Left hepatic duct formed by segmental branches from segments II-IV
 Right hepatic duct has 2 branches, including a horizontally oriented anterior branch draining segments V and VIII and a vertically oriented posterior branch draining segments VI and VII
Right hepatic duct has 2 branches, including a horizontally oriented anterior branch draining segments V and VIII and a vertically oriented posterior branch draining segments VI and VII Only central intrahepatic ducts seen normally (measuring ≤ 3 mm): Visualization of ↑ intrahepatic ducts concerning for dilated ducts or strictures
Only central intrahepatic ducts seen normally (measuring ≤ 3 mm): Visualization of ↑ intrahepatic ducts concerning for dilated ducts or strictures• Most common variants



 , presumably a type 3 choledochal cyst or choledochocele. Also noted is aberrant drainage of the posterior lobe bile duct
, presumably a type 3 choledochal cyst or choledochocele. Also noted is aberrant drainage of the posterior lobe bile duct  into the common hepatic duct.
into the common hepatic duct.
IMAGING
General Features
• Normal biliary anatomy
 Right hepatic duct (which is typically relatively short) has 2 branches
Right hepatic duct (which is typically relatively short) has 2 branches
 Right hepatic duct (which is typically relatively short) has 2 branches
Right hepatic duct (which is typically relatively short) has 2 branches
– Anterior (ventrocranial) branch drains segments VI and VIII and has horizontal course extending lateral and towards right from right hepatic duct
• Most common variants
 Most common anatomic variants involve aberrant right hepatic duct
Most common anatomic variants involve aberrant right hepatic duct
 Most common anatomic variants involve aberrant right hepatic duct
Most common anatomic variants involve aberrant right hepatic duct
DIFFERENTIAL DIAGNOSIS
MRCP Artifacts and Pitfalls
• Respiratory motion artifacts
• Flow artifact
 Often within dilated duct (such as at point of cystic duct insertion) due to swirling or helical flow of bile
Often within dilated duct (such as at point of cystic duct insertion) due to swirling or helical flow of bile
 Often within dilated duct (such as at point of cystic duct insertion) due to swirling or helical flow of bile
Often within dilated duct (such as at point of cystic duct insertion) due to swirling or helical flow of bile• Susceptibility artifacts
 Susceptibility artifact from metallic foreign bodies (such as surgical clips, endovascular coils, stents, etc.) produces adjacent signal loss, potentially mimicking stone or filling defect within biliary tree
Susceptibility artifact from metallic foreign bodies (such as surgical clips, endovascular coils, stents, etc.) produces adjacent signal loss, potentially mimicking stone or filling defect within biliary tree
 Susceptibility artifact from metallic foreign bodies (such as surgical clips, endovascular coils, stents, etc.) produces adjacent signal loss, potentially mimicking stone or filling defect within biliary tree
Susceptibility artifact from metallic foreign bodies (such as surgical clips, endovascular coils, stents, etc.) produces adjacent signal loss, potentially mimicking stone or filling defect within biliary tree
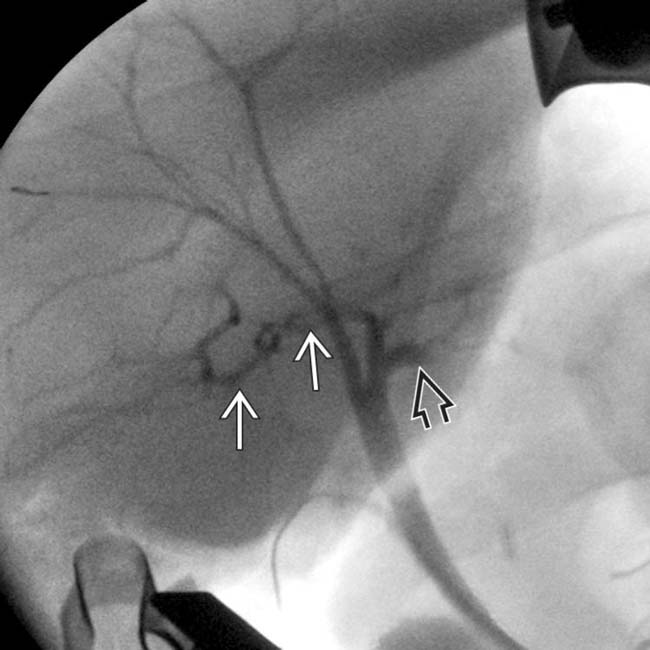
• Pulsatile vascular compression
 into the proximal left bile duct
into the proximal left bile duct  .
.
 arising from the left hepatic duct. This is the most common biliary anatomic variant, and is found in 13-19% of the population.
arising from the left hepatic duct. This is the most common biliary anatomic variant, and is found in 13-19% of the population.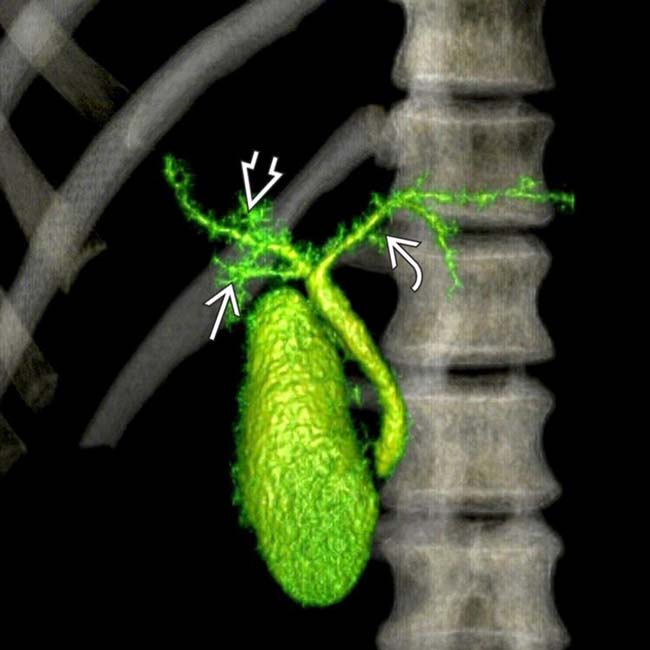
 , right anterior
, right anterior  , and right posterior
, and right posterior  ducts. This anatomy may require more complex biliary reconstruction during transplantation or may preclude donation.
ducts. This anatomy may require more complex biliary reconstruction during transplantation or may preclude donation.
 . There was no proximal ductal dilation. Flow artifacts like these are more common when using single-shot technique.
. There was no proximal ductal dilation. Flow artifacts like these are more common when using single-shot technique.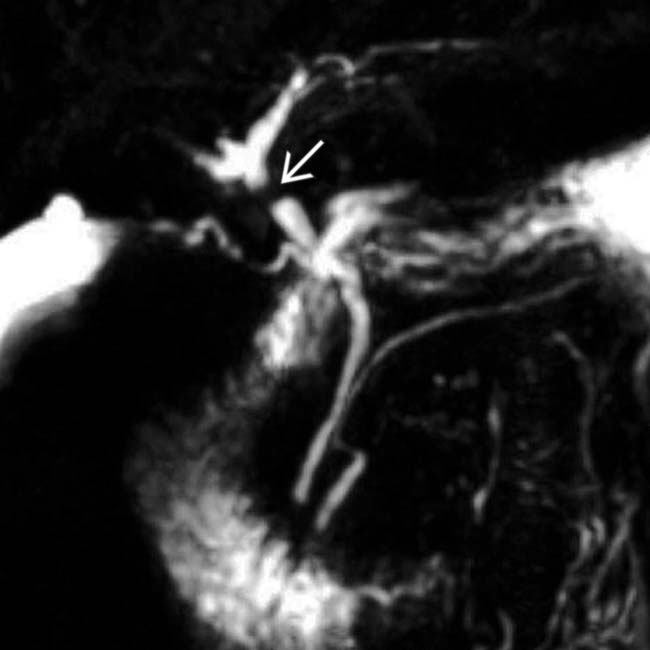
 in the common hepatic duct that simulates a stone. Note the absence of dilation of the ducts upstream from this point.
in the common hepatic duct that simulates a stone. Note the absence of dilation of the ducts upstream from this point.
 into the proximal left hepatic duct. Note the pulsation artifact proximal to the bifurcation
into the proximal left hepatic duct. Note the pulsation artifact proximal to the bifurcation  and a motion-reconstruction artifact along the mid common duct
and a motion-reconstruction artifact along the mid common duct  .
.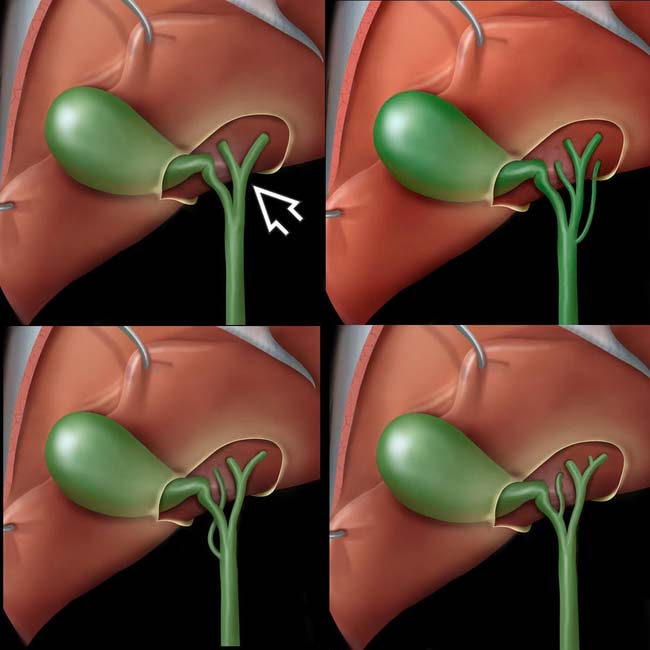
 . Variations are common, especially with aberrant insertion of the right posterior duct, as seen in the other 3 graphics. This may lead to inadvertent ligation or transection at surgery.
. Variations are common, especially with aberrant insertion of the right posterior duct, as seen in the other 3 graphics. This may lead to inadvertent ligation or transection at surgery.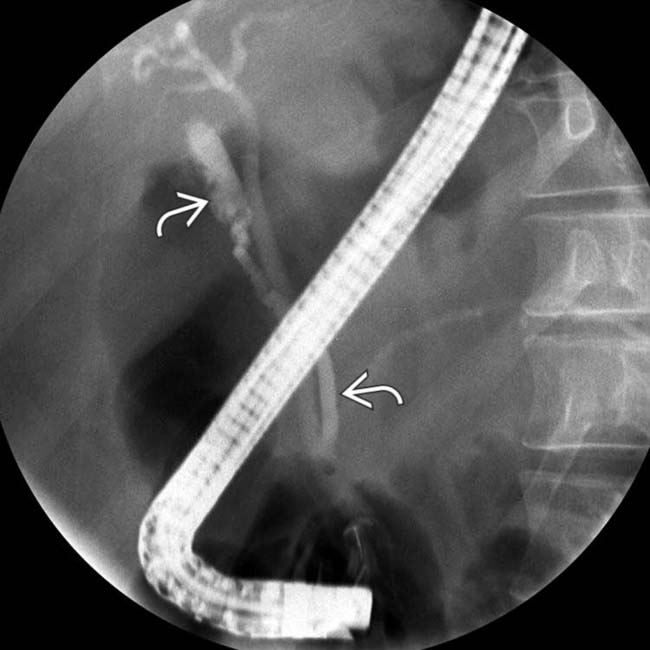
 into the distal common duct. Note the valves of Heister that impart a “corrugated” appearance of the cystic duct near its junction with the gallbladder.
into the distal common duct. Note the valves of Heister that impart a “corrugated” appearance of the cystic duct near its junction with the gallbladder.
 into the distal common bile duct
into the distal common bile duct  , very close to the ampulla.
, very close to the ampulla.
 into the medial inferior aspect of a choledochal cyst
into the medial inferior aspect of a choledochal cyst  .
.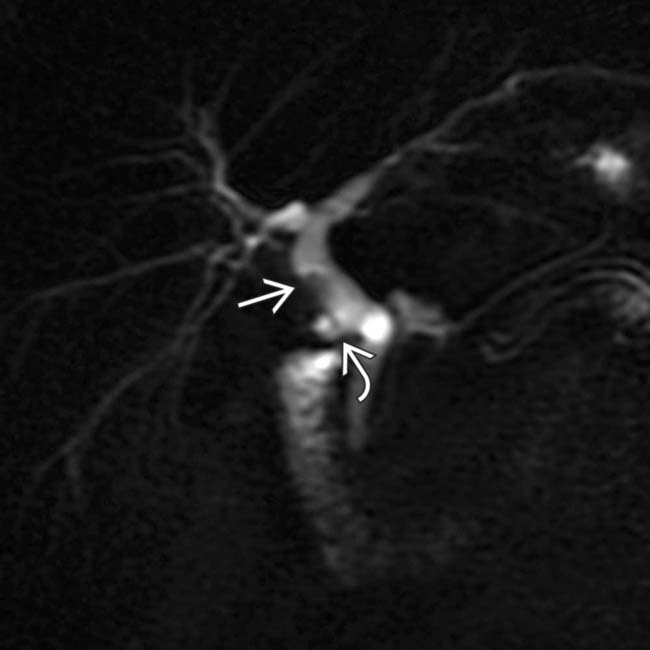
 , above the cystic duct stump
, above the cystic duct stump  . The signal void is caused by adjacent cholecystectomy clip susceptibility artifact. Note trifurcation of the common hepatic duct.
. The signal void is caused by adjacent cholecystectomy clip susceptibility artifact. Note trifurcation of the common hepatic duct.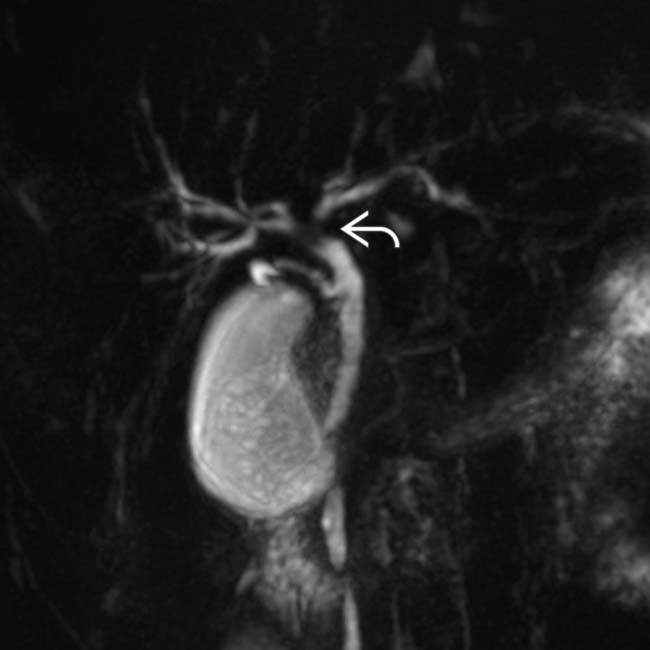
 due to pulsation artifact from the adjacent right hepatic artery. Note the absence of intrahepatic biliary ductal dilatation.
due to pulsation artifact from the adjacent right hepatic artery. Note the absence of intrahepatic biliary ductal dilatation.















































































 in the distal common duct that simulates a stone. However, a repeat film moments later showed a normal duct. This was caused by a spasm of the sphincter of Oddi.
in the distal common duct that simulates a stone. However, a repeat film moments later showed a normal duct. This was caused by a spasm of the sphincter of Oddi.
 in the proximal common duct with no proximal biliary dilatation, characteristic of pulsation artifact from the right hepatic artery.
in the proximal common duct with no proximal biliary dilatation, characteristic of pulsation artifact from the right hepatic artery.


