Chapter 215 Bilateral Locked Cervical Facets with Incomplete Myelopathy
Open versus Closed Reduction
Open Reduction
Background
Bilateral locked facets are an uncommon result of a traumatic hyperflexion injury.1–3 Collateral damage is substantial, with insults to the ligamentum flavum, anulus, apophyseal joints and supraspinous, interspinous, posterior longitudinal, and anterior longitudinal ligaments. The most commonly affected levels are C5-6 and C6-7, with adjacent fractures to the vertebral body, pedicle, or other structures in 40% to 60% of patients.1,4 Clinically, a strong majority of patients (65–87%) present with complete quadriplegia, followed by 13% to 25% presenting with incomplete spinal cord injury (SCI) and fewer than 10% presenting with no clinical signs of SCI.4,5 Disc herniation has been reported to be present in up to 80% of patients presenting with bilateral facet locking, and the presence of herniation in these patients has been a main focus of discussion when choosing between open and closed reduction.6 There is currently little argument that urgent decompression is warranted in the face of acute SCI, but the decision to utilize open versus closed reduction has remained contentious.7,8 We present a review of the literature and a case illustration to provide the reader with an understanding of the risks and benefits associated with each modality.
Use of Closed Reduction
Closed reduction, the most widely used method, has been shown to be effective in case series dating back several decades.9–11 Success rates using closed reduction have been reported as low as 40%, but have been as high as 100% in some studies; most recently, Yu et al. presented a series of 25 patients over 17 years with a success rate of 88%.12 The use of closed traction is inexpensive, historically necessitating only the use of a cervical spine radiograph series, clinical evaluation, and traction itself. In patients who have concomitant traumatic injuries such as pulmonary or cardiac contusions, traction may be the surgeon’s only recourse.
Enthusiasm for use of closed reduction must be tempered by the potential for catastrophic neurologic deterioration.13,14 A high rate of disc herniation is associated with bilateral locked facets, and it is postulated that herniation could increase the amount of spinal cord compression during closed reduction. This is thought to occur when the facet dislocation holds the canal open in an angulated position.14 Disc herniation has been reported in several clinical series and should stand as a serious consequence of closed reduction.4 If it is decided to employ closed traction, whether or not to obtain a prereduction MRI also must be considered. MRI offers the advantage of detecting disc herniation, thus eliminating an important element of risk from closed reduction.
In 2002, the indications for obtaining an MRI prior to reduction were discussed by Vaccaro et al.15 One argument for obtaining the MRI, as already described, is the possibility of serious and irreversible consequences, which may tip the clinical decision toward ruling out a disc herniation. Additionally, an MRI may be needed for the surgical stabilization of patients after closed reduction (discussed later in this section). Arguments against obtaining an MRI are based on the large number of patients who have undergone reduction successfully, as well as the very important consideration of the delay that may result if access to MRI is limited. Additionally, some reports indicate that while reduction often may precipitate disc herniation, these herniations may have no neurologic sequelae.16 It is argued that in the alert patient, frequent clinical examinations and vigilant monitoring may provide appropriate observation, and new neurologic signs can be readily detected.15 In 2002, the Congress of Neurological Surgeons recommended preoperative MRI in patients who are obtunded, those undergoing open posterior reduction, or those in whom attempts at closed reduction have failed.17 A recent study by Grauer et al. reinforced that the timing and influence of MRI on the management of cervical facet dislocations is highly variable among surgeons.18 While the debate over obtaining a prereduction MRI falls outside the scope of this chapter, it adds a level of complexity to the decision to utilize closed reduction.
Several outright complications can result from closed reduction, including overdistraction rostral to the level of the locked facets and worsening of fractures located elsewhere in the spine. Beyond these complications, it is important to consider the outcomes of patients who undergo closed reduction. While closed traction may provide decompression in many cases, these patients are likely eventually to require operative stabilization. Recognizing that surgical fusion is indicated after many successful closed reductions, failed closed reductions, and also open reductions, the long-term outcomes of those patients who underwent successful closed reduction with halo-vest immobilization should be examined. Sears and Fazl found that patients with facet subluxation had poor anatomic results in up to 77% of cases when a halo vest alone was used after closed reduction.19 When taken alone, this evidence would provide grounds against using closed reduction alone, but it is necessary to consider that in the criteria utilized to determine “poor anatomy,” instability was uncommon. Regardless, the results of this study suggest that since the ultimate result of closed reduction is a surgical fusion, surgery at presentation may be more appropriate than the time-consuming (and painful) process of closed reduction.
Use of Open Reduction
The surgical approach to bilateral locked facets allows several distinct advantages. As outlined earlier, the possibility that disc herniation may worsen neurologic status in closed reduction is a low-risk but high-stakes consequence.20 Using an anterior approach, an open surgical reduction allows resection of the disc prior to reduction and can essentially eliminate this risk. Moreover, direct surgical reduction and fixation avoids the often lengthy attempt at closed reduction. As mentioned previously, some reports have demonstrated high failure rates with closed reduction, thus necessitating open decompression and fixation. The advocacy of open reduction suffers from a paucity of published clinical outcomes. In 2005, Payer presented a case series of 5 patients, all treated with immediate open reduction using an anteroposterior fixation and fusion with external traction.21 In this series, all patients had achieved fusion at the 3-month follow-up. Ordonez et al. showed similar results in four patients using a ventral approach in 2000.22 The choice to utilize an anterior approach versus a combined anteroposterior fixation was evaluated by Kim et al., who concluded that the ventral approach was sufficient for long-term stabilization.23 The choice of approach during open reduction has been outlined by Nassr et al., and is predicated on two factors: the success of closed reduction and the presence of disc herniation. In those patients who underwent successful reduction and showed signs of herniation, anterior cervical discectomy and fusion followed by posterior fusion is recommended. Patients who underwent successful reduction and had no radiographic evidence of herniation may undergo posterior fusion with instrumentation. Those patients who were treated unsuccessfully with closed reduction and show evidence of herniation may undergo anterior reduction and fusion followed by posterior fusion.24
The evidence in favor of open reduction relies on several case series, all of which show excellent outcomes. Certain factors, including the time from presentation to the operating room and surgeon experience and comfort may influence the outcomes of open reduction, based on the resources of the center or region. The influence of cost and the patient’s clinical stability also may be taken into account. The availability of an operative suite and time to surgery should be strongly considered. In a series of 37 patients with bilaterally locked facets, Hadley et al. showed a correlation between long-term outcomes and time to treatment, regardless of whether open or closed reduction was employed. Thus, the choice to employ either open or closed reduction must be made with particular regard to the temporal availability of either modality.25
Case Illustration
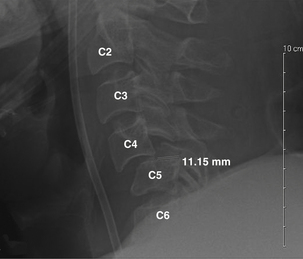
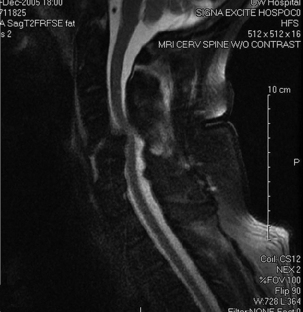
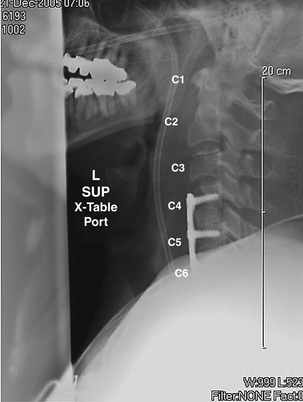
A 59-year-old man presented after being involved in a rollover motor vehicle accident. On examination, he had grade 4/5 strength in his lower extremities and 3/5 strength in his upper extremities. Right deltoid strength was 0/5 and left deltoid 2/5. Rectal examination showed intact tone. Cervical radiographs revealed bilaterally jumped facets at C4-5 (Fig. 215-1). Due to alcohol intoxication, the patient underwent immediate MRI in the trauma bay. No disc herniation was present (Fig. 215-2). He was taken immediately to the operating room from the emergency department for a ventral decompression and fixation. Following anterior cervical discectomy at C4-5 and complete decompression of the spinal cord, cranial traction was applied as well as direct manipulation of the C4 vertebral body. Reduction was accomplished, traction reduced, and bone grafting performed. Fractures were noted at C5-6, and this level also was included in the arthrodesis. Plate fixation was applied from C4 to C6 (Fig. 215-3). Physical examination performed immediately postoperatively revealed rapid improvement in motor strength, to 5/5 in the lower extremities, 4/5 in the upper extremities, 2/5 in the right deltoid, and 4/5 in the left deltoid. This case illustrates the variability that may be present in the patient presenting with bilaterally locked facets. Here, the decision to obtain an MRI examination was simplified by the patient’s intoxication, which did not allow for a reliable assessment of his neurologic status. The MRI did not show herniation as it does in most of these cases; thus, the decision to employ closed reduction would have been safe, as to avoid delay in reduction, the patient was taken immediately to the operating room. In this situation, a ventral strategy alone was employed, and was sufficient and allowed for rapid reduction and stabilization of the dislocation.
Fehlings M.G., Perrin R.G. The role and timing of early decompression for cervical spinal cord injury: update with a review of recent clinical evidence. Injury. 2005;36(Suppl 2):B13-B26.
Hadley M.N. Initial closed reduction of cervical spine fracture-dislocation injuries. Neurosurgery. 2002;50:S44-S50.
Panjabi M.M., Simpson A.K., Ivancic P.C., et al. Cervical facet joint kinematics during bilateral facet dislocation. Eur Spine J. 2007;16:1680-1688.
Resnick D.K., Choudhri T.F., Dailey A.T., et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. part 1: introduction and methodology. J Neurosurg Spine. 2005;2:637-638.
Sonntag V.K. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1981;8:150-152.
1. Allen B.L.Jr., Ferguson R.L., Lehmann T.R., O’Brien R.P. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7:1-27.
2. Bauze R.J., Ardran G.M. Experimental production of forward dislocation in the human cervical spine. J Bone Joint Surg [Br]. 1978;60:239-245.
3. Panjabi M.M., Simpson A.K., Ivancic P.C., et al. Cervical facet joint kinematics during bilateral facet dislocation. Eur Spine J. 2007;16:1680-1688.
4. Payer M., Schmidt M.H. Management of traumatic bilateral locked facets of the subaxial cervical spine. Contemp Neurosurg. 2005;27:1-3.
5. Sen C.N., Sekhar L.N. An extreme lateral approach to intradural lesions of the cervical spine and foramen magnum. Neurosurgery. 1990;27:197-204.
6. Rizzolo S.J., Piazza M.R., Cotler J.M., et al. Intervertebral disc injury complicating cervical spine trauma. Spine (Phila Pa 1976). 1991;16:S187-S189.
7. Fehlings M.G., Perrin R.G. The role and timing of early decompression for cervical spinal cord injury: Update with a review of recent clinical evidence. Injury. 2005;36(Suppl 2):B13-B26.
8. Hadley M.N., Walters B.C., Grabb P.A., et al. Guidelines for the management of acute cervical spine and spinal cord injuries. Clin Neurosurg. 2002;49:407-498.
9. Cotler J.M., Herbison G.J., Nasuti J.F., et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine (Phila Pa 1976). 1993;18:386-390.
10. O’Brien P.J., Schweigel J.F., Thompson W.J. Dislocations of the lower cervical spine. J Trauma. 1982;22:710-714.
11. Sonntag V.K. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1981;8:150-152.
12. Yu Z.S., Yue J.J., Wei F., et al. Treatment of cervical dislocation with locked facets. Chin Med J (Engl). 2007;120:216-218.
13. Grant G.A., Mirza S.K., Chapman J.R., et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg. 1990;90:13-18.
14. Doran S.E., Papadopoulos S.M., Ducker T.B., Lillehei K.O. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79:341-345.
15. Hart R.A. Cervical facet dislocation: when is magnetic resonance imaging indicated? Spine (Phila Pa 1976). 2002;27:116-117.
16. Vaccaro A.R., Falatyn S.P., Flanders A.E., et al. Magnetic resonance evaluation of the intervertebral disc, spinal ligaments, and spinal cord before and after closed traction reduction of cervical spine dislocations. Spine (Phila Pa 1976). 1999;24:1210-1217.
17. Hadley M.N. Initial closed reduction of cervical spine fracture-dislocation injuries. Neurosurgery. 2002;50:S44-S450.
18. Grauer J.N., Vaccaro A.R., Lee J.Y., et al. The timing and influence of MRI on the management of patients with cervical facet dislocations remains highly variable: a survey of members of the Spine Trauma Study Group. J Spinal Disord Tech. 2009;22:96-99.
19. Sears W., Fazl M. Prediction of stability of cervical spine fracture managed in the halo vest and indications for surgical intervention. J Neurosurg. 1990;72:426-432.
20. Vaccaro A.R., Nachwalter R.S. Is magnetic resonance imaging indicated before reduction of a unilateral cervical facet dislocation? Spine (Phila Pa 1976). 2002;27:117-118.
21. Payer M. Immediate open anterior reduction and antero-posterior fixation/fusion for bilateral cervical locked facets. Acta Neurochir (Wien). 2005;147:509-513. discussion 513–514
22. Ordonez B.J., Benzel E.C., Naderi S., Weller S.J. Cervical facet dislocation: Techniques for ventral reduction and stabilization. J Neurosurg. 2000;92:18-23.
23. Kim K.H., Cho D.C., Sung J.K. The management of bilateral interfacetal dislocation with anterior fixation in cervical spine: comparison with combined antero-posterior fixation. J Korean Neurosurg Soc. 2007;42:305-310.
24. Nassr A., Lee J.Y., Dvorak M.F., et al. Variations in surgical treatment of cervical facet dislocations. Spine (Phila Pa 1976). 2008;33:E188-E193.
25. Hadley M.N., Fitzpatrick B.C., Sonntag V.K., Browner C.M. Facet fracture-dislocation injuries of the cervical spine. Neurosurgery. 1992;30:661-666.
Closed Reduction
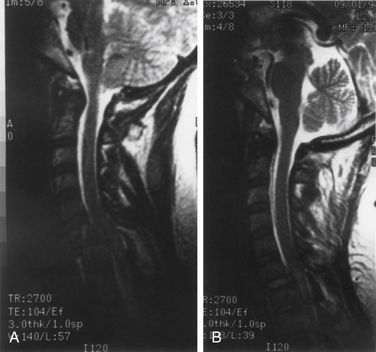
The patient with cervical trauma that results in C6-7 dislocation, with locked facets and an incomplete motor and sensory neurologic deficit, is presented in Figure 215-4. By virtue of its ventral subluxation, angular deformity, bilateral facet dislocation, and neurologic deficit, such a spinal injury is considered unstable.1,2 These fractures of the lower cervical spine have been analyzed extensively, both clinically and in the laboratory, using cadaveric spines. The mechanism of injury is considered to be flexion distraction with resultant partial or total disruption of the interspinous ligament, bilateral capsular ligaments, posterior longitudinal ligament, and anulus and disc.1,3 Biomechanical studies on human cadaveric spines have further confirmed that for a facet dislocation to occur, the ligaments above that facet must be injured or severed. Owing to this mechanism with primarily ligamentous injury and minor bony fractures, if any, the treatment of facet dislocations has been controversial. Whereas some experts have resorted to nonoperative treatment and halo immobilization,4–7 others have chosen operative intervention without necessarily expending time and effort with preoperative reduction.8–11
The argument in favor of surgery has been that ligamentous injury often heals poorly in spite of reduction and prolonged immobilization. Indeed, failure rates of up to 20% have been reported with halo immobilization.4– 6 These results have swayed some to prefer early operative intervention to expedite rehabilitation. This enthusiasm for surgery must be tempered by the morbidity and mortality of surgical intervention, which has been estimated at up to 10%.9,12 In addition to the morbidity of operative intervention, one should also consider the exorbitant cost of the implants, and the fact that some of these patients are still immobilized in a cervical orthosis postoperatively.
The patient shown in Figure 215-4 presented with a radiculopathy and incomplete spinal cord injury secondary to a fracture-dislocation at C6-7 with perched facets. Before the application of traction, an MRI was obtained to assess the spinal cord and to rule out the presence of surgical pathology, such as a herniated disc or epidural hematoma. Several authors have emphasized that disc herniation may be detrimental if closed reduction is attempted.13–16 Generally, as in the case illustrated, the posttraumatic neurologic deficit arises from acute and dynamic spinal cord injury and acute compression rather than disc herniation or a blood clot. The patient was treated with skeletal traction (see Fig. 215-4B). The dislocation was reduced, and the patient showed some, but not total, neurologic recovery. Traction with fracture reduction and relief of spinal cord compression, followed by halo immobilization, can be the sole treatment necessary. Traction can be the only treatment used in patients with associated multiple injuries, such as pulmonary and cardiac contusions, visceral lacerations, long bone fractures, and, occasionally, head injury. These patients often require prolonged ventilatory support and traction and immobilization for their extremity fractures.
Once reduction is achieved and the patient’s condition improves, gradual mobilization in a halo with sequential radiographs commences. A postreduction MRI is indicated to confirm the adequacy of the decompression achieved by traction. This regimen of treatment is successful in up to 90% of cases.6 In fact, the neurologic deficit of those treated nonoperatively has been similar to that of those treated with open reduction and internal fixation. Should the patient experience failure of the halo device, and experience redislocation or develop unacceptable angulation, surgical intervention may then be undertaken. Such failure is not inconsequential, and the rate can be as high as 20%.4,5 Operative intervention with open reduction and internal fixation can then be undertaken.1,3,4,8,12 Traction is time proven and controlled, with the patient generally awake and interactive. When traction fails to reduce a dislocation, or the patient redislocates in a halo, surgery can be undertaken at that time.
Bohlman H.H. Acute fractures and dislocations of the cervical spine: an analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg [Am]. 1979;61:1119-1142.
Lind B., Sihlbom H., Nordwall A. Halo-vest treatment of unstable traumatic cervical spine injuries. Spine (Phila Pa 1976). 1988;13:425-432.
Maiman D.J., Barolat G., Larson S.J. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1986;18:542-547.
Tator C.H., Duncan E.G., Edmonds V.E., et al. Comparison of surgical and conservative management in 208 patients with acute spinal cord injury. Can J Neurol Sci. 1987;14:60-69.
White A.A., Panjabi M.M. The problem of clinical instability in the human spine: a systematic approach. In White A.A., Panjabi M.M., editors: Clinical biomechanics of the spine, ed 2, Philadelphia: Lippincott-Raven, 1990.
Woodsworth R., Molinari W.J., Brandenstein D., et al. Anterior cervical discectomy and fusion with structural allograft and plates for the treatment of unstable posterior cervical spine injuries. J Neurosurg Spine. 2009;10:93-101.
1. Allen B.L., Ferguson R.L., Lehmann T.R., O’Brien R.P. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine (Phila Pa 1976). 1982;7:1-27.
2. White A.A., Panjabi M.M. The problem of clinical instability in the human spine: a systematic approach. In White A.A., Panjabi M.M., editors: Clinical biomechanics of the spine, ed 2, Philadelphia: Lippincott-Raven, 1990.
3. Maiman D.J., Barolat G., Larson S.J. Management of bilateral locked facets of the cervical spine. Neurosurgery. 1986;18:542-547.
4. Bucholz R.D., Cheung K.C. Halo vest versus spinal fusion for cervical injury: evidence from an outcome study. J Neurosurg. 1989;70:884-892.
5. Fisher C., Dvorak M., Leith J., Wing P. Comparison of outcomes for unstable lower cervical flexion teardrop fractures managed with halo thoracic vest versus anterior corpectomy and plating. Spine (Phila Pa 1976). 2002;27(2):160-166.
6. Lind B., Sihlbom H., Nordwall A. Halo-vest treatment of unstable traumatic cervical spine injuries. Spine (Phila Pa 1976). 1988;13:425-432.
7. Tator C.H., Duncan E.G., Edmonds V.E., et al. Comparison of surgical and conservative management in 208 patients with acute spinal cord injury. Can J Neurol Sci. 1987;14:60-69.
8. Bohlman H.H. Acute fractures and dislocations of the cervical spine: an analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg [Am]. 1979;61:1119-1142.
9. Brodke D., Anderson P., Newell D., et al. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech. 2003;6(3):229-235.
10. Kotani Y., Abumi K., Ito M., Minami A. Cervical spine injuries associated with lateral mass and facet joint fractures: new classification and surgical treatment with pedicle screw fixation. Eur Spine J. 2005;14:69-77.
11. Woodsworth R., Molinari W.J., Brandenstein D., et al. Anterior cervical discectomy and fusion with structural allograft and plates for the treatment of unstable posterior cervical spine injuries. J Neurosurg Spine. 2009;10:93-101.
12. Hadley M.N., Fitzpatrick B.C., Sonntag V.K., Browner C.M. Facet fracture-dislocation injuries of the cervical spine. Neurosurgery. 1992;30(5):661-666.
13. Berrington N.R., van Staden J.F., Willers J.G., van der Westhuizen J. Cervical intervertebral disc prolapse associated with traumatic facet dislocations. Surg Neurol. 1993;40(5):395-399.
14. Doran S.E., Papadopoulos S.M., Ducker T.B., Lillehei K.O. Magnetic resonance imaging documentation of coexistent traumatic locked facets of the cervical spine and disc herniation. J Neurosurg. 1993;79(3):341-345.
15. Eismont F.J., Arena M.J., Green B.A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg [Am]. 1991;73(10):1555-1560.
16. Robertson P.A., Ryan M.D. Neurological deterioration after reduction of cervical subluxation. Mechanical compression by disc tissue. J Bone Joint Surg [Br]. 1992;74(2):224-227.