an appropriately positioned drain
into the biloma, and an appropriately positioned drain  . The biloma completely resolved after percutaneous drainage and biliary stent placement.
. The biloma completely resolved after percutaneous drainage and biliary stent placement.IMAGING
General Features
MR Findings
• MRCP delineates relationship of biloma with adjacent biliary tree and anomalies in bile duct anatomy

 immediately adjacent to the hepaticojejunostomy. Given the proximity of the biliary anastomosis, a biloma was strongly suspected.
immediately adjacent to the hepaticojejunostomy. Given the proximity of the biliary anastomosis, a biloma was strongly suspected.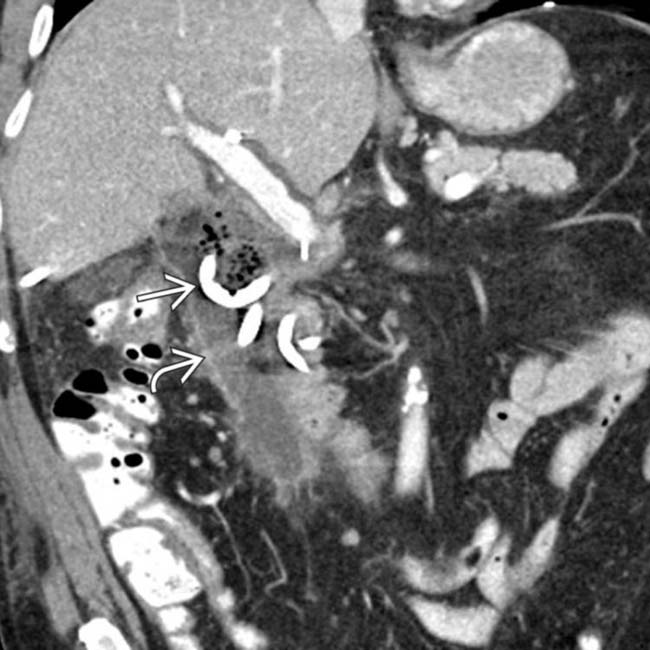
 into the collection
into the collection  , as there was concern for superinfection. The collection was found to have markedly elevated bilirubin levels, in keeping with a biloma.
, as there was concern for superinfection. The collection was found to have markedly elevated bilirubin levels, in keeping with a biloma.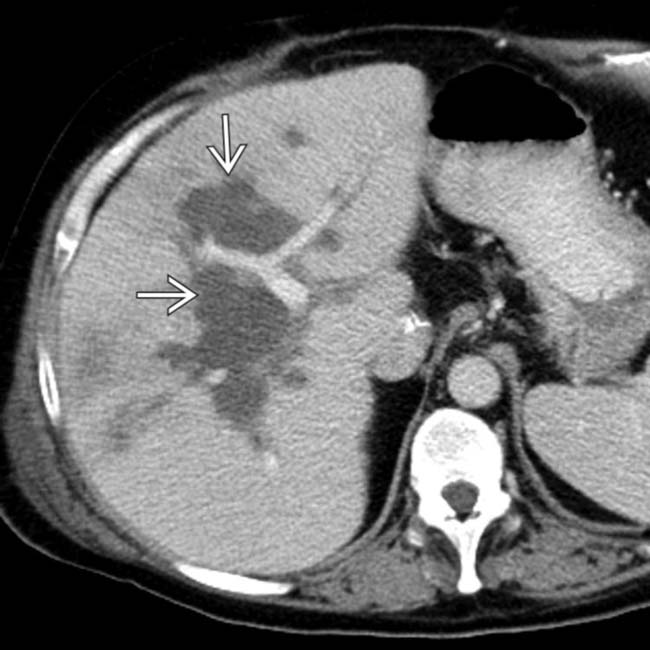
 with a branching configuration that parallels the bile ducts, representing a biloma due to arterial thrombosis.
with a branching configuration that parallels the bile ducts, representing a biloma due to arterial thrombosis.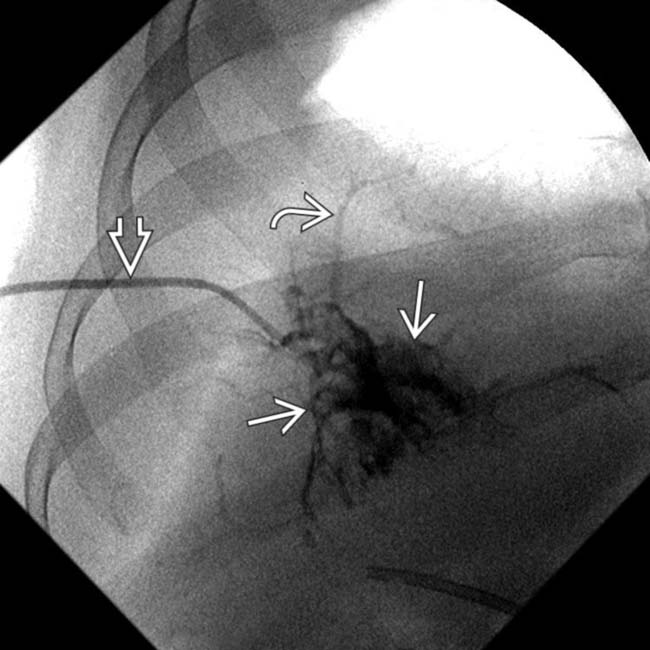
 placed into the biloma. Injection of contrast opacifies both the biloma
placed into the biloma. Injection of contrast opacifies both the biloma  and nondilated ducts
and nondilated ducts  , confirming communication between necrotic bile ducts and the biloma.
, confirming communication between necrotic bile ducts and the biloma.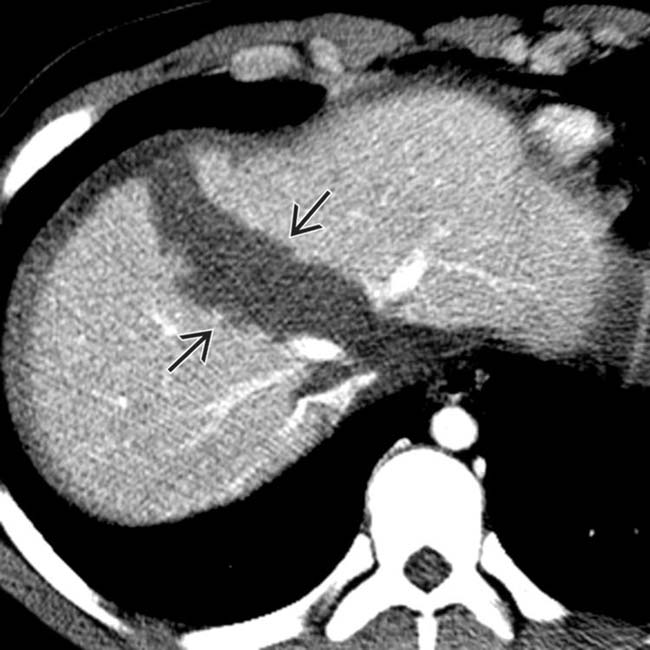
 traversing the liver in the plane of the main lobar fissure.
traversing the liver in the plane of the main lobar fissure.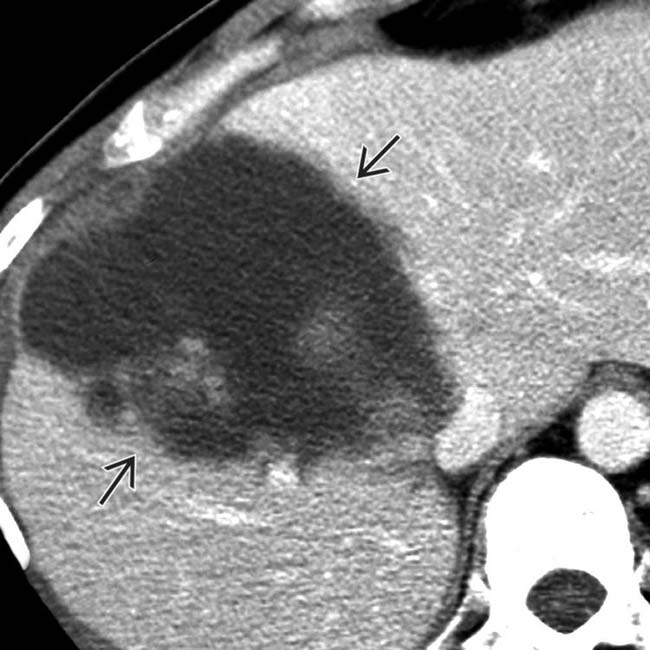
 at the site of the previous hepatic fracture. Post-traumatic bilomas occur because of disrupted intrahepatic bile ducts and bile leakage into lacerations/hematomas.
at the site of the previous hepatic fracture. Post-traumatic bilomas occur because of disrupted intrahepatic bile ducts and bile leakage into lacerations/hematomas.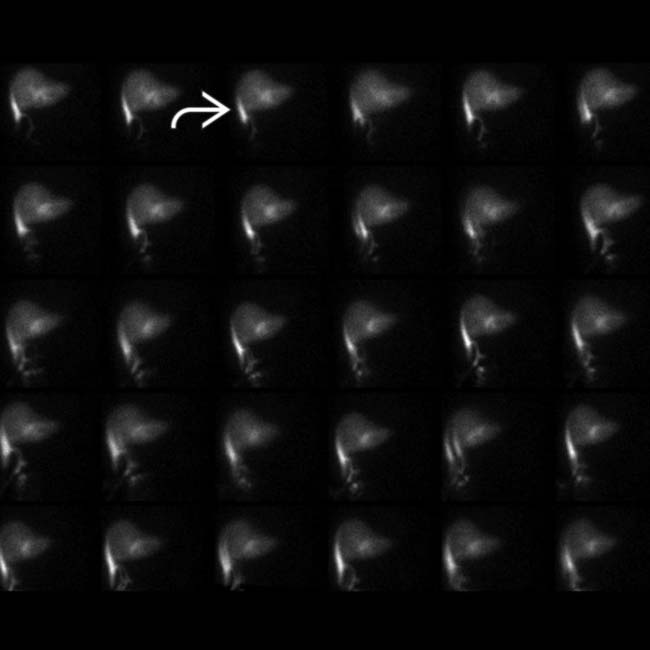
 and none within the small bowel, compatible with a bile leak.
and none within the small bowel, compatible with a bile leak.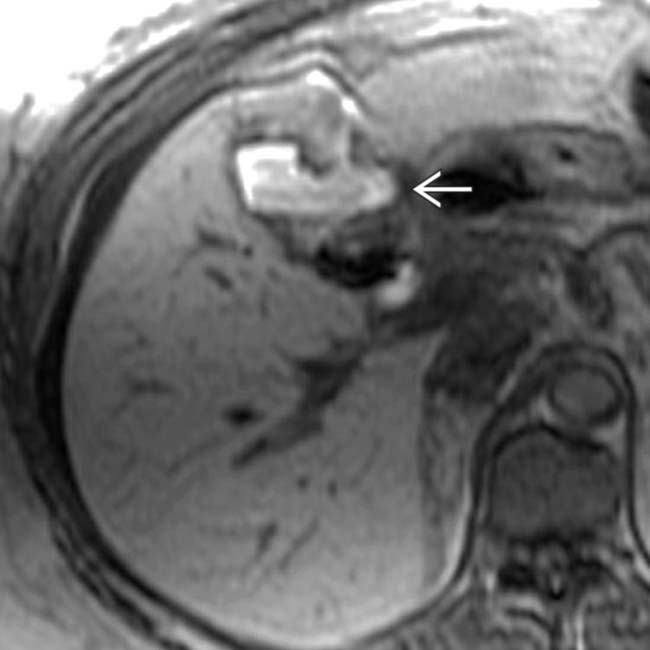
 within the gallbladder fossa post cholecystectomy. MR hepatobiliary agents may be particularly useful for delineating biliary injuries and bilomas.
within the gallbladder fossa post cholecystectomy. MR hepatobiliary agents may be particularly useful for delineating biliary injuries and bilomas.
 along the surgical margin of the liver.
along the surgical margin of the liver.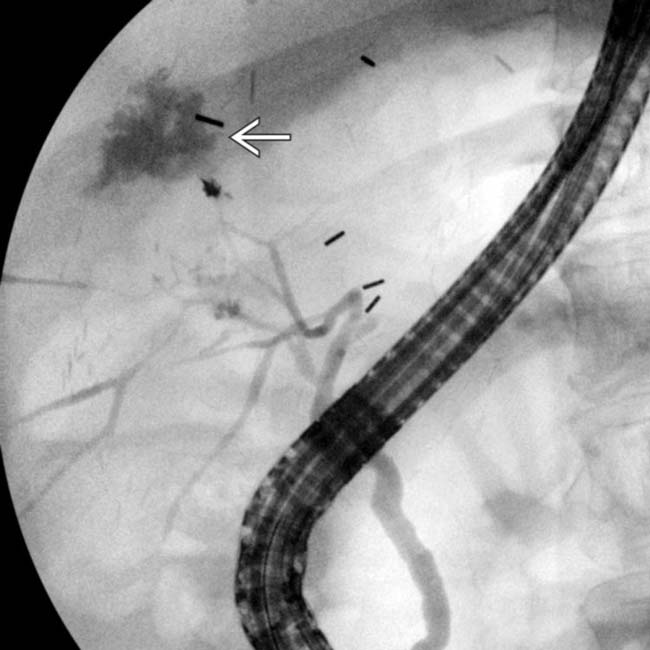
 . Asymptomatic post-traumatic/operative bilomas often resolve without intervention. Biloma growth, pain, and leukocytosis should, however, prompt treatment. This biloma was successfully treated by percutaneous drainage and antibiotics.
. Asymptomatic post-traumatic/operative bilomas often resolve without intervention. Biloma growth, pain, and leukocytosis should, however, prompt treatment. This biloma was successfully treated by percutaneous drainage and antibiotics.
 . A CECT performed 1 month prior showed a thrombosed hepatic artery and small hepatic arterial collaterals.
. A CECT performed 1 month prior showed a thrombosed hepatic artery and small hepatic arterial collaterals.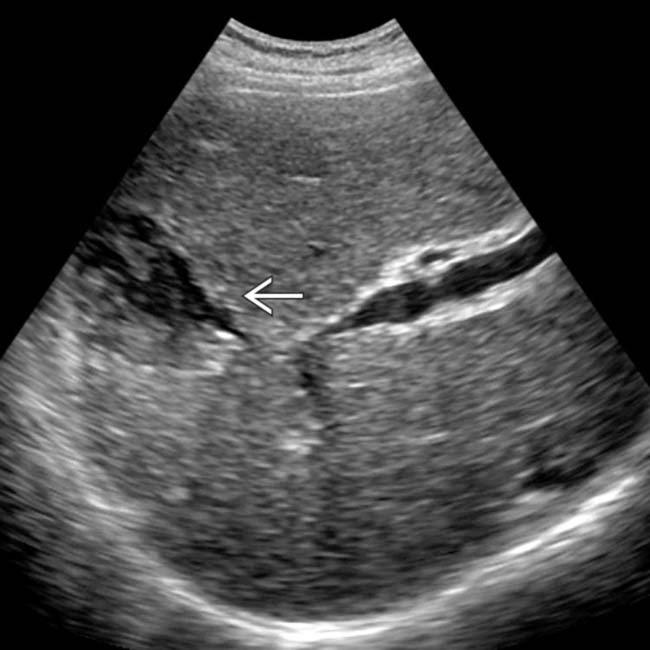
 . Liver transplant bilomas are typically due to hepatic arterial stenoses/thromboses. Biliary ischemia leads to bile duct necrosis, sloughing, and intrahepatic bilomas.
. Liver transplant bilomas are typically due to hepatic arterial stenoses/thromboses. Biliary ischemia leads to bile duct necrosis, sloughing, and intrahepatic bilomas.
 abutting the liver immediately adjacent to a recently created biliary-enteric anastomosis. The location of this collection raises strong suspicion for a biloma due to bile leak from the anastomosis.
abutting the liver immediately adjacent to a recently created biliary-enteric anastomosis. The location of this collection raises strong suspicion for a biloma due to bile leak from the anastomosis.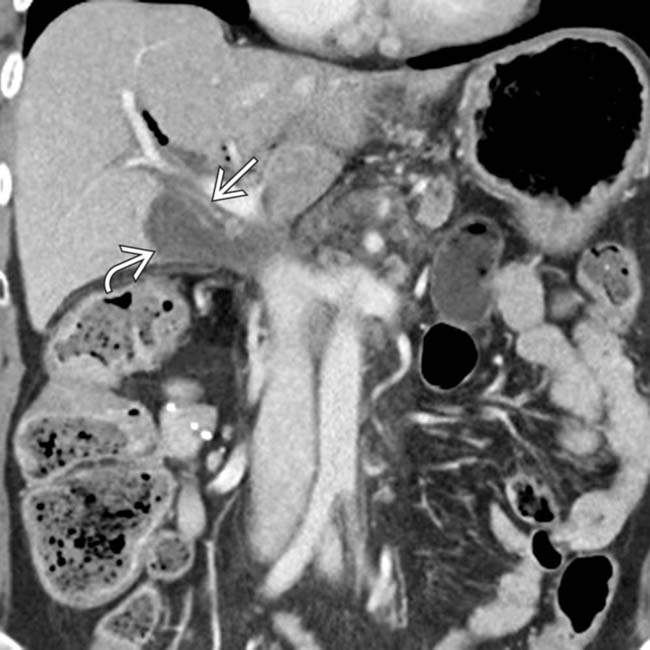
 to be immediately adjacent to the bile duct remnant
to be immediately adjacent to the bile duct remnant  . A drain was placed and the bile leak resolved over time.
. A drain was placed and the bile leak resolved over time.
 of fluid with dependent debris. In the setting of dysfunction of a liver allograft, this is very suggestive of a biloma due to biliary necrosis secondary to hepatic artery stenosis or thrombosis. The finding of hepatic artery stenosis was confirmed on ultrasound (not shown).
of fluid with dependent debris. In the setting of dysfunction of a liver allograft, this is very suggestive of a biloma due to biliary necrosis secondary to hepatic artery stenosis or thrombosis. The finding of hepatic artery stenosis was confirmed on ultrasound (not shown).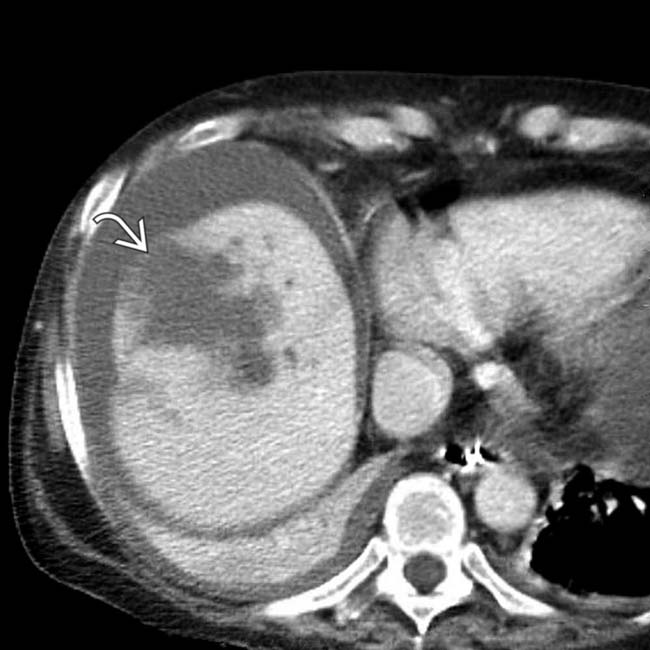
 , which was thought to communicate with the dilated biliary tree, in keeping with a biloma.
, which was thought to communicate with the dilated biliary tree, in keeping with a biloma.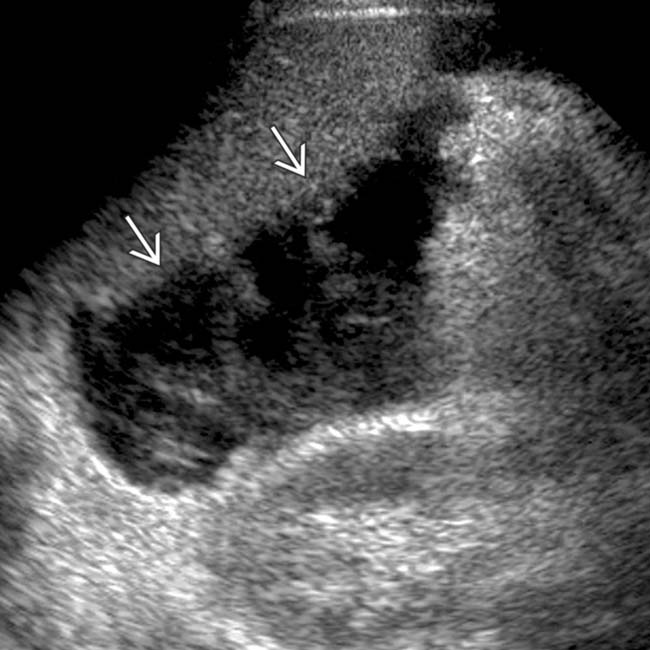
 with low-level echoes and mass effect in the Morrison pouch between the caudal margin of the liver and the upper pole of the kidney.
with low-level echoes and mass effect in the Morrison pouch between the caudal margin of the liver and the upper pole of the kidney.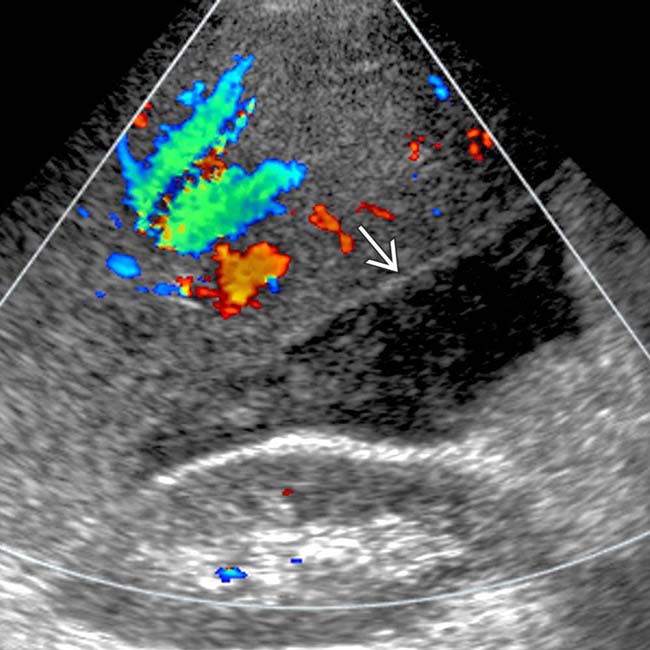
 ; needle aspiration revealed an infected biloma.
; needle aspiration revealed an infected biloma.
 , post radiofrequency ablation.
, post radiofrequency ablation.
 . Aspiration confirmed an infected biloma. Post-ablation bilomas occur because of thermal injury to intrahepatic ducts and bile leakage. Most post-ablation bilomas are asymptomatic.
. Aspiration confirmed an infected biloma. Post-ablation bilomas occur because of thermal injury to intrahepatic ducts and bile leakage. Most post-ablation bilomas are asymptomatic.
 in the left hepatic lobe, strongly suggestive of an infected biloma. The biloma was drained via CT-guided catheter placement with resolution of the biloma and symptoms.
in the left hepatic lobe, strongly suggestive of an infected biloma. The biloma was drained via CT-guided catheter placement with resolution of the biloma and symptoms.



































