1 Basic Airway Management
• Establishment of a patent airway is the cornerstone of successful resuscitation and a defining proficiency of emergency medicine.
• Basic airway management includes the initial airway evaluation and identification and use of interventions to maintain oxygenation and ventilation. These interventions might be simple, such as the application of supplemental oxygen, or complex, such as noninvasive ventilation or emergency tracheal intubation.
• The goal of emergency intubation is safe, successful intubation of the trachea with an endotracheal tube that allows oxygenation and ventilation while protecting the airway from aspiration.
• Patients in the emergency department are always considered high risk because they have not been evaluated beforehand, may have eaten recently, may have anatomic obstacles that are not readily apparent, or may have unstable hemodynamic parameters.
Rapid-sequence intubation (RSI) is the technique of combining sedation and paralysis to create optimal intubating conditions to facilitate emergency intubation. RSI has become the standard in emergency airway management, with intubation success rates greater than 99%.1 The emergency airway operator should fully understand the risks and benefits and also know when to deviate from its standard algorithm.
Airway Assessment
Anatomically, one should assess the patient by looking for facial distortion and the position in which the airway is held. Drooling or inability to tolerate secretions may be apparent and are ominous signs that suggests significant supraglottic irritation. Patients should be asked to open their mouth, or if they are obtunded, a jaw-thrust and mouth-opening maneuver should be performed carefully to determine how far it can be opened. Palpation of facial structures includes determination of nasal, maxillary, and mandibular stability. Maxillary instability, in particular, should alert the practitioner to be cautious with any nasal intubation, whether by nasal trumpet, nasogastric tube, or blind nasotracheal intubation, because intracranial misplacement of nasal trumpets and nasogastric and nasotracheal tubes has been reported.2–6 Once past the facial structures, the tongue should be viewed. Similarly, the hard and soft palate, as well as the tonsils, should be evaluated.
Functional assessment is performed to determine whether the patient can move air and phonate. Specific airway noises should be noted, especially stridor.7 Such assessment leads the clinician to evaluate for specific indications for intubation (Box 1.1).8,9
Oxygenation failure can be defined as an inability to maintain oxygen saturation greater than 90% despite optimal oxygen supplementation (the exception is a patient with chronic obstructive pulmonary failure, who typically maintains a saturation of 85% to 90%).8,10 Ventilatory failure is usually measured by clinical features, including respiratory rate, abnormal depth or work of breathing, abnormal breathing patterns, accessory muscle use, inability to speak in complete sentences, presence of abnormal airway sounds (stridor or severe wheezing), or altered mental status. Studies also point to end-tidal carbon dioxide measurement as an aid in procedural sedation,10 but it is potentially unable to accurately predict PaCO2 in patients with dyspnea.11
Acute obtundation diminishes a patient’s ability to sense irritant stimuli and therefore spontaneously protect the airway.9,12 This is part of the rationale for using a Glasgow Coma Scale score of 8 or lower as a cue to intubate trauma patients.12 Traditionally, the gag reflex has been used to determine whether a patient’s airway reflexes are intact. Stimulation of a gag reflex in an obtunded or trauma patient may result in unwanted patient reactions, however, such as bucking, gagging, coughing, or actual vomiting; additionally, up to 37% of healthy volunteers fail to demonstrate a gag reflex.12,13 Alternatively, a patient who swallows spontaneously while recumbent has sensory and motor paths capable of protecting the airway.12,14,15 In addition, recent articles have questioned use of the Glasgow Coma Scale score in nontrauma patients and instead emphasize clinical judgment in making the decision to intubate.16,17
Critical Airway Physiology
Oxygenation Techniques
The binding of oxygen to hemoglobin is not linear. Hemoglobin tends to bind oxygen well until the partial pressure of oxygen decreases to 60 mm Hg, and then it rapidly dissociates to allow diffusion of oxygen into blood and surrounding tissue. An oxygen partial pressure of 60 mm Hg correlates with an oxygen saturation of approximately 90%18 (Fig. 1.1). This is an important correlation that should be kept in mind throughout resuscitation (Table 1.1).
| DEVICE | RATE | FIO2 (%) |
|---|---|---|
| Nasal cannula | 2 L | 24 |
| Nasal cannula | 4 L | 27 |
| Nasal cannula | 6 L | 30 |
| Venturi mask | — | 40 |
| Nonrebreather mask | 15 L + | 65-70 |
| Bag-mask (one-way inhalation valve + one-way exhalation port, seal maintained without bagging) | 15 L + | 90 |
From Barker TD, Schneider RE. Supplemental oxygenation and bag-mask ventilation. In: Walls RM, Murphy MF, editors. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. pp. 47-61. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html; http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html.
Patients who require intubation should be preoxygenated with a nonrebreather mask. The goal is to wash as much nitrogen out of the lungs as possible and replace it with oxygen.19–21
When the patient is paralyzed during RSI, this reservoir will permit continued delivery of oxygen to the alveoli for some time, thereby allowing the patient to maintain oxygen saturation while apneic. Five or more minutes of preoxygenation allows this reservoir to develop. Alternatively, if pressed for time, the patient can be asked to take eight vital capacity breaths through the nonrebreather in an attempt to build as great a reservoir as possible.22 Not surprisingly, critically ill patients have decreased oxygen reserve and tolerate apnea less well than do relatively healthy subjects.19,20,23,24
Positive pressure will occasionally be required to oxygenate a patient before intubation. A critical feature of RSI is avoidance of active bag-mask ventilation unless it is absolutely necessary.22 Active bag-mask ventilation with oxygenation is reserved for patients whose oxygen saturation is below 90%.8 Any positive pressure ventilation will not only ventilate the lungs but also insufflate the stomach. This fact is critical to the performance of RSI because a paralyzed patient is at risk for aspiration as a result of relaxed esophageal sphincter tone, especially if the stomach is distended with air.22 Active bag ventilation and oxygenation may need to be performed in patients who are experiencing acute oxygenation failure. Most adult bag-mask devices have reservoirs greater than 1 L and can deliver high-flow oxygen if a good mask seal is maintained.24–26 Alternatively, continuous positive airway pressure or bilevel positive airway pressure can provide a constant level of positive pressure support or two levels of pressure support, respectively, through a tightly fitted mask that fits over the nose or the mouth and nose27,28; if applied in a timely manner in the correct patient, the need for intubation might be averted.
Bag-Mask Technique
Bag-mask oxygenation plus ventilation is a critical skill that all airway managers must master before learning to perform RSI (Boxes 1.2 and 1.3).19 Application of the bag and mask requires proper patient positioning and correct application of a mask seal. The ideal position for mask ventilation is with the patient supine and the head and neck in the sniffing position.19 A proper mask seal is obtained by opposing the mask to the facial skin to create a good air seal. Additionally, new extraglottic devices are available that allow bag ventilation with an inflated balloon surrounding the glottis.29 These devices can also be used to ventilate and oxygenate patients who do not have contraindications (Box 1.4).7,30–37
Box 1.2 Failed Airway Fallback
Mask ventilation is the initial airway management modality of choice for any patient who fails to maintain adequate oxygenation with a nonrebreather mask or begins to desaturate below 90% while apneic during an attempt at rapid-sequence intubation.8
Box 1.4
Causes of Airway Difficulty
Problems with bag ventilation: MOANS (Mask seal, Obesity, Age [>50 years old], Neck mobility, Snores)7,30
Problems with laryngoscopy: LEMON (Look for airway distortion, Evaluate mouth opening and thyromental distance, Mallampati score, Obstruction, Neck mobility)31–37
Problems with cricothyrotomy: SHORT (previous neck Surgery, expanding neck Hematomas, Obesity, previous Radiation therapy, and Tumors and abscesses that might distort the anatomy)7
Problems with the use of extraglottic devices: RODS (Restricted mouth opening, Obstruction, Disrupted or distorted airway, Stiff lungs or cervical spine)36
From Murphy MF, Walls RM. Identification of the difficult and failed airway. In: Walls RW, Murphy WF, editors. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott, Williams & Wilkins; 2008. pp. 81-93. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html; http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html.
Emergency Airway Algorithm
A patient who merits intubation and is dead or nearly so (a crash airway) requires immediate orotracheal intubation or cricothyrotomy without sedation or paralysis. A patient who is alive and requires intubation will force the airway manager to determine the method of intubation and what medications to use to facilitate it (Fig. 1.2).8
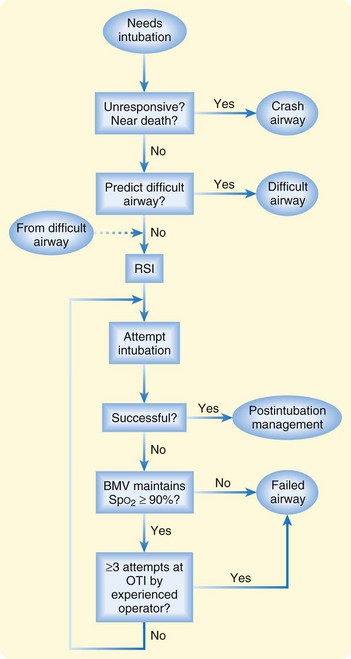
Fig. 1.2 Main emergency airway management algorithm.
(Adapted from Walls RM: The emergency airway algorithms. In Walls RM, Luten RC, Murphy MF, et al, editors. Manual of emergency airway management. 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2004. Copyright 2004: The Airway Course and Lippincott Williams & Wilkins.)
If the patient is not a crash airway candidate, one should plan to use medications to facilitate intubation. This step requires a determination of expected airway difficulty. Failure to evaluate and anticipate airway difficulty is one of the major causes of failure of intubation.38,39 The use of paralytics in emergency intubation requires preparation for an alternative airway in the event that a patient cannot be intubated by standard means. A difficult airway may preclude the use of paralytics altogether until the clinician can ensure glottic visualization, which is usually obtained with procedural sedation and topical anesthesia. The approach to a difficult airway is discussed in greater detail in Chapter 2.
Unfortunately, there is no universal definition of a difficult airway. Some patients give the clinician an immediate gestalt that their airway will be difficult. Clinicians tend to be correct when their initial reaction is that an airway will be difficult.38,39 The converse is not true. Some otherwise normal-appearing patients will have subtle anatomic differences that may make intubation difficult and are not immediately recognizable by a clinician who is not specifically evaluating for such difficulty.
A number of studies have demonstrated various clinical cues that can be used in an attempt to predict a difficult airway (see Box 1.4). No clinical sign, either alone or in combination with other signs, is 100% sensitive in ruling out a difficult airway.31–35,38,40 However, by using a combination of signs, the vast majority can be identified to make the practitioner aware of potential hazards.
Identification of airway difficulty will require the clinician to give serious thought to performing a sedated examination of the airway with topical anesthesia before proceeding to RSI with neuromuscular blockade (see Chapter 2.)
Intubation
Orotracheal intubation is now the preferred method of emergency intubation, either by direct laryngoscopy or by video laryngoscopy.44–46 The process of intubation includes proper patient positioning, clinician positioning, tool choice and assembly, and technique of laryngoscopy. In performing standard oral intubation, the patient lies flat and supine while positioning of the patient’s head is addressed.44 Patients with immobile cervical spines, whether secondary to trauma, arthritis, or other causes, should not have their heads or necks manipulated, and the head should be maintained in a neutral position with in-line stabilization by a person designated for this task.45,46 If mobility is not an issue, the age of the patient and size of the occiput determine the need for elevation of the patient’s shoulders or head. Infants have a relatively large occiput with respect to their bodies and will therefore passively flex their head forward when lying flat.47 This makes a more acute angle that the laryngoscopist has to navigate. The airway axes will align better if the infant’s shoulders are elevated. An adult’s head is relatively smaller and tends to extend at the cervicothoracic junction instead of flexing. This counterintuitively moves the laryngeal and pharyngeal axes into an alignment that is less parallel and can be overcome by placing a roll under the adult’s head.47 A key anatomic relationship to keep in mind is that the head is ideally aligned when an imaginary line drawn between the tragus of the ear and the anterior axillary line is parallel to the floor.
Video laryngoscopic intubation is the newest method of orotracheal intubation and has developed into a valid option for primary intubation in the majority of patients. Multiple options exist, and each has its own method of how it is used.48 The benefit of these devices is that they routinely provide a laryngoscopic view superior to that possible with direct laryngoscopy in the vast majority of patients in whom they are used.42,43,49,50 The angles required for passage of the tube may sometimes present the key challenge, so this is an additional focal point of training. As with any video-based system, the principal downside is the potential for obstruction of the operator’s view if blood, vomitus, or excessive secretions are present in the oropharynx.
Finally, nasotracheal intubation is another option for intubation, although its use is decreasing in favor of directly visualized oral intubation. Nasotracheal intubation requires a breathing patient because the patient’s breath sounds will guide the intubator in placing the tube. Nasotracheal intubation should not be considered a primary mode of intubation because its success rate has clearly been shown to be lower than that of orotracheal intubation with RSI.51
Medications, Pharmacology, and Physiologic Responses to Medication Classes
Sedative Agents
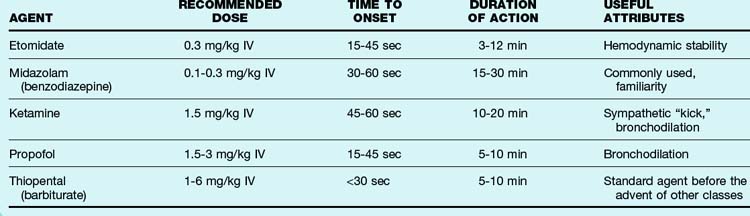
Multiple sedatives can be used for RSI. Use of a sedative humanely allows amnesia and sedation, thereby potentially improving laryngoscopy and intubation.41 The choice of sedative agent for a given clinical scenario differs according to the pathophysiologic parameters that the clinician observes or anticipates to occur during the attempt at RSI. Hemodynamic instability, elevated intracranial pressure, and bronchospasm are some of the most common complicating factors that the clinician must consider during preparation for sedation. A list of sedative agents used for RSI and their side effect profiles can be found in Table 1.2.
The most commonly used sedatives in current emergency practice include midazolam (Versed) and etomidate (Amidate). Doses of midazolam recommended in the anesthesia literature are 0.1 to 0.3 mg/kg intravenously. The danger of using midazolam in these doses is the hypotension that it generates, especially in critically ill patients. Most practitioners will intentionally underdose midazolam in the setting of RSI for this specific reason.52
Etomidate is administered at a dose of 0.3 mg/kg intravenously and does not cause the hypotension seen with midazolam.52–54 Etomidate does cause reversible cortisol suppression, however, and is no longer used as a drip for long-term sedation. The effect on cortisol after a single dose has been demonstrated to resolve spontaneously and has not been shown to have an effect on patient outcome.55 Controversy has recently developed regarding the use of etomidate in patients with sepsis. One major study reportedly identified etomidate as a causal agent in increasing mortality in this patient population.56,57 However, this study was underpowered and not designed to look for this concern, and its findings were based on post hoc analysis of the study results.58 At least one small-scale study has demonstrated no increase in mortality between etomidate and midazolam in this setting.59 No large-scale study exists at the time of this writing to specifically answer this question, but with the overwhelming success of single-dose etomidate in emergency intubations, definitive studies would be necessary to change practice.
Neuromuscular Blocking Agents (Paralytics)
The paralytics commonly used for RSI include depolariz-ing agents (succinylcholine) and nondepolarizing agents (vecuronium, rocuronium). Succinylcholine has been studied extensively and is the classic agent used for RSI. It has a short time of onset (approximately 45 seconds), a short duration of action (approximately 5 to 10 minutes), and a wide dosing margin (the typical dose for RSI is 1.5 mg/kg, but doses up to 6 mg/kg do not change its pharmacokinetics).60 Succinylcholine also has some significant side effects, including occasionally significant hyperkalemia, fasciculations, and malignant hyperthermia. Any airway manager who plans to use succinylcholine should be well versed in its mechanism of action, as well as its potentially significant and life-threatening side effects61,62 (Box 1.5).
Box 1.5 Succinylcholine—Critical Points
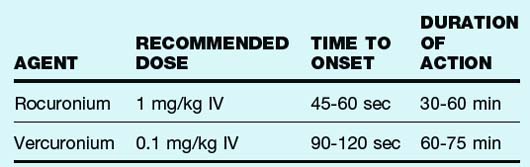
Rocuronium has recently come into favor as a nondepolarizing agent that can provide succinylcholine-like intubating conditions in 45 to 60 seconds, provided that the correct dose (1.0 to 1.2 mg/kg intravenously) is used.63–66 The benefits of using a nondepolarizing agent include the absence of fasciculations and hyperkalemia. The duration of action of nondepolarizing agents is much longer than that of succinylcholine, however, with rocuronium being the shortest acting at 45 to 60 minutes. See Table 1.3 for a list of commonly used nondepolarizing paralytic agents.
Pretreatment Agents
Some medications have the potential to aid in promoting physiologic responses to intubation if given as pretreatment agents. The typical laryngoscopy in an adult will result in sympathetic stimulation that could be detrimental in certain cases. Patients with asthma, elevated intracranial pressure, aortic dissection, hypertensive emergencies, and acute myocardial infarction have pathophysiology that could be worsened by an increase in sympathetic stimulation.67 Intravenous lidocaine, 1.5 mg/kg, has potential benefit in attenuating bronchospasm68,69 and increases in intracranial pressure70,71 when given as a premedication 2 to 3 minutes before RSI. Opioids (e.g., fentanyl, 1 to 5 mcg/kg intravenously 2 to 3 minutes before RSI) may have benefit in attenuating increases in intracranial pressure72 and reflexive, sympathetic hemodynamic responses to intubation.73,74 A body of literature indirectly supports the select use of these medications in critical airway management (Table 1.4). Laryngoscopy or the succinylcholine dosage in pediatric patients can result in parasympathetic stimulation and resultant bradycardia, which has led some experts to advocate a pretreatment dose of atropine before attempts at pediatric intubation. Current recommendations are to use atropine for all intubations in children younger than 1 year and to have the drug available for those older than 1 year.47
| Agent | Recommended Dose | Proposed Action |
|---|---|---|
| Lidocaine | 1.5 mg/kg IV | Blunt bronchospasm, blunt the reflexive response to laryngoscopy |
| Opioid (fentanyl) | 1.5 mcg/kg IV | Blunt the reflexive response to laryngoscopy |
| Atropine | 0.01 mg/kg IV | Avoid bradycardia in children receiving succinylcholine |
Putting It Together: Rapid-Sequence Intubation
RSI is the technique of combining sedation and paralysis to create the most optimal intubating conditions during emergency intubation (Box 1.6).1,9,22,41,75 Seven checklist points have been identified to help clinicians prepare for emergency RSI (Box 1.7).22 Also known as the 7 P’s, this or a similar checklist can be used during each intubation in which airway managers participate.22 This tool should be viewed as a patient safety device and an error minimization instrument. As with any high-stakes activity, the use of memory aids and algorithms can reduce the cognitive load associated with decision making and allow the practitioner to focus on the specific task at hand.76
Protection of the airway refers to the use of cricoid ring pressure (Sellick maneuver) during the process of paralysis, intubation, and confirmation of endotracheal placement. The cricoid ring is compressed with an assistant’s index finger and thumb in an attempt to compress the underlying esophagus and prevent passive regurgitation of stomach contents into the trachea.77,78 The amount of force recommended is equivalent to the amount required to create discomfort when pressing with the same fingers on the bridge of the nose.19 Some studies have identified improper Sellick maneuver technique as a potential obstruction to laryngoscopy and placement of the endotracheal tube (ETT), but it might help prevent gastric insufflation during attempts at bag-mask ventilation and is currently recommended if resources permit.19
The sixth step is passage of the tube. Laryngoscopy is performed at approximately 1 minute after the paralytic agent has been administered. The ETT is placed under direct vision (either line of sight or with video monitoring) through the cords and into the trachea. An adult man should typically have the tube placed orally to a depth of 24 cm, and an adult woman should typically have the tube inserted to 21 cm. A general rule of thumb is that the ETT should be inserted to three times its size.79 Placement of the ETT is considered complete once objective verification of placement has occurred, typically by end-tidal carbon dioxide detection.80,81
Summary
Emergency airway management involves a combination of techniques and strategies designed to ensure success of intubation in critically ill patients. The approach to an emergency airway is necessarily different from that taken for an elective or urgent case. The airway manager must have a solid foundation in ventilation techniques (bag-mask, extraglottic devices), which will be the first rescue device. Assessment of the airway is a critical skill that mandates a methodic approach to ensure that a difficult airway is recognized and appropriately planned for. The use of RSI has revolutionized emergency intubation, and a set of strategies is required to deal with routine intubations and difficult airways. Management of difficult airways is discussed in Chapter 2.
1 Sagarin MJ, Barton ED, Chng YM, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46:328–336.
2 Marlow TJ, Goltra DD, Jr., Schabel SI. Intracranial placement of a nasotracheal tube after facial fracture: a rare complication. J Emerg Med. 1997;15:187–191.
3 Martin JE, Mehta R, Aarabi B, et al. Intracranial insertion of a nasopharyngeal airway in a patient with craniofacial trauma. Mil Med. 2004;169:496–497.
4 Moustoukas N, Litwin MS. Intracranial placement of nasogastric tube: an unusual complication. South Med J. 1983;76:816–817.
5 Schade K, Borzotta A, Michaels A. Intracranial malposition of nasopharyngeal airway. J Trauma. 2000;49:967–968.
6 Arslantas A, Durmaz R, Cosan E, et al. Inadvertent insertion of a nasogastric tube in a patient with head trauma. Childs Nerv Syst. 2001;17:112–114.
7 Murphy MF, Walls RM. Identification of the difficult and failed airway. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:81–93. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
8 Walls RM. The emergency airway algorithms. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:8–24. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
9 Walls RM. The decision to intubate. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:1–7. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
10 Deitch K, Miner J, Chudnofsky CR, et al. Does end tidal CO2 monitoring during emergency department procedural sedation and analgesia with propofol decrease the incidence of hypoxic events? A randomized, controlled trial. Ann Emerg Med. 2010;55:258–264.
11 Delerme S, Freund Y, Renault R, et al. Concordance between capnography and capnia in adults admitted for acute dyspnea in an ED. Am J Emerg Med. 2010;28:711–714.
12 Mackway-Jones K, Moulton C. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Gag reflex and intubation. J Accid Emerg Med. 1999;16:444–445.
13 Davies AE, Kidd D, Stone SP, et al. Pharyngeal sensation and gag reflex in healthy subjects. Lancet. 1995;345:487–488.
14 Nishino T. Physiological and pathophysiological implications of upper airway reflexes in humans. Jpn J Physiol. 2000;50:3–14.
15 Page M, Jeffery HE. Airway protection in sleeping infants in response to pharyngeal fluid stimulation in the supine position. Pediatr Res. 1998;44:691–698.
16 Eizadi-Mood N, Saghaei M, Alfred S, et al. Comparative evaluation of Glasgow Coma Score and gag reflex in predicting aspiration pneumonitis in acute poisoning. J Crit Care. 2009;24(470):e9–e470. 15
17 Duncan R, Thakore S. Decreased Glasgow Coma Scale score does not mandate endotracheal intubation in the emergency department. J Emerg Med. 2009;37:451–455.
18 Miller RD. Transfusion therapy. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s anesthesia [electronic resource]: expert consult—online and print. 7th ed. Philadelphia: Churchill Livingstone; 2009:1739–1766.
19 Barker TD, Schneider RE. Supplemental oxygenation and bag-mask ventilation. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:47–61. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
20 Benumof JL, Dagg R, Benumof R. Critical hemoglobin desaturation will occur before return to an unparalyzed state following 1 mg/kg intravenous succinylcholine. Anesthesiology. 1997;87:979–982.
21 Henderson J. Airway management in the adult. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s anesthesia [electronic resource]: expert consult—online and print. 7th ed. Philadelphia: Churchill Livingstone; 2009:1573–1610.
22 Walls RM. Rapid sequence intubation. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:25–35. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
23 Chiron B, Laffon M, Ferrandiere M, et al. Standard preoxygenation technique versus two rapid techniques in pregnant patients. Int J Obstet Anesth. 2004;13:11–14.
24 Davidovic L, LaCovey D, Pitetti RD. Comparison of 1- versus 2-person bag-valve-mask techniques for manikin ventilation of infants and children. Ann Emerg Med. 2005;46:37–42.
25 Mort TC. Preoxygenation in critically ill patients requiring emergency tracheal intubation. Crit Care Med. 2005;33:2672–2675.
26 Dorges V, Ocker H, Hagelberg S, et al. Smaller tidal volumes with room-air are not sufficient to ensure adequate oxygenation during bag-valve-mask ventilation. Resuscitation. 2000;44:37–41.
27 Hore CT. Non-invasive positive pressure ventilation in patients with acute respiratory failure. Emerg Med (Fremantle). 2002;14:281–295.
28 Hess D, Chatmongkolchart S. Techniques to avoid intubation: noninvasive positive pressure ventilation and heliox therapy. Int Anesthesiol Clin. 2000;38:161–187.
29 Murphy MF. Extraglottic devices. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:112–138. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
30 Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
31 Juvin P, Lavaut E, Dupont H, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003;97:595–600.
32 Yildiz TS, Solak M, Toker K. The incidence and risk factors of difficult mask ventilation. J Anesth. 2005;19:7–11.
33 Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005;22:99–102.
34 Krobbuaban B, Diregpoke S, Kumkeaw S, et al. The predictive value of the height ratio and thyromental distance: four predictive tests for difficult laryngoscopy. Anesth Analg. 2005;101:1542–1545.
35 Iohom G, Ronayne M, Cunningham AJ. Prediction of difficult tracheal intubation. Eur J Anaesthesiol. 2003;20:31–36.
36 Murphy MF, Walls RM. Identification of the difficult and failed airway. In: Walls RW, Murphy WF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:81–93. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
37 Merah NA, Wong DT, Foulkes-Crabbe DJ, et al. Modified Mallampati test, thyromental distance and inter-incisor gap are the best predictors of difficult laryngoscopy in West Africans. Can J Anaesth. 2005;52:291–296.
38 Murphy M, Hung O, Launcelott G, et al. Predicting the difficult laryngoscopic intubation: are we on the right track? Can J Anaesth. 2005;52:231–235.
39 Walls RM. Management of the difficult airway in the trauma patient. Emerg Med Clin North Am. 1998;16:45–61.
40 Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann Emerg Med. 2004;44:307–313.
41 Sivilotti ML, Filbin MR, Murray HE, et al. Does the sedative agent facilitate emergency rapid sequence intubation? Acad Emerg Med. 2003;10:612–620.
42 Brown CA, 3rd., Bair AE, Pallin DJ, et al. for the National Emergency Airway Registry (NEAR) Investigators. Improved glottic exposure with the Video Macintosh Laryngoscope in adult emergency department tracheal intubations. Ann Emerg Med. 2010;56:83–88.
43 Lim HC, Goh SH. Utilization of a GlideScope videolaryngoscope for orotracheal intubations in different emergency airway management settings. Eur J Emerg Med. 2009;16:68–73.
44 Cassorla L, Lee J. Patient positioning and anesthesia. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s anesthesia [electronic resource]: expert consult—online and print. 7th ed. Philadelphia: Churchill Livingstone; 2009:1151–1170.
45 Nee PA, Birnbaumer DM. The geriatric patient. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:391–396. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
46 Walls RM. Trauma. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:332–342. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
47 Luten RC, McAllister JD. Approach to the pediatric airway. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:263–281. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
48 Sackles JC, Brown CA, III. Video laryngoscopy. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:167–184. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
49 Cooper RM, Pacey JA, Bishop MJ, et al. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198.
50 Sun DA, Warriner CB, Parsons DG, et al. The GlideScope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–384.
51 Godwin SA. Blind intubation techniques. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:104–111. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
52 Sagarin MJ, Barton ED, Sakles JC, et al. Underdosing of midazolam in emergency endotracheal intubation. Acad Emerg Med. 2003;10:329–338.
53 Fuchs-Buder T, Sparr HJ, Ziegenfuss T. Thiopental or etomidate for rapid sequence induction with rocuronium. Br J Anaesth. 1998;80:504–506.
54 Oglesby AJ. Should etomidate be the induction agent of choice for rapid sequence intubation in the emergency department? Emerg Med J. 2004;21:655–659.
55 Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med. 2001;8:1–7.
56 Lipiner-Friedman D, Sprung CL, Laterre PF, et al. Adrenal function in sepsis: the retrospective Corticus cohort study. Crit Care Med. 2007;35:1012–1018.
57 Cuthbertson BH, Sprung CL, Annane D, et al. The effects of etomidate on adrenal responsiveness and mortality in patients with septic shock. Intensive Care Med. 2009;35:1868–1876.
58 Pallin DJ, Walls RM. The safety of single-dose etomidate. Intensive Care Med. 2010;36:1268. author reply 1269–1270
59 Tekwani KL, Watts HF, Sweis RT, et al. A comparison of the effects of etomidate and midazolam on hospital length of stay in patients with suspected sepsis: a prospective, randomized study. Ann Emerg Med. 2010;56:481–489.
60 Naguib M, Lien CA. Pharmacology of muscle relaxants and their antagonists. In: Miller RD, Eriksson LI, Fleisher LA, et al. Miller’s anesthesia [electronic resource]: expert consult—online and print. 7th ed. Philadelphia: Churchill Livingstone; 2009:859–912.
61 Caro DA, Bush S. Neuromuscular blocking agents. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:248–262. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
62 Sparr HJ. Choice of the muscle relaxant for rapid-sequence induction. Eur J Anaesthesiol Suppl. 2001;23:71–76.
63 Laurin EG, Sakles JC, Panacek EA, et al. A comparison of succinylcholine and rocuronium for rapid-sequence intubation of emergency department patients. Acad Emerg Med. 2000;7:1362–1369.
64 Mallon WK, Keim SM, Shoenberger JM, et al. Rocuronium vs. succinylcholine in the emergency department: a critical appraisal. J Emerg Med. 2009;37:183–188.
65 Perry JJ, Lee JS, Sillberg VA, et al. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2, 2008. CD002788
66 Seupaul RA, Jones JH. Evidence-based emergency medicine. Does succinylcholine maximize intubating conditions better than rocuronium for rapid sequence intubation? Ann Emerg Med. 2011;57:301–302.
67 Caro DA, Bush S. Pretreatment agents. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:221–233. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
68 Groeben H, Peters J. Lidocaine exerts its effect on induced bronchospasm by mitigating reflexes, rather than by attenuation of smooth muscle contraction. Acta Anaesthesiol Scand. 2007;51:359–364.
69 Adamzik M, Groeben H, Farahani R, et al. Intravenous lidocaine after tracheal intubation mitigates bronchoconstriction in patients with asthma. Anesth Analg. 2007;104:168–172.
70 Robinson N, Clancy M. In patients with head injury undergoing rapid sequence intubation, does pretreatment with intravenous lignocaine/lidocaine lead to an improved neurological outcome? A review of the literature. Emerg Med J. 2001;18:453–457.
71 Butler J, Jackson R. Towards evidence based emergency medicine: best BETs from Manchester Royal Infirmary. Lignocaine premedication before rapid sequence induction in head injuries. Emerg Med J. 2002;19:554.
72 Kerr ME, Sereika SM, Orndoff P, et al. Effect of neuromuscular blockers and opiates on the cerebrovascular response to endotracheal suctioning in adults with severe head injuries. Am J Crit Care. 1998;7:205–217.
73 Reynolds SF, Heffner J. Airway management of the critically ill patient: rapid-sequence intubation. Chest. 2005;127:1397–1412.
74 Hussain AM, Sultan ST. Efficacy of fentanyl and esmolol in the prevention of haemodynamic response to laryngoscopy and endotracheal intubation. J Coll Physicians Surg Pak. 2005;15:454–457.
75 Sagarin MJ, Chiang V, Sakles JC, et al. Rapid sequence intubation for pediatric emergency airway management. Pediatr Emerg Care. 2002;18:417–423.
76 Levitan RM. Patient safety in emergency airway management and rapid sequence intubation: metaphorical lessons from skydiving. Ann Emerg Med. 2003;42:81–87.
77 Kalinowski CP, Kirsch JR. Strategies for prophylaxis and treatment for aspiration. Best Pract Res Clin Anaesthesiol. 2004;18:719–737.
78 Turgeon AF, Nicole PC, Trepanier CA, et al. Cricoid pressure does not increase the rate of failed intubation by direct laryngoscopy in adults. Anesthesiology. 2005;102:315–319.
79 Murphy MF. Applied functional anatomy of the airway. In: Walls RM, Murphy MF. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008:36–45. Available at http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0807/2007050100-d.html http://www.loc.gov.lp.hscl.ufl.edu/catdir/enhancements/fy0811/2007050100-t.html
80 Bair AE, Smith D, Lichty L. Intubation confirmation techniques associated with unrecognized non-tracheal intubations by pre-hospital providers. J Emerg Med. 2005;28:403–407.
81 Hogg K, Teece S. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Colourimetric CO(2) detector compared with capnography for confirming ET tube placement. Emerg Med J. 2003;20:265–266.

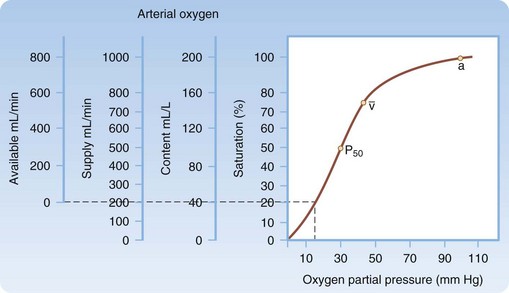
 , normal mixed venous pressure; and P50, the partial pressure (27 mm Hg) at which hemoglobin is 50% saturated.
, normal mixed venous pressure; and P50, the partial pressure (27 mm Hg) at which hemoglobin is 50% saturated.