Pericholecystic free fluid, intraluminal or pericholecystic hematoma, or GB wall thickening
 Poor definition of GB wall, abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, suggest GB perforation
Poor definition of GB wall, abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, suggest GB perforation• Bile duct injuries
 Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
 Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture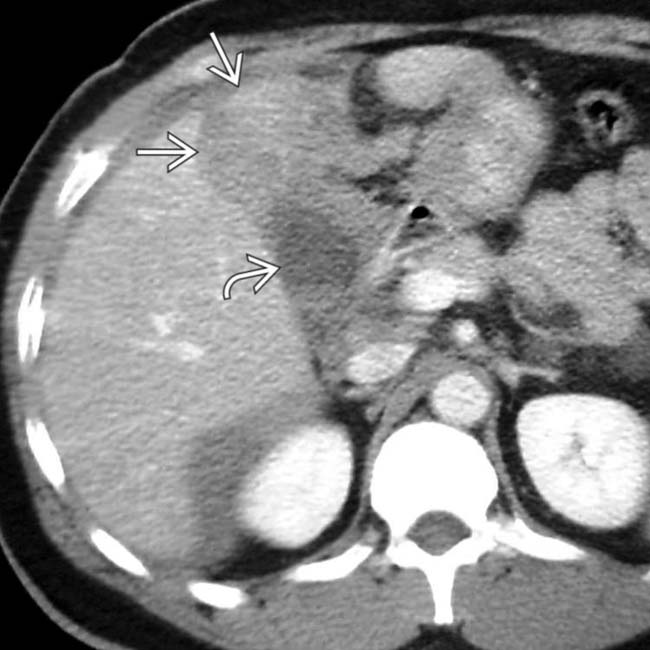
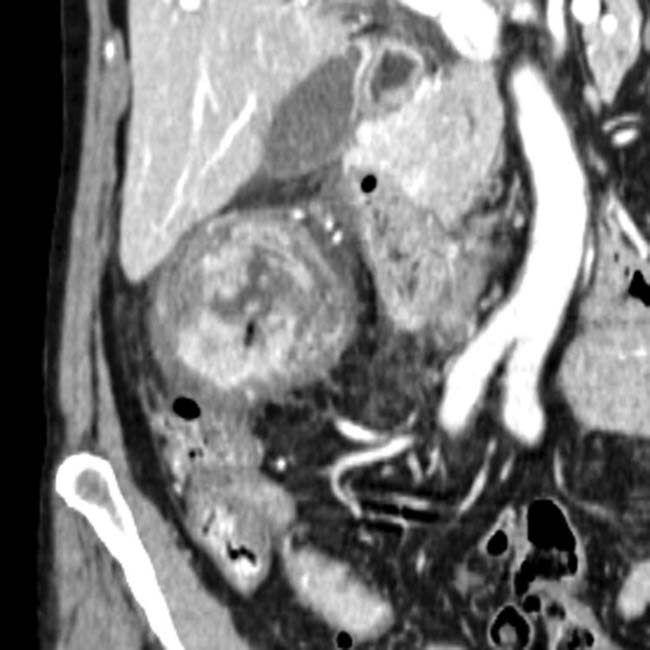
 separating the gallbladder
separating the gallbladder  from its normal location in the gallbladder fossa. The patient was taken to surgery where the gallbladder was found to be “avulsed” from its hepatic attachment and leaking bile.
from its normal location in the gallbladder fossa. The patient was taken to surgery where the gallbladder was found to be “avulsed” from its hepatic attachment and leaking bile.
 immediately adjacent to a surgical clip
immediately adjacent to a surgical clip  , in keeping with an iatrogenic stricture. The stricture in this case ultimately required hepaticojejunostomy.
, in keeping with an iatrogenic stricture. The stricture in this case ultimately required hepaticojejunostomy.
 and small hemoperitoneum. The depth of the laceration raised concern for biliary transection. The patient developed signs of bile peritonitis.
and small hemoperitoneum. The depth of the laceration raised concern for biliary transection. The patient developed signs of bile peritonitis.
 . The patient was successfully treated with biliary stenting without surgery. The biliary and hepatic injuries resolved.
. The patient was successfully treated with biliary stenting without surgery. The biliary and hepatic injuries resolved.IMAGING
General Features
• Location
 Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
 Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
– Most common injury is common duct transection (common duct mistaken for cystic duct during cholecystectomy)
CT Findings
• Gallbladder injury
 Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging
Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging
 Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury
Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury
 Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging
Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury
Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury• Bile duct injuries
 Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
 Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
• Helical CT cholangiography (after IV administration of biliary contrast material) to verify and localize bile duct leakage
• Presence of biliary dilatation, configuration of injured bile duct, and ancillary abdominal findings
PATHOLOGY
General Features
• Etiology
 Trauma: Can result from blunt or penetrating injuries
Trauma: Can result from blunt or penetrating injuries
 Trauma: Can result from blunt or penetrating injuries
Trauma: Can result from blunt or penetrating injuries
– Tend to result from significant trauma with other injuries frequent (especially liver, spleen, and duodenum)
– Most commonly injured site in biliary tree is GB
 GB injuries range in severity, including contusion, laceration, perforation, and GB avulsion (separation of GB from GB fossa)
GB injuries range in severity, including contusion, laceration, perforation, and GB avulsion (separation of GB from GB fossa)
 Isolated injury to GB rare due to protection from rib cage and liver, so almost always associated with other significant traumatic injuries
Isolated injury to GB rare due to protection from rib cage and liver, so almost always associated with other significant traumatic injuries
 GB injuries range in severity, including contusion, laceration, perforation, and GB avulsion (separation of GB from GB fossa)
GB injuries range in severity, including contusion, laceration, perforation, and GB avulsion (separation of GB from GB fossa) Isolated injury to GB rare due to protection from rib cage and liver, so almost always associated with other significant traumatic injuries
Isolated injury to GB rare due to protection from rib cage and liver, so almost always associated with other significant traumatic injuriesCLINICAL ISSUES
Presentation
• Most common signs/symptoms
 Virtually all patients with traumatic bile duct injury have other significant injuries that require attention
Virtually all patients with traumatic bile duct injury have other significant injuries that require attention
 Virtually all patients with traumatic bile duct injury have other significant injuries that require attention
Virtually all patients with traumatic bile duct injury have other significant injuries that require attention
Treatment
• Minor bile duct injuries (including many intrahepatic ductal injuries) usually treated conservatively with ERCP stent placement or biliary drainage catheter to divert bile away from site of injury and allow time for healing
• More severe injuries require surgical treatment (usually Roux-en-Y hepaticojejunostomy) after ERCP (or PTC) to assess injury and plan operative repair
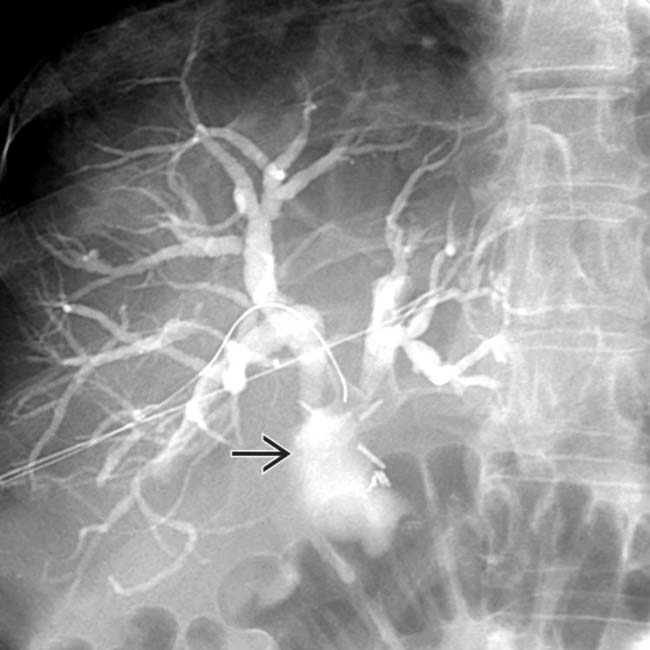
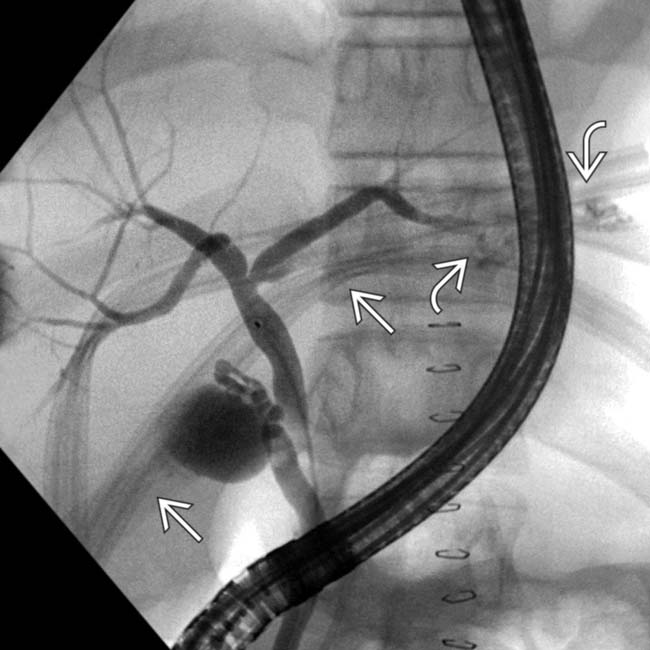
 , immediately adjacent to surgical clips, in keeping with an iatrogenic bile duct transection.
, immediately adjacent to surgical clips, in keeping with an iatrogenic bile duct transection.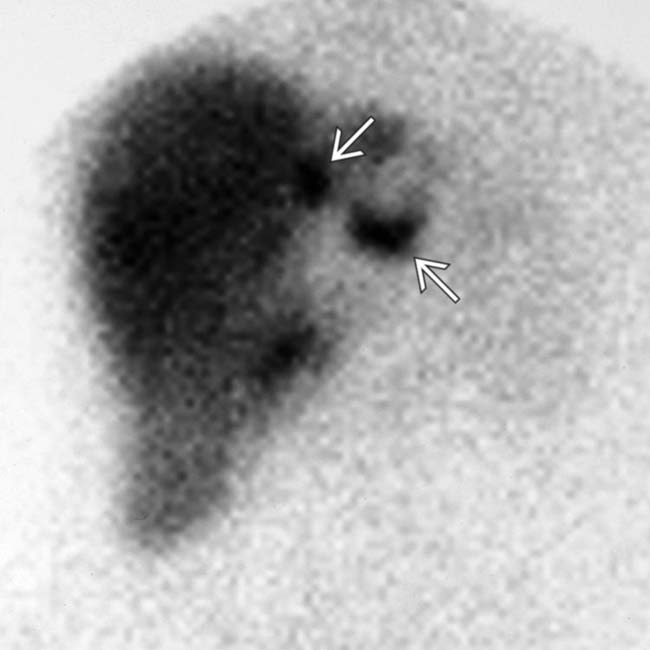
 outside of the biliary tree due to bile extravasation in a patient who had prior blunt trauma. HIDA scans are very sensitive and specific for bile leaks.
outside of the biliary tree due to bile extravasation in a patient who had prior blunt trauma. HIDA scans are very sensitive and specific for bile leaks.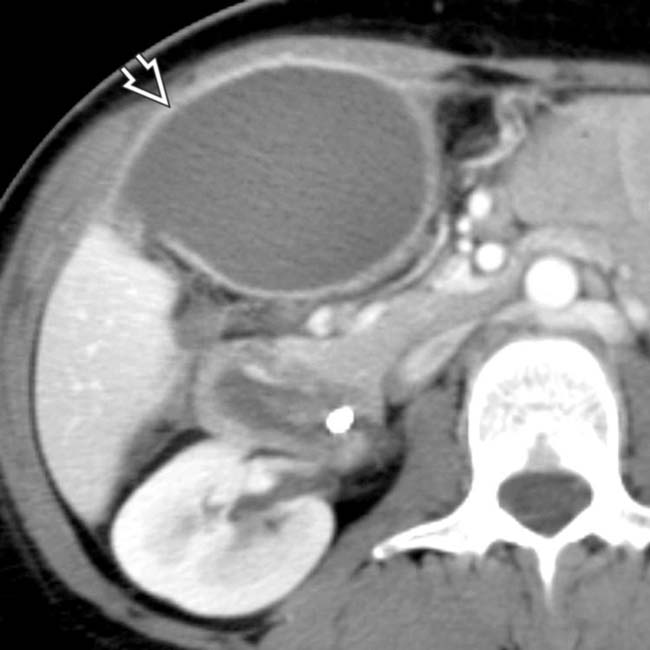
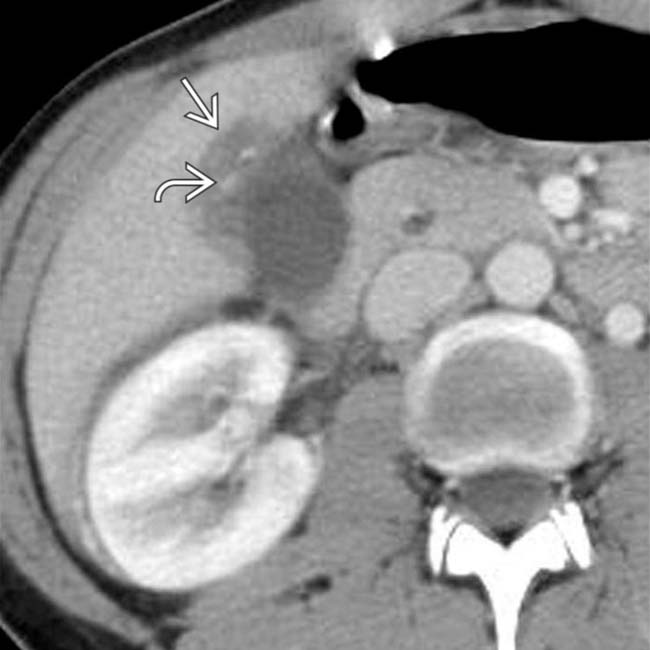
 in the gallbladder fossa, subsequently confirmed to be a biloma based on ultrasound-guided needle aspiration.
in the gallbladder fossa, subsequently confirmed to be a biloma based on ultrasound-guided needle aspiration.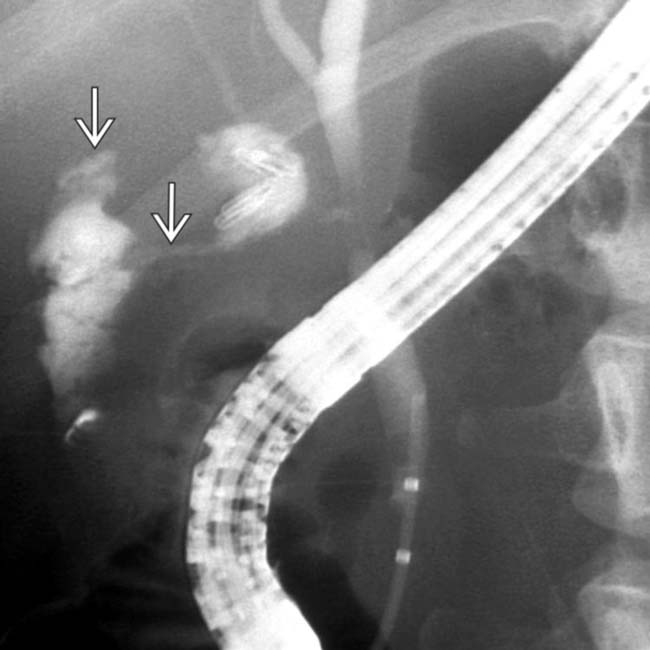
 from the cystic duct remnant. Sphincterotomy was performed, and a plastic biliary stent was placed. The bile leak resolved, and the stent was removed subsequently without complication.
from the cystic duct remnant. Sphincterotomy was performed, and a plastic biliary stent was placed. The bile leak resolved, and the stent was removed subsequently without complication.
 and intraperitoneal free fluid. There is heterogeneous fluid and hematoma around the pancreatic head
and intraperitoneal free fluid. There is heterogeneous fluid and hematoma around the pancreatic head  , near the expected position of the common bile duct.
, near the expected position of the common bile duct.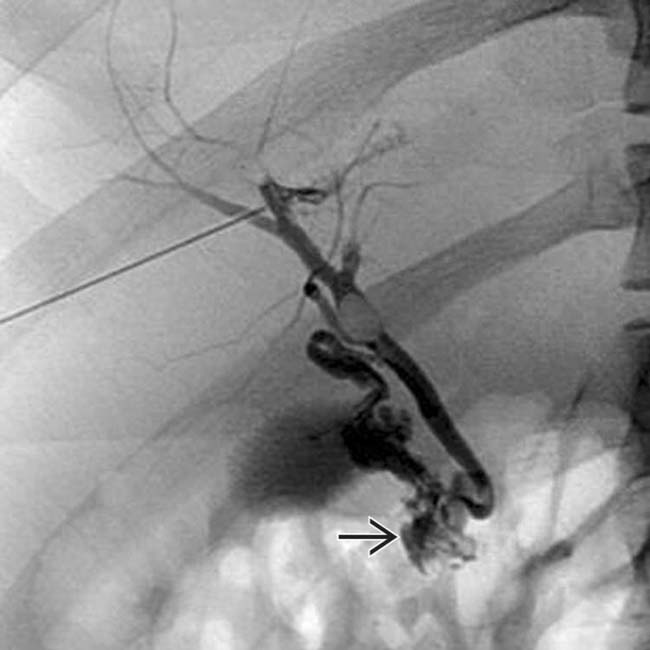
 .
.
 with subtle active extravasation
with subtle active extravasation  of blood immediately adjacent to the gallbladder fossa. The gallbladder itself appears normally distended, suggesting that it is intact. At surgery, the gallbladder itself was intact, but it was “avulsed” from its hepatic attachments, which were the source of the active bleeding.
of blood immediately adjacent to the gallbladder fossa. The gallbladder itself appears normally distended, suggesting that it is intact. At surgery, the gallbladder itself was intact, but it was “avulsed” from its hepatic attachments, which were the source of the active bleeding.
 . The patient’s clinical history and the absence of hemoperitoneum strongly suggests a bile duct injury and hemobilia.
. The patient’s clinical history and the absence of hemoperitoneum strongly suggests a bile duct injury and hemobilia.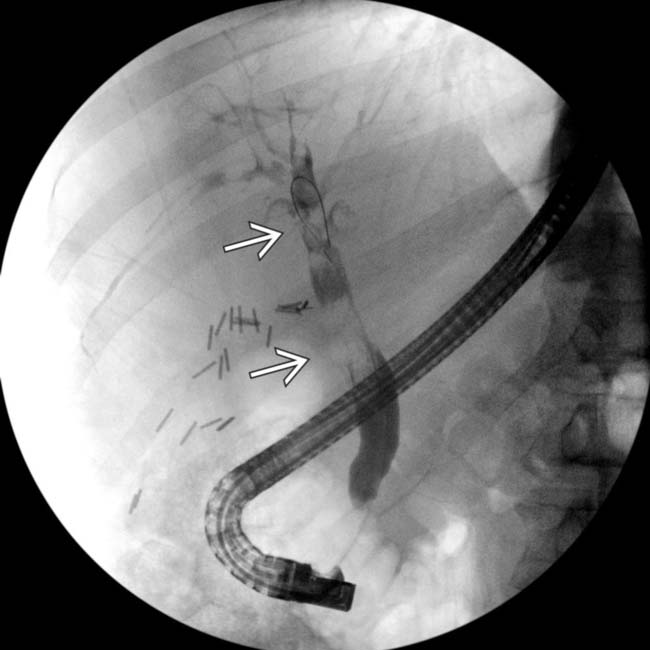
 within a slightly dilated common duct. The patient’s symptoms resolved after sphincterotomy and clot retrieval.
within a slightly dilated common duct. The patient’s symptoms resolved after sphincterotomy and clot retrieval.
 . ERCP (not shown) demonstrated a high-grade stricture adjacent to a clip. Post-cholecystectomy strictures may require surgical biliary diversion.
. ERCP (not shown) demonstrated a high-grade stricture adjacent to a clip. Post-cholecystectomy strictures may require surgical biliary diversion.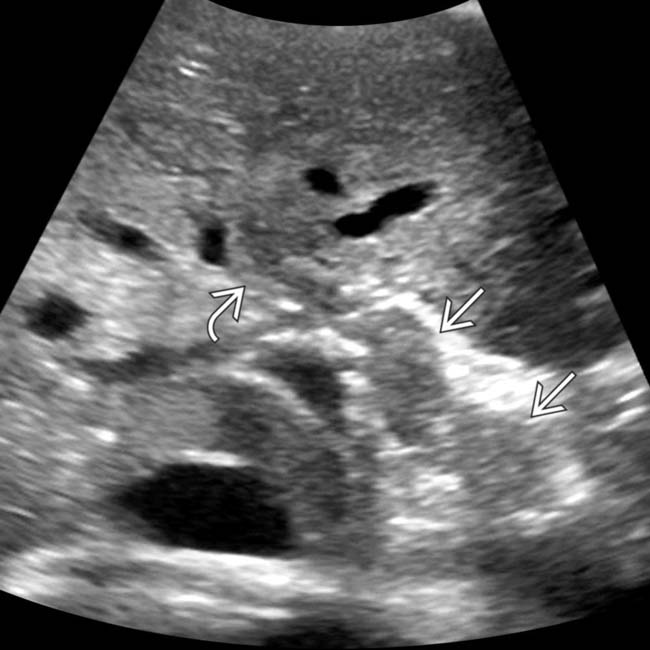
 and right bile duct
and right bile duct  . Clot was also shown within the gallbladder.
. Clot was also shown within the gallbladder.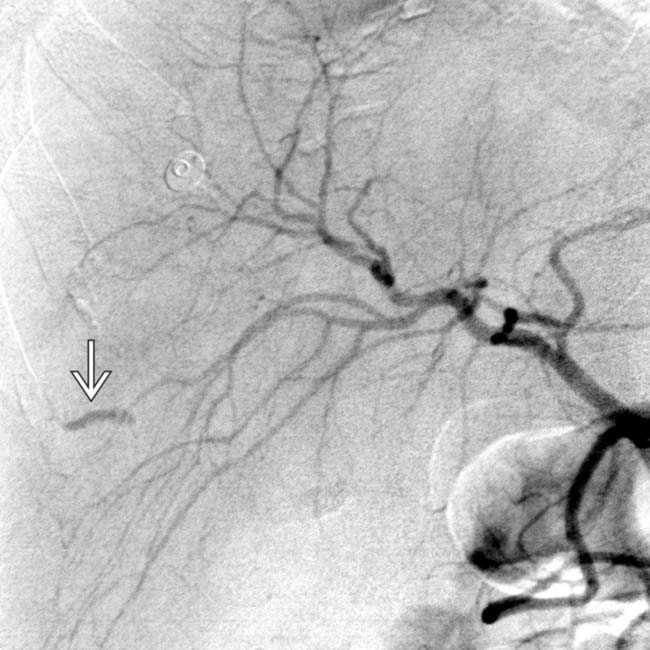
 . The fistula was successfully treated with coil embolization.
. The fistula was successfully treated with coil embolization.
 shows perihepatic bile
shows perihepatic bile  . Note the mild mass effect upon the liver and extensive fluid within the lesser sac
. Note the mild mass effect upon the liver and extensive fluid within the lesser sac  .
.
 shows a distal left bile duct injury and extravasated contrast
shows a distal left bile duct injury and extravasated contrast  . The leak was treated successfully with perihepatic drainage and left bile duct stent placement.
. The leak was treated successfully with perihepatic drainage and left bile duct stent placement.
















































































 with a spherical intrahepatic pseudoaneurysm
with a spherical intrahepatic pseudoaneurysm  . Endoscopy confirmed blood entering the duodenum via the ampulla of Vater, indicating hemobilia.
. Endoscopy confirmed blood entering the duodenum via the ampulla of Vater, indicating hemobilia.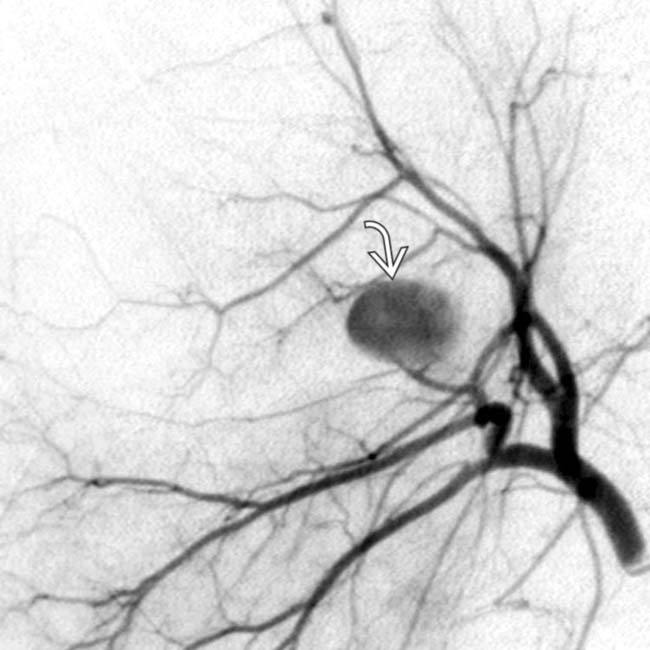
 , which was occluded by coil embolization. The hemobilia also ceased following embolization.
, which was occluded by coil embolization. The hemobilia also ceased following embolization.