Balance and vestibular dysfunction
LESLIE K. ALLISON, PT, PhD and KENDA FULLER, PT, NCS
After reading this chapter the student or therapist will be able to:
1. Describe both central and peripheral sensory and motor components of the postural control system.
2. List common postural control impairments found in clients with neurological problems.
3. List commonly used balance tests, and distinguish which are appropriate for clients at low, moderate, and high levels of function.
4. Differentiate how test results are used to identify body system impairments and activity limitations that limit participation.
5. Analyze the interaction of individual, task, and environmental factors that affect balance.
6. Describe how to plan and progress balance exercise programs to increase the use of, or compensation with, available sensory inputs.
7. Describe how to plan and progress balance exercise programs to facilitate anticipatory postural adjustments to prevent balance loss and provoke automatic postural responses to regain balance after unexpected disturbances.
8. Describe how to plan and progress balance exercise programs to increase the control of center of gravity in upright postures and during gait.
9. Describe how to increase the difficulty level of balance exercise programs in order to promote the automaticity of postural control during functional activities.
10. Identify and analyze the function of the vestibular system.
11. Describe how to facilitate adaptation and central nervous system reorganization to regain control of balance and decrease dizziness.
12. Identify patterns of recovery that influence choices of intervention.
Balance Function and Disorders
No matter what the neurological diagnosis, a disease or injury that affects the nervous system is likely to compromise one or more of the postural control mechanisms. For example, clients with such diverse diagnoses as stroke, head trauma, spinal cord injury, peripheral neuropathy, multiple sclerosis (MS), Parkinson disease, cerebellar dysfunction, cerebral palsy, and Guillian-Barré syndrome all experience disequilibrium problems. One common thread among all these different medical diagnoses is the presence of balance impairments. Clients with different medical diagnoses may have the same balance impairments, and clients with the same medical diagnosis may have different balance impairments depending on which portions of the postural control system are involved.1 To optimally understand and manage balance problems, a test of each balance component and the interactive nature of the components is important. The traditional medical “diagnostic” model does not provide this information and is not the most beneficial model for planning balance rehabilitation interventions. The medical diagnosis is relevant: knowing whether deficits are permanent or temporary, and whether recovery or progressive decline is expected, is critical. This medical prognostic information will assist physical and occupational therapists in goal setting and intervention planning.
The International Classification of Functioning, Disability and Health (ICF) model described in Chapter 1 and illustrated in Figure 1-1 describes the interactions of body function and structure problems (impairments) and activity limitations as seen in clients with balance disorders, and how these functional activity limitations restrict an individual’s ability to participate in life situations, thus decreasing quality of life. Balance impairments negatively affect function, often reducing the individual’s ability to participate fully in life.2 These impairments often restrict activity levels, produce abnormal compensatory motor behavior, and may require devices for support or assistance from another person. Falls can result when imbalance is severe, leading to secondary injuries. To avoid these consequences and advance the functional status of clients, therapists should understand both the demands that various environments and functional tasks place on postural control systems and the impairments that may diminish the ability of those systems to respond adequately.
Balance
Definitions of balance
Balance is a complex process involving the reception and integration of sensory inputs and the planning and execution of movement to achieve a goal requiring upright posture. It is the ability to control the center of gravity (COG) over the base of support in a given sensory environment.3,4 The COG is an imaginary point in space, calculated biomechanically from measured forces and moments, where the sum total of all the forces equals zero. In a person standing quietly the COG is located just forward of the spine at approximately the S2 level. With movement of the body and its segments, the location of the COG in space constantly changes. The base of support is the body surface that experiences pressure as a result of body weight and gravity; in standing it is the feet, and in sitting it includes the thighs and buttocks. The size of the base of support will affect the difficulty level of the balancing task. A broad base of support makes the task easier; a narrow base makes it more challenging. The COG can travel farther while still remaining over the base if the base is large. The “shape” of the base of support will alter the distance that the COG can move in certain directions.
Any given base of support places a limit on the distance a body can move without either falling (as the COG exceeds the base of support) or establishing a new base of support by reaching or stepping (to relocate the base of support under the COG). This perimeter is frequently referred to as the limit of stability or stability limit.3,5 It is the farthest distance in any direction a person can lean (away from midline) without altering the original base of support by stepping, reaching, or falling.
Human control of balance
Early studies of postural control mechanisms using selectively lesioned cats and primates focused on reflexive and reactive equilibrium responses that are relatively “hard-wired.”6 These valuable studies brought to light certain stereotypical motor responses to specific sensory stimuli, such as the crossed extension reflex or tonic neck reflexes. There is no doubt that these reflexive and reactive responses—for example, the vestibuloocular reflex (VOR) and the protective extension reactions—are foundational to normal postural control. However, the postural control system encompasses much more than these subcortically driven components. Balance abilities are heavily influenced by higher-level neural circuitry and other systems (e.g., cognitive, musculoskeletal), as well.5 In addition, the nervous system is influenced by and responsive to the demands placed on it by the tasks being accomplished and the environments in which those tasks are performed.7–9 All of these facets are included in a systems approach to dynamic equilibrium.10–12 Examination and intervention methods based on this systems model have consequently evolved.11,13
The systems approach
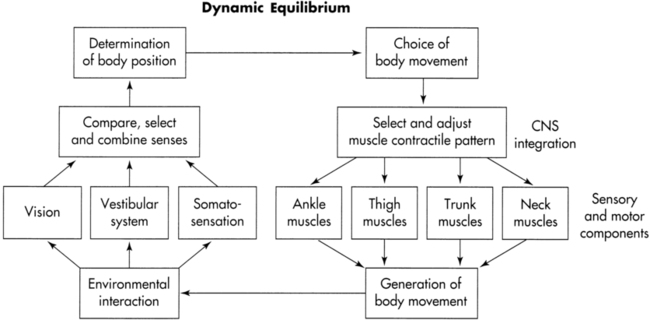
The dynamic systems model for dynamic equilibrium recognizes that balance is a result of interactions among the individual, the task(s) the individual is performing, and the environment in which the task(s) must be performed. These interactions are represented in Figure 22-1. Within the individual, both sensory inputs and processing systems (left side of figure) and motor planning and execution systems (right side of figure) are critical. Both peripheral components (lower part of figure) and central components (upper part of figure) of the systems are involved in the cycle. The cycle is driven both by purposeful choices of the individual (tasks) and by demands placed on the individual by the environment. Successful function of the sensory systems allows recognition of body position and motion in relation to self and the world. The desired outcome from the motor systems is the generation of movement sufficient to maintain balance and perform the chosen, goal-directed task(s).
Peripheral sensory reception
The three primary peripheral sensory inputs contributing to postural control are the bilateral receptors of the somatosensory, visual, and vestibular systems.4,10 Somatosensory receptors located in the joints, ligaments, muscles, and skin provide information about muscle length, stretch, tension, and contraction; pain, temperature, and pressure; and joint position. The feet, ankles, knees, hips, back, neck, and eye muscles all furnish useful information for balance maintenance. Somatosensation is the dominant sense for upright postural control and is responsible for triggering automatic postural responses (APRs). Somatosensory loss significantly impairs balance. Loss of peripheral somatosensation occurs in clients with loss or disease of or injury to the peripheral sensory receptors or afferent sensory nerves. Examples include clients with diabetic neuropathy, peripheral vascular disease, spinal cord injury, and amputation.
Visual receptors in the eyes perform dual tasks. Central (or foveal) vision allows environmental orientation, contributing to the perception of verticality and object motion, as well as identification of the hazards and opportunities presented by the environment.10 For example, a kayaker may see rocks in a stream as a hazard to be avoided, whereas a hiker who wants to cross the stream may see the same rocks as a welcome opportunity. Peripheral (or ambient) vision detects the motion of the self in relation to the environment, including head movements and postural sway. Peripheral vision is largely subconscious, whereas central visual inputs tend to receive more conscious recognition.10 Both are normally used for postural control. Vision is critical for feed-forward, or anticipatory, postural control in changing environments. This includes planning for functional movements such as reaching and grasping, and especially for successful navigation during gait. Vision loss also impairs balance. Loss of peripheral visual inputs occurs in clients with disease of or injury to the eyes or afferent cranial nerves. Examples include clients with cataracts, macular degeneration, glaucoma, or diabetic retinopathy.
The vestibular system provides the central nervous system (CNS) with information about the position and motion of the head. The position of the head in relation to gravity is detected through the otolith system. Horizontal and vertical accelerations, as in riding in a car or an elevator, are also detected by the otoliths.14 Movements of the head are detected through the semicircular canals. Head movement stimulates both sets of semicircular canals, so that the vestibular nerve on one side becomes inhibited while the other becomes excited. The vestibular system provides sensory redundancy in the information obtained from each separate vestibular apparatus. If the peripheral vestibular system is damaged on one side, the information can be captured by the intact canals on the opposite side. The vestibular system is critical for balance because it uniquely identifies self-motion as different from motion in the environment. Box 22-1 describes the sensory components of the vestibular system. Vestibular loss also impairs balance. Loss of peripheral vestibular inputs occurs in clients with disease of or injury to the peripheral sensory receptors or afferent cranial nerves. Examples include clients with head injury involving temporal bone damage, acoustic neuroma, benign positional vertigo (BPV), or Meniere disease. For a comprehensive review of the vestibular system and vestibular disorders, please see the vestibular section of this chapter beginning on page 689.
Central sensory perception
The brain processes all the environmentally available sensory information gathered by the peripheral receptors in varying degrees. This processing is usually referred to as multisensory integration or sensory organization.4,10 Central sensory structures function first to compare available inputs between two sides and among three sensory systems. The somatosensory system alone is unable to distinguish surface tilts from body tilts. Also, the visual system by itself cannot discriminate movement of the environment from movement of the body.14 The vestibular system by itself cannot tell if head movement through space is produced by neck motion or trunk and hip motion. Therefore the brain needs information from all three senses to correctly distinguish self-motion from motion in the environment.
When changes in the environment occur, the relative availability, accuracy, and usefulness of information from the three sensory systems may also change. Sensory organization also includes an adaptive process, called multisensory reweighting, that permits the CNS to prioritize the sources of sensory information when environmental conditions change.15,16 Available, accurate, and useful information is “upweighted,” whereas unavailable, inaccurate, or less-useful information is “downweighted.” For example, in dark environments, vision would be downweighted and somatosensory and vestibular information would be upweighted. This adaptive process is imperfect, however, and balance is not as well controlled when any sense must be downweighted as it is when all three senses are available and accurate. Individuals with peripheral sensory loss or central sensory processing deficits may have difficulty reweighting quickly and fully. This impairs their ability to adapt to, and remain stable in, changing environments.17
Intrinsic central sensory processing impairments also can produce sensory conflict. An adult hemiplegic patient with pusher syndrome illustrates an inability to integrate visual, vestibular, and somatosensory inputs for midline orientation. Within a single system, discrepancies between the sides are also problematic. Unequal firing from opposite sides of the vestibular system, as in unilateral vestibular hypofunction, produces a mismatch that is subsequently interpreted as head rotation when head movement does not occur. This spinning sensation is known as vertigo.14 Vertigo is resolved if the brain is able to adapt to the mismatch. For further information on vertigo, refer to the section on the vestibular system.
Finally, the central processing mechanisms combine any available and accurate inputs to answer the questions “Where am I?” and “How am I moving?” This includes both an internal relation of the body segments to one another (e.g., head in relation to trunk, trunk in relation to feet) and an external relation of the body to the outside world (e.g., feet in relation to surface, arm in relation to handrail). CNS disease or trauma involving the parietal lobe may impair these processing mechanisms so that even available, accurate sensory inputs are not recognized or incorporated into determinations of position and movement.18,19 Impairments of central sensory processing may occur after stroke, head trauma, tumors, or aneurysms; with disease processes such as MS; and with aging.
Central motor planning and control
Whereas sensory processing allows the interaction of the individual and the environment, motor planning underlies the interaction of the individual and the task. Aside from reflexive activity such as breathing and blinking, most motor actions are voluntary and occur because some goal is to be achieved. That is not to say that reflexes occur separately from volitional movements; for example, the vestibuloocular reflex is active concurrently with visual tracking activity, but most actions occur because of some purposeful intent.14 These task intentions precede motor actions.10,20 Wrist and hand movements vary depending on what is to be grasped (a cup versus a doorknob); foot placement and trunk position vary depending on what is to be lifted (a heavy suitcase versus a laundry basket). The initiation of volitional motor actions depends on intention, attention, and motivation.10,21
Once an objective (“Where do I want to be?” “What do I want to do?”) has been chosen, the next step in motor planning is to determine how to best accomplish the goal given the many options that are potentially available. For example, when the task demands fine skills or accuracy, the dominant hand is preferred; when the task involves lifting a large or heavy object, both hands are preferred. In addition to which limbs, joints, and muscles will be used, motor planning also adjusts the timing, sequencing, and force modulation. This can be demonstrated in various reaching tasks. Reaching to remove a hot item from the oven will occur slowly, whereas reaching to put an arm through a sleeve will occur more quickly. Optimal motor plans are developed with knowledge of self (abilities and limitations), knowledge of task (characteristics of successful performance), and knowledge of the environment (risks and opportunities).21
Clients with CNS disorders often have central motor planning and control system problems. After a stroke, clients may have hypertonus and poor reciprocal inhibition; clients with head trauma may have difficulty initiating or ceasing movements; clients with Parkinson disease exhibit bradykinesia; and those with cerebellar ataxia display modulation problems.22
Peripheral motor execution
Movement is accomplished through the bilateral joints and muscles. Normal range of motion (ROM), strength, and endurance of the feet, ankles, knees, hips, back, neck, and eyes must be present for the execution of the full range of normal balance movements. Decreased ankle dorsiflexion ROM, for example, restricts the forward limits of stability. Strength deficits are a primary cause of movement abnormalities in both central and peripheral nervous system disorders. In addition, weakness may be the result of force modulation deficits or disuse.11 Balance is directly affected by loss of strength. For example, weakness of the hip extensors and abductors will impede successful use of a hip strategy for upright trunk control. Initially adequate toe clearance may diminish with fatigue. Many clients with neurological issues also have stiffness and contractures as a result of persistent weakness or hypertonus. Restrictions in ROM also limit balance abilities.
The ability to achieve static postural alignment, although necessary for normal balance, is not sufficient to allow volitional functions. Adequate strength (to control body weight and any additional loads) through normal postural sway ranges is needed to permit dynamic balance activities such as reaching, leaning, and lifting. Postural control demands are increased during gait because the forces of momentum and the interaction between recruitment, timing, and velocity also must be regulated.23 Traditionally considered orthopedic problems, deficits in strength, ROM, posture, and endurance have a great impact on balance abilities. Attention must be given to these musculoskeletal system problems in examination of and intervention for clients with neurological diagnoses.
Influence of other systems
Balance abilities are also influenced by other systems. Attention, cognition and judgment, and memory are critical for optimal balance function and are often impaired in hemiplegic and head-injured clients as well as those who have progressive neurological disorders. Attentional deficits reduce awareness of environmental hazards and opportunities, interfering with anticipatory postural control.12 When balance is threatened, an inability to allocate attention to the necessary task of balance versus a secondary, less necessary task increases the risk of falls. Cognitive problems such as distractibility, poor judgment, and slowed processing also increase the risk of falls. Memory loss may preclude recall of safety measures. Depression, emotional lability, agitation, or denial of impairments also can increase the risks for loss of balance. In addition to having a direct impact on balance abilities themselves, these cognitive and behavioral problems impede motor learning processes, which are crucial for the relearning of balance skills.
Constant cyclic nature
The systems model of postural control previously presented illustrates the constant cycle that simultaneously occurs at many levels. Attention and intention allow feed-forward processing for active sensory search of the environment and motor planning, both of which are needed for anticipatory postural control. Movements are initiated and executed with resultant sensory experiences and error detection, or feedback. Successful movements are repeated and refined; unsuccessful ones are modified. The nature of this cycle presents the clinician with opportunities for intervention after the appropriate examination of sensory, motor, and cognitive functions. Through feedback and practice, balance abilities can improve.24
Motor components of balance
Reflexes
Many levels of neuromuscular control must be functioning to produce normal postural movements. At the most basic level, reflexes and righting reactions support postural orientation. The VOR and the vestibulospinal reflex (VSR) contribute to orientation of the eyes, head, and body to self and environment.10
When motion of the head is identified by the semicircular canals, it triggers a response within the oculomotor system called the vestibuloocular reflex. This causes the eyes to move in the opposite direction of the head but at the same speed. Stimulation of the otoliths drives the eyes to respond to linear head movement. Quick movements of the head will trigger the VOR.25
The VOR allows the coordination of eye and head movements. When the eyes are fixed on an object while the head is moving, the VOR supports gaze stabilization. Visuo-ocular responses often work concurrently with the VOR. They permit “smooth pursuit” when the head is fixed while the eyes move and visual tracking when both the eyes and the head move simultaneously.10
The VSR helps control movement and stabilize the body. Both the semicircular canals and the otoliths activate and modulate muscles of the neck, trunk, and extremities after head movement to maintain balance. The VSR permits stability of the body when the head moves and is important for the coordination of the trunk over the extremities in upright postures. Righting reactions support the orientation of the head in relation to the trunk and the head position relative to gravity and include labyrinthine head righting, optical head righting, and body-on-head righting.10
Automatic postural responses
At the next level, automatic postural responses operate to keep the COG over the base of support. They are a set of functionally organized, long-loop responses that act to keep the body in a state of equilibrium.3,4 Functionally organized means that the responses, although stereotypical, are matched to the perturbing stimulus in direction and amplitude. If the stimulus is a push to the right, the response is a shift to the left, toward midline. The larger the stimulus, the greater the response. Automatic postural responses always occur in response to an unexpected stimulus and are typically triggered by somatosensory inputs. Because they occur rapidly, in less than 250 ms, they are not under immediate volitional control.
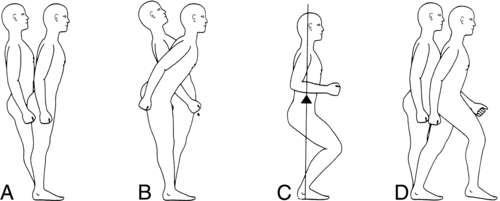
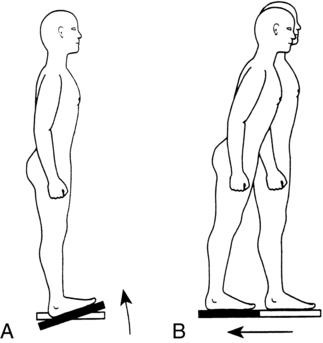
Four automatic postural responses have been described. Ankle strategy describes postural sway control from the ankles and feet. The head and hips travel in the same direction at the same time, with the body moving as a unit over the feet (Figure 22-2, A). Muscle contractile patterns are from distal to proximal (i.e., gastrocnemius, hamstrings, paraspinals). This strategy is used when sway is small, slow, and near midline. It occurs when the surface is broad and stable enough to allow pressure against it to produce forces that can counteract sway to stabilize the body. Ankle strategy is typically used to control anterior-posterior sway, because most of the degrees of freedom at the ankle are in this direction.
Hip strategy involves postural sway control from the pelvis and trunk. The head and hips travel in opposite directions, with body segment movements counteracting one another (Figure 22-2, B). Muscle contractile patterns are from proximal to distal (i.e., abdominals, quadriceps, tibialis anterior). This strategy is observed when sway is large, fast, and nearing the limit of stability or if the surface is too narrow or unstable to permit effective counterpressure of the feet against the surface. Hip strategy is used to control both anterior-posterior and medial-lateral sway. Hip strategy in the medial-lateral direction involves weight shifts from foot to foot; any client with difficulty weight-shifting quickly and accurately will have difficulty with medial-lateral hip strategy.
Suspensory strategy involves a lowering of the COG toward the base of support by bilateral lower-extremity flexion or a slight squatting motion (Figure 22-2, C). By shortening the distance between the COG and the base of support, the task of controlling the COG is made easier. This strategy is often used when a combination of stability and mobility is required, as in windsurfing.
Stepping and reaching strategies involve steps with the feet or reaches with the arms in an attempt to reestablish a new base of support with the active limb(s) when the COG has exceeded the original base of support (Figure 22-2, D). A successful stepping strategy is the best way to avoid a fall after a slip or trip.
Misconceptions about these APR strategies are common. First, these strategies do not function in daily life as separately as they are described in the early research literature. In quiet standing, for example, frequency analysis of unperturbed postural sway in healthy adults reveals that both ankle and hip strategies occur in combination, simultaneously.26 In perturbation studies, mixed use of strategies is often seen unless the perturbation is clearly below or above certain-sized thresholds. Second, these strategies occur in response to disturbances from all directions, not just in pure anterior-posterior or medial-lateral directions.27 Third, although these strategies are stereotypical in humans, great individual variation in strategy selection and performance comes from other influential factors. For example, many people use stepping strategy for most perturbations unless specifically instructed not to step or unless the conditions do not permit a step. An anxious person may reach or step much sooner than a relaxed person with similar physical deficits. Last, all these strategies do not occur in sequence with every balance disturbance.28,29 In other words, individuals normally do not try ankle strategy and wait until it fails before trying hip strategy, then wait until it fails before trying stepping strategy (although early learning may involve such exploration). Because these responses must occur extremely rapidly to prevent balance loss, such a sequential approach would be inefficient and ineffective. Instead, the normal response is the emergence of the single strategy best suited to the particular perturbation, the limitations of the individual, and the conditions in the environment.
Abnormal use of automatic postural responses is often observed in individuals with neurological disorders. Clients with vestibular deficits typically rely on ankle strategy, which permits the head to remain aligned with the body and sustains congruence between vestibular and somatosensory inputs. Use of hip strategy may be modified or limited because when the head is moving in the opposite direction as the COG, vestibular and somatosensory inputs are not congruent. Activities that require use of hip strategy, such as standing in tandem or on one leg, can be a problem for clients with bilateral vestibular loss or an uncompensated vestibular lesion. However, some cases involve excessive use of hip strategy on a level surface (when an ankle strategy would suffice).30 This may reflect abnormal integration of the somatosensory and vestibular information. If peripheral somatosensation is impaired, as in diabetic neuropathy, or central sensory weighting of somatosensory inputs is inadequate, hip strategy may dominate.
Anticipatory postural adjustments
Anticipatory postural adjustments are similar to automatic postural responses, but they occur before the actual disturbance.20 If a balance disturbance is predicted, the body will respond in advance by developing a “postural set” to counteract the coming forces. For example, if an individual lifts an empty suitcase thinking it is full and heavy, the anticipatory forces generated before the lift (to counter the anticipated weight) will cause excessive movement and brief instability. Failure to produce these anticipatory adjustments increases the risk of sudden balance loss, creating the need to use rapid, reactive automatic postural responses to prevent a fall. For clients with deficits in reaction time or automatic postural responses, superior use of anticipatory postural control can help the client avoid the unexpected perturbations that make automatic postural responses necessary.
Clinical assessment of balance
Objectives of testing
When present, activity limitations need to be identified and measured. Functional scales are typically used to determine the presence and severity of these limitations, not necessarily why those limitations exist. From these functional tests, decisions can be made about whether to treat and, if so, what tasks need to be practiced. If treatment is indicated, clinicians must make judgments about what to treat. Further testing to identify and measure impairments is then necessary to know what systems are involved. A comprehensive evaluation of balance includes both functional and impairment tests.12
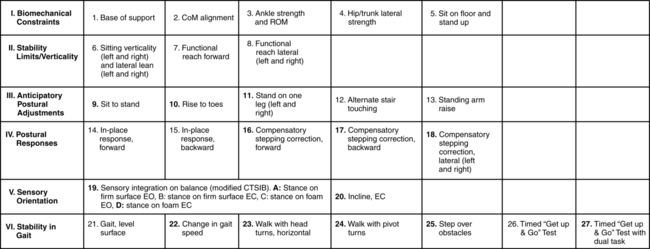
No single quick-and-easy test of balance can adequately cover the many multidimensional aspects of balance, although many such tests have great value as screening tools. However, a comprehensive test battery, called the Balance Evaluation Systems Test (BESTest), based on the systems model has been developed that provides clinicians with a thorough examination at the impairment level (Figure 22-3).31 The BESTest takes more time to administer than, for example, a single-leg stance test, but results from the BESTest give the clinician a far more complete and accurate picture of the client’s balance impairments than any single-item test or screening test can. Armed with these results, the clinician can develop interventions specifically targeted to the impaired systems. For clients whose primary problems include imbalance, the clinician’s investment of time to perform this comprehensive test battery yields a valuable outcome. A shorter version of this test, the mini-BESTest, has subsequently been published.32 It takes less time to administer but likewise provides a less complete picture of the client’s balance systems. Specifically, it does not include any items from the biomechanical constraints or stabilities limits categories. Even so, it is superior to single-item tests or screening tests that are not based on the systems model and do not identify balance system impairments that should be addressed in the intervention plan.
No single, simple test for balance is possible because balance is such a complex sensorimotor process.33 Many relatively simple balance tests exist, but not all tests are appropriate for all clients. Different tests may be needed to answer specific questions. For example, several good tests have been developed to determine the risk of falls in elderly people. These would be insufficient to discern whether an injured dancer can resume practice or an injured roofer is ready to return to work. Clinicians should understand the advantages and limitations of different balance tests to be able to select appropriate evaluative tools.
Because so many balance tests are available, several questions must be asked to determine whether a test is appropriate for use.33 For what purpose and population was the test designed? Can that test be used legitimately for a different purpose or with a different population? Is it valid? Is it repeatable by different examiners or by the same examiner multiple times? Are results reliable? In what populations are they reliable? What is the threshold for this test—that is, how large must performance changes be before this test can detect them? Are normative data available for comparison? These questions are being investigated but have not yet been answered for many of the clinical balance tests commonly used by therapists with the many different neurological populations they treat. Some of the evidence already reported may be frustrating to clinicians. For example, the Timed Up-and-Go test (TUG) predicts falls in community-dwelling older adults but not in acute-care hospital populations.34,35 For several balance tests such as the Functional Reach Test, the Berg Balance Scale, and others, the cutoff scores used for accurate prediction of falls in clients with Parkinson disease are different from the cutoff scores used in older adults without Parkinson disease.36 These examples make it clear that clinicians must understand their clients and the characteristics of the various balance tests in order to select the most appropriate tests and interpret test results for each client.
Types of balance tests
Balance tests can be grouped or classified by type. Different types of tests measure different facets of postural control (Table 22-1). Quiet standing (static) refers to tests in which the client is standing and the movement goal is to hold still. Disturbances to balance, called perturbations, may or may not be applied. Active standing (dynamic) tests also position the patient standing, but the movement goal involves voluntary weight shifting. Sensory manipulation tests use altered surface and visual conditions to determine how well the CNS is using and reweighting sensory inputs for postural control. Functional balance, mobility, and gait scales involve the performance of whole-body movement tasks, such as sitting to standing, walking, and stepping over objects. A few test batteries offer a combination of the preceding tests. The BESTest is the most comprehensive test battery to date. Dual-task tests have been developed to examine the effect of concurrent activities and divided attention on balance and mobility performance. A commonly accepted test for sitting balance in adults is not yet available, although clients with neurological problems often need sitting balance retraining in early stages. Clinicians typically modify standing tests or pediatric sitting tests to assess sitting balance in adult clients with neurological conditions. For example, the Functional Reach Test has been used to measure excursion in seated individuals with spinal cord injuries.37
TABLE 22-1 
| TYPE | TESTS |
| Quiet standing (with or without perturbation) | RombergSharpened Romberg or tandem Romberg One-legged stance test (OLST) Timed stance battery Postural sway Nudge or push Postural Stress Test Motor Control Test |
| Active standing | Functional Reach TestMulti-Directional Reach Test Limits of stability |
| Sensory manipulation | Sensory Organization Test (SOT)Clinical Test of Sensory Interaction and Balance (CTSIB) |
| Vestibular | Vertiginous positionsHallpike-Dix maneuver Nystagmus Semicircular canal function Visual-vestibular interaction Visual acuity Oculomotor tests Fukuda Stepping Test Dizziness Handicap Inventory |
| Functional scales | Berg Balance ScaleTimed Up-and-Go Test Tinetti Performance-Oriented Assessment of Balance Tinetti Performance-Oriented Assessment of Gait Gait Assessment Rating Scale (GARS) Dynamic Gait Index Functional Gait Assessment |
| Combination test batteries | Fregly-Graybiel Ataxia Test BatteryFugl-Meyer Sensorimotor Assessment of Balance Performance |
| Dual task | Stops walking when talkingMultiple Tasks Test |
Quiet standing
The classic Romberg test was originally developed to “examine the effect of posterior column disease upon upright stance.”38 The client stands with feet parallel and together and then closes the eyes for 20 to 30 seconds. The examiner subjectively judges the amount of sway. Quantification of sway can be accomplished with a videotape, forceplate, or, more recently, accelerometer.39,40 Excessive sway, loss of balance, or stepping during this test is abnormal. The sharpened Romberg,38 also known as the tandem Romberg, requires the client to stand with feet in a heel-to-toe position and arms folded across the chest, eyes closed for 60 seconds. Often four trials of this test are timed with a stopwatch, for a maximum score of 240 seconds.
One-legged stance tests (OLSTs) are commonly used.38,41 Both legs must be alternately tested, and differences between sides are noted. The client stands on both feet and places hands on the hips or crosses the arms over the chest, then picks up one leg and holds it with the hip in neutral and the knee flexed to 90 degrees. The lifted leg may not be pressed into the stance leg. This test is scored with a stopwatch. Five 30-second trials are performed for each leg (alternating legs), with a maximum possible score of 150 seconds per leg. Normal young subjects are able to stand for 30 seconds, but this may not be a reasonable expectation for frail older clients.38
A battery of timed stance tests has been developed by Bohannon and Leary.42 This set of tests varies the foot position (apart, together, tandem, and single leg) and the availability of visual information (eyes open and closed) to produce eight different combinations. Maintenance of balance in each condition is timed for a maximum of 30 seconds; the assigned score is the total number of seconds that balance could be maintained. The best possible score on this test is 240 seconds. This test is reliable, valid, and sensitive to change over time.42
A related test is the Balance Error Scoring System, or BESS test, which was developed for use with athletes to screen for concussion effects.43,44 The original BESS test involved three stance positions (double-leg stance with feet together, single-leg stance, tandem stance) on two surfaces (firm and foam), thus providing six conditions. The eyes are closed in all conditions. Each trial is 20 seconds in duration. The examiner observes and counts the number of balance errors that are made in each condition. The six observed errors include hands lifted off waist; opening eyes; step, stumble, or balance loss; moving a hip past 30 degrees of abduction; lifting the forefoot or heel; and remaining out of the test position for more than 5 seconds. If more than one error occurs at the same time, for example, opening eyes and hands off waist, only one error is counted. When measured in high-level young adults, the reliability of this test improved with the removal of the double-leg stance condition, which produced few to no errors in this high-functioning population, and the addition of three trials in each of the remaining four conditions. The modified BESS test thus includes only four conditions.45 This test has not been investigated for use in traditional neurological rehabilitation populations.
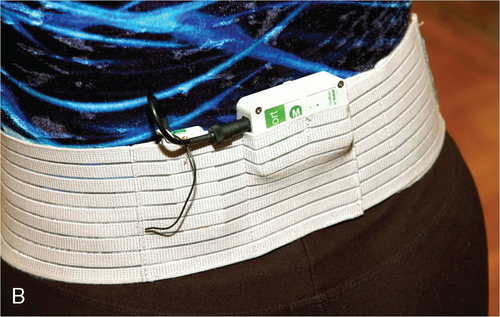
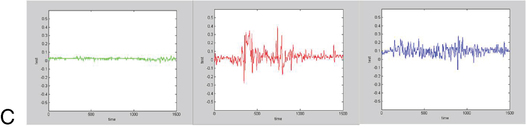
Objective postural sway measures can be obtained by computerized force plates (Figure 22-4) or wearable accelerometers (Figure 22-5).40,46–48 The client is asked to adopt a standardized foot placement if possible (this varies by manufacturer) and to stand quietly with arms at the sides or hands on hips for 20 or 30 seconds. Sway with both eyes open and eyes closed is commonly measured. Graphic and numerical quantification is provided. Normative data may be provided. These more technical measures are able to detect more subtle problems and are more sensitive to change in performance after treatment than are rating scales or timed measures.
Automatic postural responses are assessed by the client’s response to perturbations. It is imperative that clinicians include APR testing in their balance assessment because APRs are the motor responses necessary to prevent loss of balance and falls. The push-and-release test is a clinically useful method with a five-point ordinal rating scale.31,49,50 Testing for ankle and hip strategies (“in-place” strategies) requires that the clinician (1) place his or her hands on the front or back of the patient’s shoulders, (2) ask the patient to remain still and centered by resisting the pressure applied by the hands (producing isometric muscle activity), (3) watch for the toes or heels to begin to raise slightly (the clinician increases pressure until this occurs), then (4) suddenly release the push. Both forward and backward directions are tested; the clinician always stands where he or she can support the client in case of balance loss. Testing for stepping strategy follows the same concept but is performed differently. Instead of keeping the client’s COG at midline, the client leans his or her weight into the clinician’s hands, shifting the COG away from midline toward the outer limit of stability before the release. The correct client response is to step to reestablish a new base of support underneath the new position of the COG. Forward, backward, and both lateral directions are tested. When nudge or push tests are performed predictably (i.e., “don’t let me push you backward”), this is assessment of anticipatory postural control. When the release happens unpredictably (no cues, unpredictable timing), automatic postural responses can be assessed. Perturbations of different strengths from multiple different directions should be given.
The Motor Control Test (MCT) is a computerized test of automatic postural responses that perturbs the client through surface displacement (Figure 22-6, B).3 The client stands on a dynamic (movable) forceplate with feet parallel and arms at sides. The support surface rapidly translates (slides) forward or backward. This surface displacement results in a rapid shift in the relation between the COG and the base of support. The expected responses are directionally specific (to the direction of the stimulus) forces generated against the surface to bring the COG back to the center. Response latencies, strength, and symmetry are measured. Normative data are available. This test can be used to look for abnormal stepping strategies when failure to select hip strategy occurs. The MCT is the most standardized and reliable test of automatic postural responses, but it is not widely used because it requires computerized equipment.
Active standing
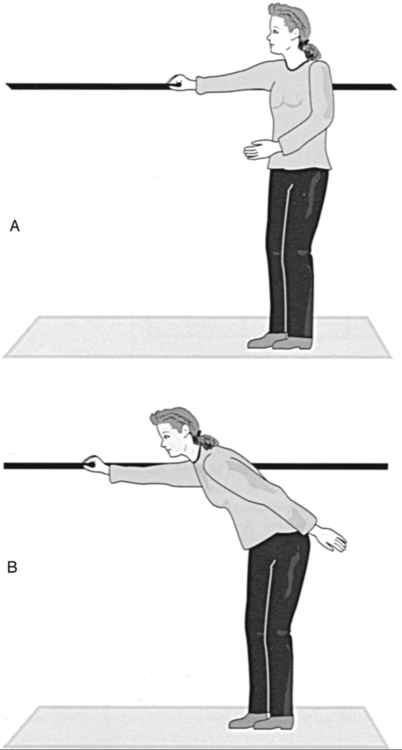
Volitional control of the COG is evaluated by asking the client to make voluntary movements that require weight shifting. The Functional Reach Test was developed for use with older adults to determine risk of falls.51 The client stands near a wall with feet parallel. Attached to the wall at shoulder height is a yardstick. The client is asked to make a fist and raise the arm nearest the wall to 90 degrees of shoulder flexion. The examiner notes the position of the fist on the yardstick. The client is then asked to lean forward as far as possible, and the examiner notes the end position of the fist on the yardstick (Figure 22-7). Beginning position is subtracted from end position to obtain a change unit in inches. Three trials are performed. Normative data are available, and the test is reliable. However, the standard error of measurement for this test may be as high as 2 inches, meaning that a change in score of less than 2 inches cannot be attributed to clinical improvement because it may reflect only measurement error. Subsequent studies have not shown that this test is useful for fall prediction.52–54
One serious limitation of the Functional Reach Test is that it measures sway in only one direction (forward). An expansion of this test has been devised to measure sway in four directions.55 The multidirectional reach test is conceptually equivalent but measures sway anteriorly, posteriorly, and laterally to both sides. This test should provide a more comprehensive picture of volitional COG control limitations. Validity and mean values have been established for community-dwelling older adults.56
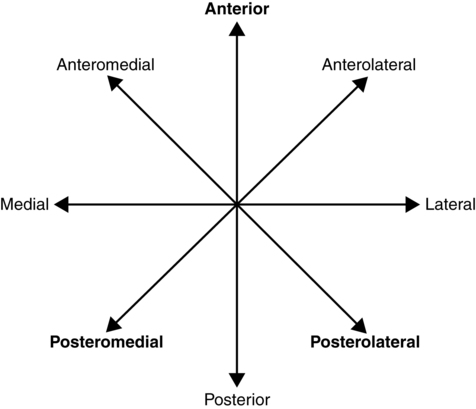
The limits of stability test uses a computerized forceplate to measure postural sway away from midline in eight directions.46,57 Clients assume a standardized foot position and control a cursor on the computer monitor by shifting their weight. They are asked to move the cursor from midline to eight targets on the screen (Figure 22-8). Measures include movement velocity, directional control (path sway), measures of excursion (length of the trajectory of the COG), and reaction time. This test should be performed once for familiarization, then a second time for scoring purposes. Second and subsequent tests are reliable. Normative data are available.
A very challenging test used primarily in athletic populations is the Star Excursion Balance Test (SEBT) (Figure 22-9).58,59 The SEBT could be used, for example, in high-level traumatic brain injury (TBI) clients who require more demanding test conditions. However, although there is evidence for the validity and reliability of this test in orthopedic populations, as yet this test has not been investigated for use in neurological populations. The SEBT is in concept a lower-extremity functional reach test, requiring single-leg stance on one leg and a reach with the other leg. The original SEBT included eight directions; currently the SEBT is typically performed in three directions: center-forward, right-rear, and left-rear.60 Three tape measures are taped to the floor, radiating out from the same center point. The two rear tape measures are at a 45-degree angle from the center line. The client stands on one foot with the great toe on the center point, then reaches the maximum distance away from the center with the lifted foot. The distance is recorded by the examiner. This is done in all three directions, with the lifted leg having to cross behind the stance leg to reach to the opposite-side rear tape. Six practice trials in each direction are given before recording scores to eliminate a learning effect, although recent evidence suggests four practice trials may be sufficient.61 Three scored trials in each direction are performed. Both legs are tested.61a
Sensory manipulation
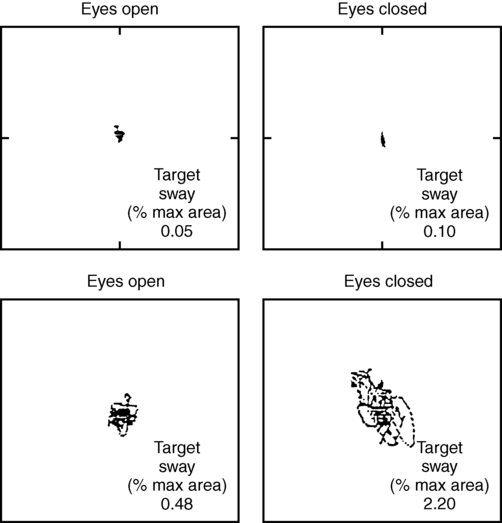
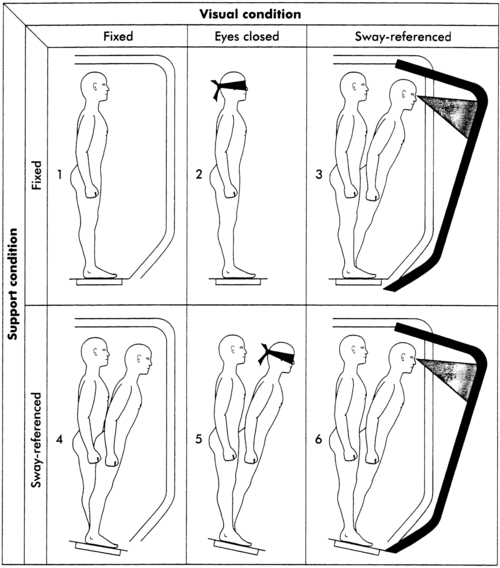
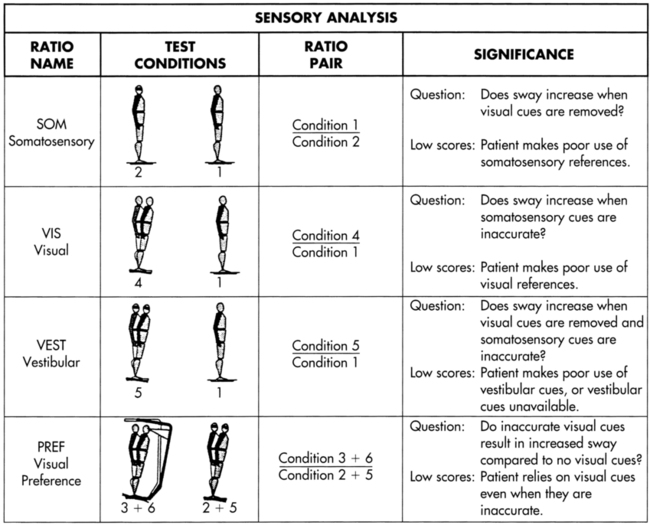
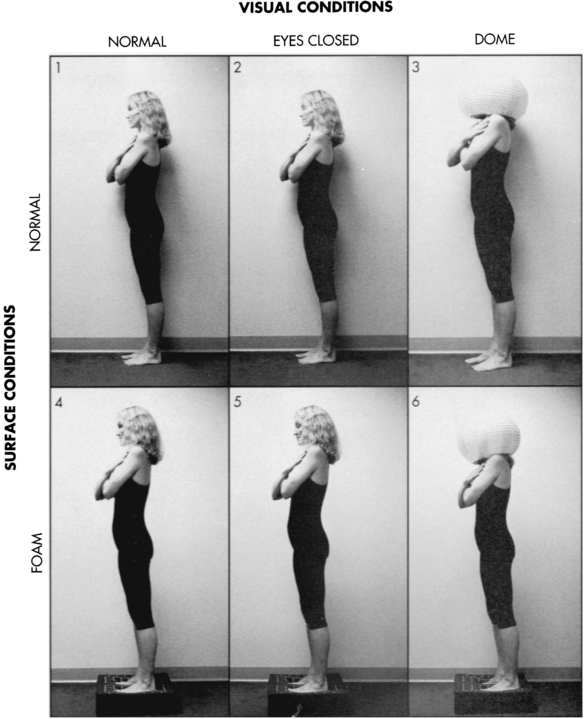
Sensory inputs play a critical role in postural control, but few tests to measure their use to produce a balance performance outcome have been developed. The Sensory Organization Test (SOT) uses a computerized, movable forceplate and movable visual surround to alter the surface and visual environments systematically.3,4 The client stands on the forceplate with feet parallel and arms at the sides and is asked to stand quietly. Three 20-second trials under each of six sensory conditions are performed (Figure 22-10). In conditions one, two, and three the support surface (forceplate) is fixed. During conditions four, five, and six the support surface is sway referenced to the sway of the client. In other words, the movement of the surface is matched to the movement of the client in a 1:1 ratio. This responsive surface movement maintains a near-constant ankle joint angle despite body sway, rendering the somatosensory information from the feet and ankles inaccurate for use in balance maintenance. Visual inputs are undisturbed in conditions one and four. Vision is absent (eyes are closed) in conditions two and five. The movable visual surround is sway referenced in conditions three and six. This responsive visual surround movement maintains a near-constant distance between the eyes and the visual environment despite body sway, rendering visual inputs from the eyes inaccurate for balance maintenance in those two conditions.
Under condition one, all three senses (vision, vestibular sense, and somatosensory sense) are available and accurate. Body sway is measured by the forceplate; this initial measurement forms the baseline against which subsequent measures are compared (Figure 22-11). Under condition two the eyes are closed, so only somatosensory and vestibular cues remain. In an individual with normal movement function, the somatosensory inputs will dominate in this condition. By comparing sway during condition two with sway during condition one, detection of how well the client is using somatosensory inputs for balance control is possible. Clients with somatosensory loss from spinal cord injury, diabetes, or amputation have difficulty in condition two. Functional situations with inadequate lighting or unusable visual cues (e.g., busy carpeting) are similar to condition two.
The Clinical Test of Sensory Interaction on Balance (CTSIB) is a clinical version of the SOT that does not use computerized forceplate technology.62 The concept of the six conditions remains intact (Figure 22-12). Instead of sway measures, the examiner uses a stopwatch and visual observation. A thick foam pad substitutes for the moving forceplate during conditions four, five, and six. In normal individuals and clients with peripheral vestibular lesions, measures with foam correlate to moving forceplate measures.63 Originally, a modified Japanese lantern substituted for the moving visual surround in conditions three and six. Studies have not shown that measures using the Japanese lantern correlate with the moving visual surround measures. Most clinicians now perform the modified CTSIB with just four conditions, eyes open and closed on a firm surface and eyes open and closed on the foam surface. The client is asked to stand with feet parallel and arms at sides or hands on hips. At least three and up to five 30-second trials of each condition are performed.18 The watch is stopped if the client steps, reaches, or falls during the 30 seconds. If the client is very steady for 30 seconds on the first trial of a condition, some clinicians choose not to test the remaining trials in that condition and will give the client a full score for that condition. A maximum score for five trials of each condition is 150 seconds. Individuals with normal movement abilities are able to stand without stepping, reaching, or exhibiting loss of balance for 30 seconds per trial per condition. It is normal for sway to increase slightly as the conditions increase in difficulty. The CTSIB may not be a reliable measure in clients with hemiplegia or other conditions that involve motor deficits in, or abnormal response time through, the lower extremities and trunk.64 The clinician can use the information regarding client response in a variety of environmental conditions to determine intervention management strategies.65
Active stepping
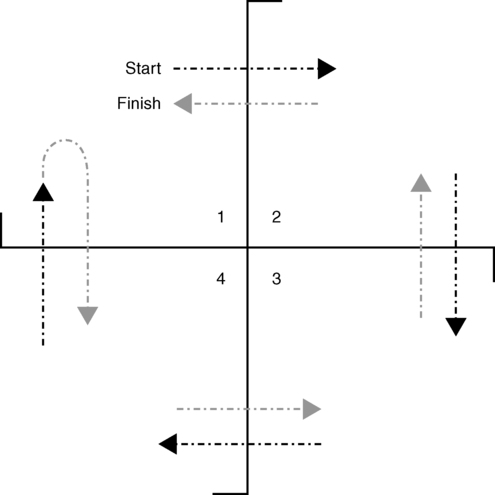
The ability to change the base of support without balance loss then to reestablish COG stability over the new base of support is a balance-dependent skill critical for functional activities. The four square step test is a timed stepping test in a standardized, structured format in forward, backward, and lateral directions (Figure 22-13).66 A simple plus sign–shaped grid is laid out on the floor using four straight canes, dowel rods, or plastic piping. This creates four quadrants. The client begins standing in the rear-left quadrant, steps forward over the first bar to stand with both feet in the front-left quadrant, steps rightward over the second bar to stand with both feet in the right-front quadrant, steps backward over the third bar to stand with both feet in the right-rear quadrant, steps leftward over the fourth bar to stand with both feet in the left-rear quadrant (starting location), then reverses direction, going back through each quadrant in the same way until standing again with both feet in the rear-left quadrant. The outcome measure is the time it takes the client to perform this task correctly, clearing each bar completely with each foot. This test has been used with older adults, individuals with vestibular disorders, and clients poststroke.67,68
Functional scales
The Berg Balance Scale consists of 14 tasks that the client is asked to perform.69 The examiner rates the client on each task by using an ordinal rating scale of 0 to 4, in which 0 is unable to perform and 4 is able to perform without difficulty. This test is highly reliable. It was originally designed for assessing risk of falls in older adults, and cutoff scores for fall risk vary depending on which of several studies is consulted.70,71 Use of higher cutoff scores may erroneously identify nonfallers as fallers; use of lower cutoff scores may erroneously identify fallers as nonfallers. The Berg Balance Scale has also been used with clients after stroke.72–75
The original Get-Up-and-Go Test is made up of seven items and subjectively scored on an ordinal rating scale of 1 to 5, in which 1 is normal and 5 is severely abnormal.76 This test has been modified by making it a timed measure to increase its objectivity and reliability, which is now high. The TUG test eliminates the “standing steady” segment and uses a stopwatch to time the performance.77 Clients are asked to rise from a chair with arms, walk 3 meters as fast as they safely can, turn, walk back to the chair, and sit down. This test may be performed with an assistive device; however, the use of a device will alter the speed at which the task can be accomplished, and any retesting must be done with the same device to produce comparable results. Originally designed to assess frailty in older adults, the test is now more commonly used to assess fall risk in this population. Young adults typically perform this task in 5 to 7 seconds, healthy older adults in 7 to 9 seconds (low risk), moderate-risk older adults in 10 to 12 seconds, and high-risk older adults in 13 seconds or more.78,79 These cut-off scores are for older adults walking without assistive devices. Improvements in test performance that are not captured by the time score alone should also be documented, for example, if the client can now perform the test without the use of chair arms to stand up, or without an assistive device.
The Tinetti Performance-Oriented Mobility Assessment—Balance subscale (POMA-Balance) is a list of nine items scored on scales of either 0 to 1 or 0 to 2, with the higher numbers reflecting better (more normal) performance.80 The score value is specific to the item. The best possible score is 16, with a score of 10 or lower indicating a high risk of falls.81
Most balance and mobility scales have been developed to assess risk of falls in older adults. Many share similar items. See Table 22-2 for a summary of scale items.
TABLE 22-2 
BALANCE AND MOBILITY SCALE ITEMS
| ACTIVITY | BERG BALANCE SCALE | DYNAMIC GAIT INDEX | TIMED UP-AND-GO TEST | TINETTI BALANCE ASSESSMENT |


































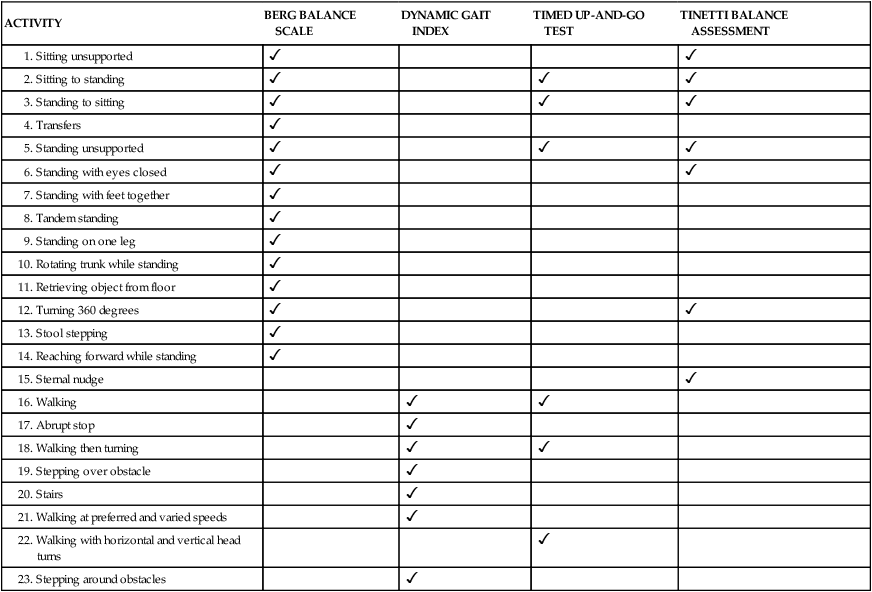
The Tinetti Performance-Oriented Mobility Assessment—Gait subscale (POMA-Gait) is a list of seven normal aspects of gait that are observed by the examiner as the client walks at a self-selected pace and then at a rapid but safe pace.80 Scoring scales are again either 0 to 1 or 0 to 2, and higher numbers indicate better performance. Score values are specific to the item being observed (Table 22-3). The best possible score is a 12; scores of 8 or below indicate a high risk of falls. When combined, the Tinetti POMA balance and gait scales offer a best possible score of 28, with scores of 19 or less indicating a high fall risk.
TABLE 22-3 
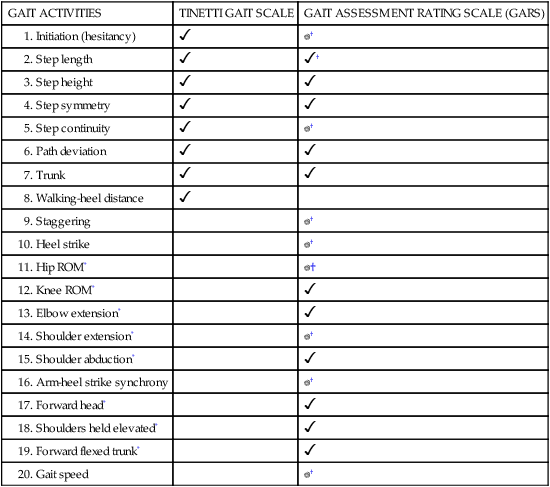
The original Gait Assessment Rating Scale (GARS) is a list of 16 abnormal aspects of gait observed by the examiner as the client walks at a self-selected pace (see Table 22-3).82 These abnormalities are commonly seen in older adults who fall, who are fearful of falling, or both. The items are scored on a scale of 0 to 3, with lower numbers reflecting better (less abnormal) performance. The best possible score is 0. This gait scale provides some relative numerical indication of the quality of gait. A shorter, modified version of this test, the Modified GARS, has been developed. The Modified GARS (GARS-M) includes nine of the original items plus a gait velocity measure. It provides equivalent sensitivity and takes less time to perform.83 These two gait scales were developed to assess risk of falls in older adults.
The Dynamic Gait Index (DGI) is a gait test specifically designed to look at postural control during gait.12 It includes eight items requiring changes in gait speed, walking with horizontal and vertical head turning, whole-body turns during gait, stepping over and around obstacles, and stair ascent and descent. Items on this test are scored on a 4-point ordinal scale of 0 to 3, with 3 being normal performance and 0 indicating severe impairment. The best possible score on this test is a 24, and scores of less than 19 points have been associated with impairment of gait and fall risk. The presence of head motion and whole-body turns in this test may help identify clients with potential vestibular dysfunction. The reliability of this test is high.71,84,85 A modified and slightly more difficult version of this test, the Functional Gait Assessment (FGA), has been developed specifically for use with patients with vestibular disorders.86 The best possible score on the FGA is 30 points, and a score of 22 points or below can be used to classify fall risk and predict unexplained falls in community-dwelling older adults.87
The three gait tests listed previously are distinct from traditional gait tests because they focus on elements of postural control during gait. One very important traditional gait measure that should be included in the assessment of balance and gait in older adults and clients with neurological disorders is gait speed. This measure has been termed “the sixth vital sign” for older adults because of its strong association with level of dependence in activities of daily living (ADLs) and instrumental ADLs (IADLs), probability of hospitalization, risk of falls, eventual discharge location, and ambulation category.88
Combination test batteries
The BESTest is an excellent comprehensive test battery based on the systems model of postural control (see Figure 22-3).31 It includes seven categories representing components of postural control: biomechanical constraints; stability limits; anticipatory postural adjustments; automatic postural responses; sensory orientation, and stability during gait. Within each category are individual test items and, in some cases, existing tests. For example, the sensory orientation category contains the individual item “Stand on incline with eyes closed” and the four-condition CTSIB discussed earlier. Although the BESTest takes approximately 30 minutes to administer, the information acquired helps to identify which underlying components of the postural control system are causing the observed balance problems. Armed with this critical information, the clinician can design a customized, individualized intervention program that targets the sources of imbalance in each client.
A shorter version of this test has been developed, the Mini-BESTest (see Figure 22-3).32 It includes 14 of the original 36 items, has a compressed rating scale, and takes approximately 15 minutes to administer. It does not include any items from the biomechanical constraints category or the stability limits category. This does not mean that these components need not be measured. Biomechanical constraints such as hip and ankle weakness, and constricted limits of stability, seriously negatively affect balance and should be tested in addition to administration of the Mini-BESTest. The compressed rating scale may reduce the ability of this test to reflect a client’s progress over time.
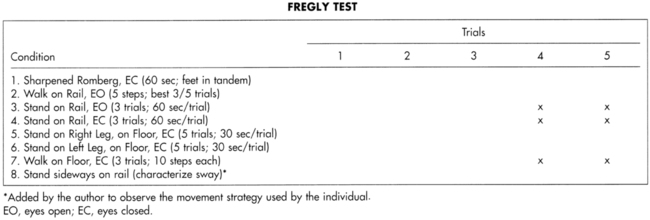
The Fregly-Graybiel Ataxia Test Battery is a more challenging test appropriate for clients with higher-level balance skills. It includes eight test items that the client must perform (Figure 22-14).38 Standing trials in tandem stance both off and on a rail with eyes open and closed are timed. Timed single-leg stance trials also are performed for each leg. Walking 10 steps with eyes closed is included. Five trials of each task are given. Trials are stopped if the client uncrosses the arms, opens the eyes (during eyes-closed trials), steps (during standing trials), or falls. Trials are judged on a pass-fail basis. This test battery is valid for use with clients who have peripheral vestibular dysfunction. Normative data are available from a normative database composed primarily of findings in young men. As noted earlier, clients must be at a high level motorically to perform these tasks. This test is a good choice for clients with higher-level abilities because it does provide more demanding balance tasks. Interpretations regarding a client’s use of sensory inputs when motor involvement is also present cannot be made with certainty.
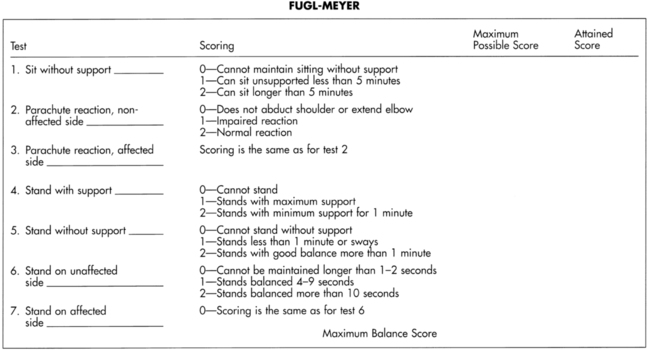
The Fugl-Meyer Sensorimotor Assessment of Balance Performance is a subset of the Fugl-Meyer Physical Performance Battery, which was designed for use with hemiplegic clients (Figure 22-15).18 Three sitting and four standing balance activities are listed. The items are scored on a 0 to 2 scale, with score values specific to each item. Higher scores indicate better performance; the maximum (best) score is 14. However, a client could achieve this score of 14 and still not have normal balance.
The Dizziness Handicap Inventory (DHI) was developed to identify specific functional, emotional, or physical problems associated with an individual’s reaction to imbalance or dizziness.89,90 The DHI assesses the client’s perception of the effects of the balance problem and the client’s level of emotional adjustment. It also looks at perceived physical limitations as a consequence of the disorder. Twenty-five items are divided into three subscales in this self-assessment inventory. Included are a nine-item functional scale, a nine-item emotional scale, and a seven-item physical scale. Each item is assigned a value of four points for a “yes,” two points for a “sometimes,” and zero points for a “no.” This inventory is reliable, is easy to administer, and can be used to evaluate treatment outcomes.91 Changes in scores on the functionally based DHI correlate highly with changes in scores on the impairment-based SOT.89
Dual-task tests
In everyday life tasks, normal balance is largely unconscious and does not compete for attentional resources. In clients with balance disorders, however, the challenge of maintaining postural control during upright activities and gait is often sufficient to demand the use of attentional resources. The interaction of cognitive demands and postural control demands is examined in dual-task tests that add concurrent cognitive and motor tasks to gait tasks. At the simplest level are the walking while talking (WWT) and stops walking when talking (SWWT) tests.92–95 In these tests the client is asked to walk and, while the client is walking, the clinician asks the client one or more questions and observes if the client must stop walking to answer the question(s). If so, the test result is positive—that is, the client must stop attending to the postural control demands of walking to reallocate attention to the cognitive task. These are gross measures, apt to identify only those with more severe attentional balance problems or to misidentify clients who prefer to chat and rest rather than keep walking. A more formalized dual-task test is the Multiple Tasks Test (MTT), which includes eight items involving gait plus other verbal cognitive and motor tasks such as carrying a tray and avoiding obstacles.96,97 Two dual-task versions of the TUG have been developed. The TUG-Manual involves performing the TUG while carrying a cup nearly full of water. The TUG-Cognitive involves performing the TUG while subtracting backward from a randomly selected number or spelling words backward.98 The Walking and Remembering Test (WART) requires the client to remember a set of numbers that the tester speaks aloud while the client walks as quickly as possible while trying not to step off of a narrow path.99 Once the walk is completed, the client must repeat the numbers in sequence. For all dual-task tests, performance of each single task is measured separately first. Then the dual-task performance is recorded. The difference for each of the two scores (physical and cognitive performance) between undivided attention and divided attention conditions is calculated.
Balance confidence tests
Reduced participation in functional activities may occur not only because balance impairments impede participation, but also when clients are anxious about falling. Fear of falling may lead individuals to avoid activities that they remain quite capable of doing.100 In turn, prolonged self-restriction of activity leads to the many negative consequences of being sedentary—decreased ROM, weakness, low endurance, and so on—and thus ironically further impairs balance and increases fall risk.101,102 As this worsening balance and increased risk is perceived by the client, further activity restriction occurs, creating a self-perpetuating downward spiral leading to social isolation, anxiety, and depression.103,104 It is just as important to address poor balance confidence as it is to address poor balance, for without sufficient balance confidence a client will not participate in activities even if balance abilities permit him or her to do so. The client will lose all the gains made in therapy if he or she does not remain active, and he or she will not be active if fearful of falling.
The two most commonly used measures of balance confidence are the Activities-specific Balance Confidence Scale (ABC Scale), and the Falls Efficacy Scale (FES).105,106 Both are questionnaires that are easy to administer. The ABC Scale consists of 16 items that range in difficulty from “walk around the house” to “walk outside on icy sidewalks.” Several of the items inquire about activities in public places, for example, parking lots and escalators. Clients are asked how confident they are that they could do each of the activities without losing their balance or becoming unsteady. Responses are given on a scale from 0 to 100 in increments of 10, with higher numbers indicating higher confidence. More recently a short version, the ABC-6, has been developed. It has six of the original 16 items and takes less time to administer, yet retains good reliability and correlation with balance and fall risk measures.107 The FES consists of 10 activity items that are less difficult than the items on the ABC Scale. Items on the FES include getting in and out of a chair and answering the door or a phone. All of the items refer to activities done in the home. Clients are asked how confident they are that they could do each of the activities without falling. Responses are given on a scale from 1 to 10, with lower numbers indicating higher confidence. The Modified FES (MFES) has 14 activity items and includes two activities done outside the home and three activities done in public spaces. It also takes into account whether or not an assistive device is used.108 Scoring is identical to that of the original FES.
A third measure of fear of falling is the Survey of Activities and Fear of Falling in the Elderly (SAFFE).109 This measurement instrument is more involved than the ABC Scale or MFES; however, it provides additional information specific to activity restriction that is valuable to the clinician. The SAFFE has 11 activity items that are similar in nature to the items on the other two scales, including community activities. This questionnaire asks if the client actually does the activity or not. If he or she does the activity, the questionnaire asks how worried the client is that he or she might fall during the activity, on a scale from 1 to 4. Lower numbers indicate increased worry. If the client does not do the activity, the client is asked whether the reason he or she does not do the activity is fear of falling, with degree of fear scored on the scale from 1 to 4, or whether the client does not do the activity for reasons other than fear, and what those other reasons are. For each item, clients also indicate whether the frequency of doing the activity has increased, decreased, or remained the same. The SAFFE takes longer to administer than the ABC Scale or MFES but provides explicit results about activity restriction not obtained from the other two scales.
The Fear of Falling Avoidance Behavior Questionnaire (FFABQ) is a recently developed instrument with a focus on activity avoidance versus fear.110 It lists 14 different activities, ranging in difficulty from walking and preparing meals to going up and down stairs to engaging in recreational activities such as sports or traveling. Clients rate whether or not they agree with a statement that they avoid a specified activity on a 5-point scale from 0 (completely disagree) to 4 (completely agree). This questionnaire is reliable, with scores that discriminate between previous fallers and nonfallers, and more versus less active individuals. The shift from an emphasis on fear or confidence as in the ABC and FES, to activity avoidance as in the SAFFE and FFABQ is an important and positive one for physical and occupational therapists. As the ICF health and disablement model describes, our goals are to increase activity and participation to achieve an improved quality of life for our clients.
Problem identification, goal setting, and treatment planning
Clinical decision making
Treatment of clients with neurological diagnoses is based on the particular set of impairments and activity limitations possessed by each individual. Remediation of balance deficits similarly must be specific to the involved body systems and functional activity losses in each client. Clinicians should generate an overall problem list for each client; if imbalance is a listed problem, then a sublist of balance problems also can be developed (Figure 22-16).
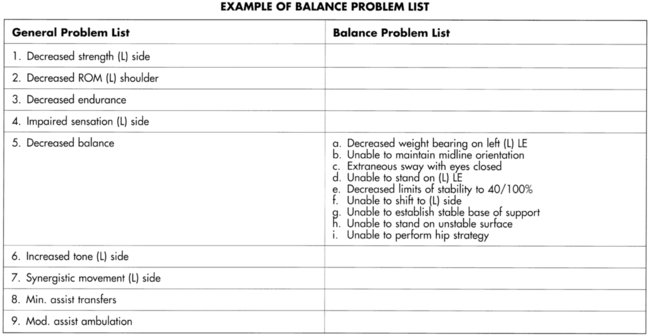
 An example of a balance-specific problem list (as a subset of a general problem list), which should be developed to guide balance rehabilitation treatments.
An example of a balance-specific problem list (as a subset of a general problem list), which should be developed to guide balance rehabilitation treatments.To direct and establish priorities for treatment, clinicians must review the problem list and ask themselves the following questions (Figure 22-17): Which impairments are temporary and can be remediated? How much improvement can be expected? How soon will it occur? Which impairments are permanent or progressive and must be compensated for? What other body systems can be counted on to substitute? What external compensations may be needed?
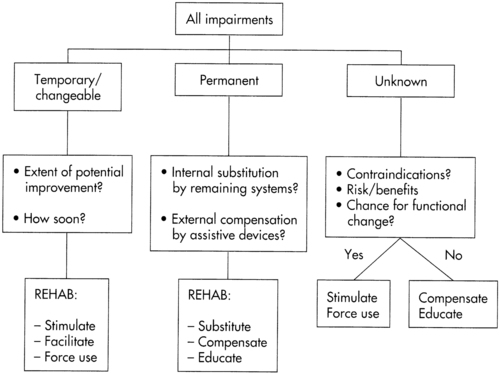
 A clinical decision-making tree to illustrate the treatment-planning process in balance rehabilitation.
A clinical decision-making tree to illustrate the treatment-planning process in balance rehabilitation.Using the systems model to identify postural control impairments
The systems approach is useful to develop a balance problem list because it can be applied to different diagnoses equally well and allows deficits in multiple systems to be recognized. Table 22-4 illustrates several examples of ways this framework is used to identify balance deficits in clients with different neurological diagnoses.
TABLE 22-4 
EXAMPLES OF MEDICAL DIAGNOSES AND RELATED IMPAIRMENTS AFFECTING BALANCE
| IMPAIRMENTS FROM SYSTEMS MODEL | CLIENT WITH DIABETIC STROKE | CLIENT WITH PARKINSON DISEASE | CLIENT WITH INCOMPLETE PARAPLEGIA |
| PERIPHERAL SENSORY | |||
| Vision | Retinopathy | Cataracts | |
| Vestibular | Hair cell loss | ||
| Somatosensory | Peripheral neuropathy | Slowed transmission time | Complete loss |
| CENTRAL SENSORY | |||
| Vision | Hemianopia | Vision dominant | Needs superior use to compensate |
| Vestibular | Failure to use inputs | Needs superior use to compensate | |
| Somatosensory | Failure to use inputs | Failure to use inputs | |
| Strategy selection | Step dominant | Ankle dominant | Hip dominant |
| Perception of position in space | Midline shift with left neglect | Restricted limits of stability | |
| CENTRAL MOTOR | |||
| Timing | Increased reaction time | Bradykinesia | |
| Sequencing | Disordered | Co-contraction | |
| Force modulation | Spasticity | Rigidity | |
| Error correction | Use right side only | ||
| PERIPHERAL MOTOR | |||
| Range of motion | Knee hyperextension | Bilateral ankle plantar flexor contractures | Hip flexion contractures |
| Strength | Decreased left side | Decreased bilateral extremities and trunk | Severe weakness bilateral lower extremities and trunk |
| Endurance | Severely impaired | Moderately impaired | Mildly impaired |
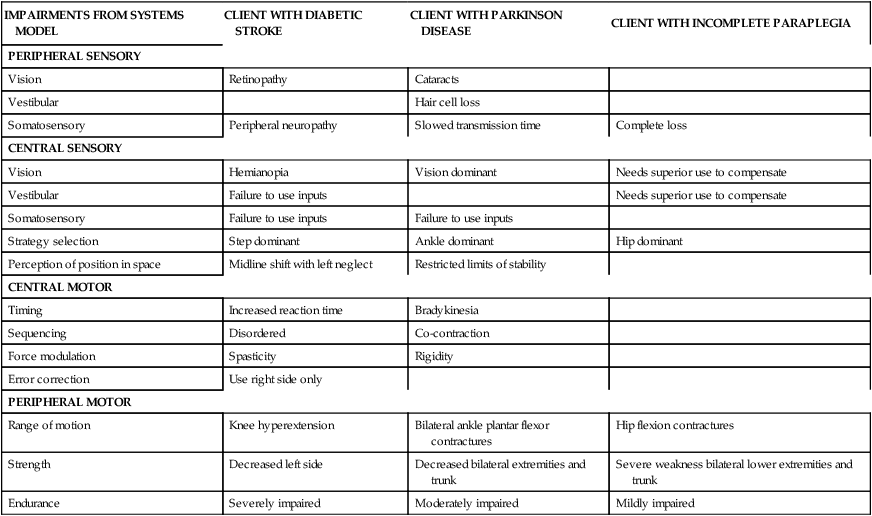
For each client, problems affecting postural control should be described in objective, measurable terms whenever possible. For example, the term “impaired vision” is too vague; “four-line drop on eye chart” is more specific. “Poor use of visual inputs for balance control” is an interpretation; the objective result could be stated “Loss of balance after less than 15 seconds on 5/5 trials of standing on foam, eyes open.” Documenting problems in this manner makes goal writing (and subsequent treatment planning) much easier.
Developing A treatment plan
The clinician must thoughtfully choose environments and tasks that together stimulate and challenge the appropriate postural control systems. To stimulate one sensory system, the other systems must be placed at a disadvantage to force reliance on the targeted system. The environment is then structured to put the other systems at a disadvantage (e.g., training with eyes closed or in the dark puts vision at a disadvantage and forces the use of somatosensory and vestibular inputs). If one side or limb is significantly more affected, such as in hemiplegia, then the other side must be disadvantaged to force reliance on the targeted side. Tasks are then selected to disadvantage the less affected side. For example, placing the less affected leg on a step or small ball makes it more difficult to use for balance and forces the transference of weight to the more affected leg. To achieve optimal function, however, all systems and all sides must be capable of working together, so training to improve balance impairments must be incorporated and interspersed with training functional tasks. For carryover of improvements into real-life situations, training tasks should be varied enough to promote motor problem solving on the part of the client.111 For example, sitting balance and transfers should be taught using stable and unstable surfaces, with different heights and firmnesses, with and without armrests and back supports, and using both right and left sides. This technique may improve the client’s abilities to perform safe sitting and transfers in new situations not previously practiced in therapy.24
Tables 22-5 through 22-7 illustrate the process of test choice, problem identification based on test results, goal setting based on impairments and disabilities, and treatment planning based on goals in three different types of clients. Note that only selected tests were performed for each client. Goals were directly related to the problems that were identified by the tests, and treatment plans followed directly from the goals.
TABLE 22-5 
| Patient profile: 50-year-old woman | |||
| Diagnosis: Uncompensated (R) unilateral peripheral vestibular deficit for 6-7 years | |||
| Course of examination and treatment: Otolaryngologist → psychologist → neuro-otologist → outpatient physical therapy | |||
| TEST | PROBLEMS IDENTIFIED | GOALS SET | TREATMENT PLAN |
| Visual acuity | Four-line drop on Snellen eye chart | Able to read chart with only one-line drop | Gaze stabilization exercises |
| Oculomotor | Positive nystagmus with Frenzel lenses | ||
| Saccades | |||
| Pursuit | |||
| Nystagmus | |||
| Gaze stabilization Visual-vestibular interaction |
Unable to perform test ↓ Fixation with horizontal + vertical head movements after 5-10 s |
Able to rotate head horizontally 2 min without problems | Gaze stabilization exercises |
| VOR cancellation Hallpike |
Able to perform visual-vestibular interaction test | ||
| SOT | Decreased use of somatosensory inputs 70/100 Decreased use of visual inputs 55/100 Absent use of vestibular inputs 0/100 Unable to resolve visual conflict 0/100 |
Somatosensory use 100/100 Vision use 90/100 Vestibular use 70/100 Visual conflict resolution 90/100 |
Sensory environment stimulation |
| Limits of stability | Restricted anteriorly and posteriorly to 35% limit of stabilitySlow movement time | Limits of stability expanded to 85% anterior and posterior at 5-s pacing | COG control training |
| ROM and strength | None | ||
| Gait | Gait training | ||
| Eyes open | Weaves side to side | ||
| Eyes closed | Deviates to (R) with eyes closed | Walks in a straight line with eyes closed | |
| Head turning | Dizzy with horizontal head turns | Walks with only slight deviation with eyes closed and head turning | |
| Pivots | Loss of balance and dizzy with (R) pivot | Spins to (R), (L) with eyes closed | |
| Abrupt stops | Very unsteady with abrupt stop; feels “off” | Comes to abrupt stop steadily |
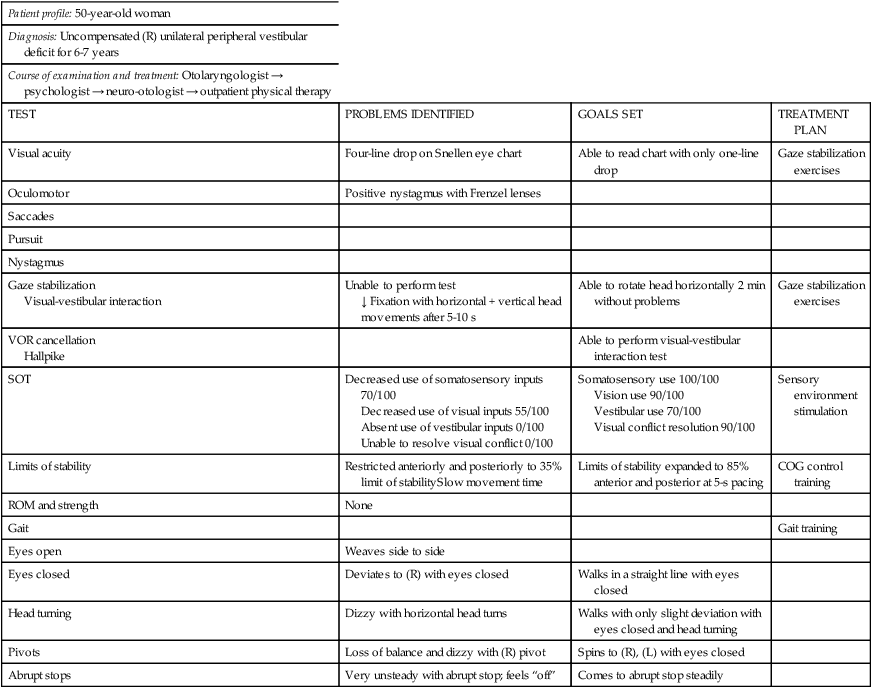
COG, Center of gravity; (L), left; (R), right; ROM, range of motion; SOT, Sensory Organization Test;
Reprinted with permission from NeuroCom International, Clackamas, Ore.
TABLE 22-6 
EXAMPLE OF HOW TREATMENT PLANNING FLOWS FROM TEST RESULTS IN AN ELDERLY CLIENT WITH FREQUENT FALLS
| Patient profile: 72-year-old woman | |||
| Diagnosis: Disequilibrium of aging, frequent falls | |||
| Course of examination and treatment: Cardiologist → neurologist → outpatient physical therapy | |||
| TEST | PROBLEMS IDENTIFIED | GOALS SET | TREATMENT PLAN |
| Peripheral sensory | Mildly decreased vibration sense bilateral lower extremity | Compensate for permanent sensory loss | Educate about safe surfaces and lighting |
| Somatosensory | Home safety evaluation | ||
| Vision | ↓ Acuity, cataracts | ||
| ↓ Depth perception | |||
| SOT | Absent use of vestibular inputs 0/100Decreased use of somatosensory inputs 60/100 Dependent on vision |
Increase use of vestibular inputs to 30/100Increase use of somatosensory inputs to 75/100 | Somatosensory and vestibular stimulation* |
| Static postural sway | Excessive sway—2 standard deviations outside normal range for age | Standing sway within normal limits for age | COG control training |
| Nudge or push test | No use of ankle or hip strategySteps immediately | Survives 5/10 pushes with hip strategy | Hip strategy exercises* |
| LOS | No ankle strategy—uses hip strategySway to 45% LOS anterior, 35% LOS posterior Slow movement time |
Uses ankle strategy to reach 40% LOS anterior and posteriorReaches 8/8 targets at 75% LOS using hip or ankle strategy within 4 s |
COG control training |
| ROM | ↓ Neck extension 0-10 degrees↓ Lumbar extension 1-15 degrees ↓ Hip extension 0-5 degrees |
↑ Spinal extension neck 0-20 degrees↑ Lumbar extension 0-20 degrees ↑ Hip extension 0-10 degrees |
ROM exercises* |
| Strength | Flexion 4/5(B) Hip abduction 3+/5, extension 3/5 (B) Knee extension 4+/5, flexion 4/5 (R) Ankle dorsiflexion 3−/5 (L) Ankle dorsiflexion 2/5 (B) Ankle plantarflexion 3+/5 |
↑(B) Hip abduction and extension to greater than 4/5↑ (B) Ankle dorsiflexion and plantarflexion to 4−/5 | Progressive resistive exercises, including bicycle* |
| Gait (GARS) | Score 35/48Deviations Forward flexed trunk Double limb stance prolonged bilaterally Short step length |
GARS scales 25/48(I) Ambulation with walker in home, community | Gait training*1—starts, stops, turns 2—treadmill 3—uneven surfaces, curbs, stairs, carpet, outdoors |
| Endurance | Fatigue after ambulating 60 ft | Ambulates more than 200 ft without stopping | Gait training as earlier |
| Tinetti balance scale | 6/16 score | Tinetti balance score 10/16 | Gait training as earlier |
| Tinetti gait scale | 5/12 scoreFalls and catches self | Tinetti gait score 8/12 | Gait training as earlier |
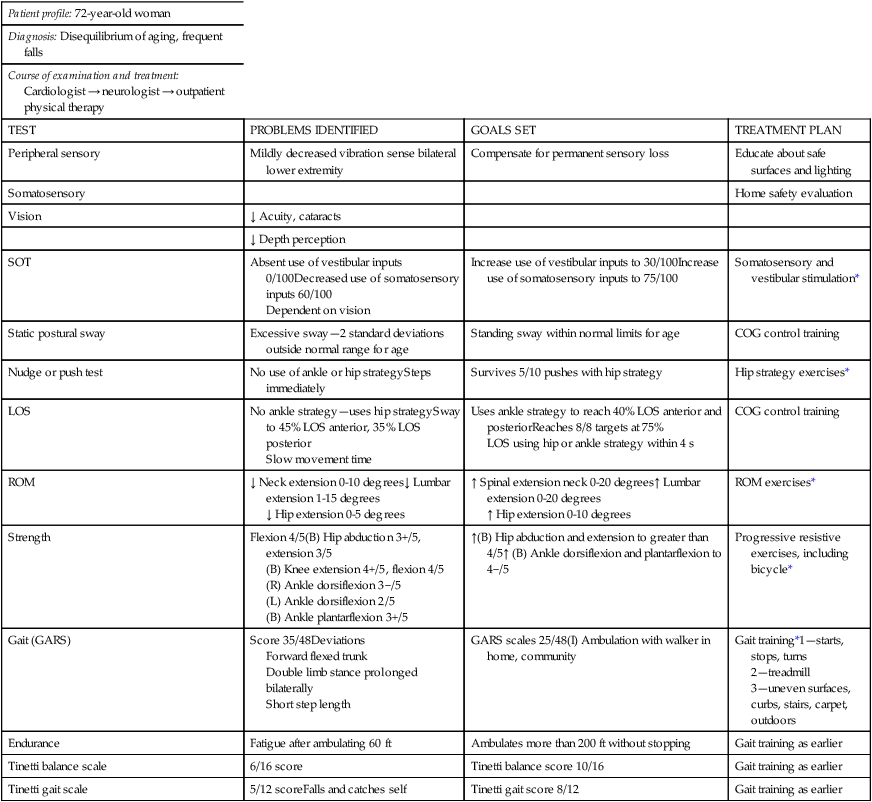
*Also included in home exercise program.
Reprinted with permission from NeuroCom International, Clackamas, Ore.
TABLE 22-7 
AN EXAMPLE OF HOW TREATMENT PLANNING FLOWS FROM TEST RESULTS IN A CLIENT WITH RIGHT HEMIPARESIS
| Patient profile: 69-year-old woman | |||
| Diagnosis: Left cerebrovascular accident with right hemiparesis | |||
| Course of examination and treatment: Acute rehabilitation → home health → outpatient rehabilitation | |||
| TEST | PROBLEMS IDENTIFIED | GOALS SET | TREATMENT PLAN |
| Peripheral somatosensory | None | ||
| SOT | Average overall stability 47/100Absent use of vestibular inputs 0/100 | Average stability 60/100) Use of vestibular inputs 15/100 | Vestibular stimulation with forced use and head movements |
| Postural sway | COG control training | ||
| Functional reach | Forward lean restricted to 5 inches | Able to reach forward 8 inches | |
| Static balance | Weight shift asymmetry to left in static standing and medial or lateral sway, 25% LOS to left of midline | ↑ Control of COGStands midline | |
| Limit of stability | Forward weight shift restricted to 25% LOS | ↑ Forward LOS to 50% ) Right LOS to 50% |
|
| Rhythmic weight shift | Extraneous sway off desired path | ↓ Extraneous sway scores by 50% | |
| OLST | Unable on right leg, 30 seconds on left leg | Stands on right leg, 10 seconds | COG control training |
| Nudge, push (motor strategy selection) | Switch from ankle to hip strategy noted but unable to withstand perturbation | Able to stand upright after mild perturbations 5/10 timesAble to “catch” self by stepping or reaching 5/10 times | Hip and stepping strategy training |
| Range of motion | None | ||
| Strength: right leg | 4/5 Knee extension3/5 Knee flexion 2/5 Ankle dorsiflexion 3/5 Ankle plantarflexion |
↑ RLE strength5/5 Knee 4/5 Ankle |
Progressive resistive exercises |
| Endurance | Standing tolerance less than 10 minutes | Able to stand unaided for 15 minutes | Standing tolerance tasks |
| Gait | ↓ Step length—RLE↓ Step height—RLE ↓ Heel strike—RLE ↓ Toe-off—RLE |
Symmetrical step height and length 5/10 times) Heel strike RLE 5/10 times | Gait training on treadmill |
| Tinetti Gait Subscale | Unable to turn, reach, or bend without loss of balanceFalls: Uneven surfaces Low lighting Head turning No community ambulation Requires cane Requires supervision for household ambulation |
8/12 scoreNo falls Gait independent without cane in household; with cane in community |
Gait training on uneven surfaces, with head movements, with low lightingSafety education |
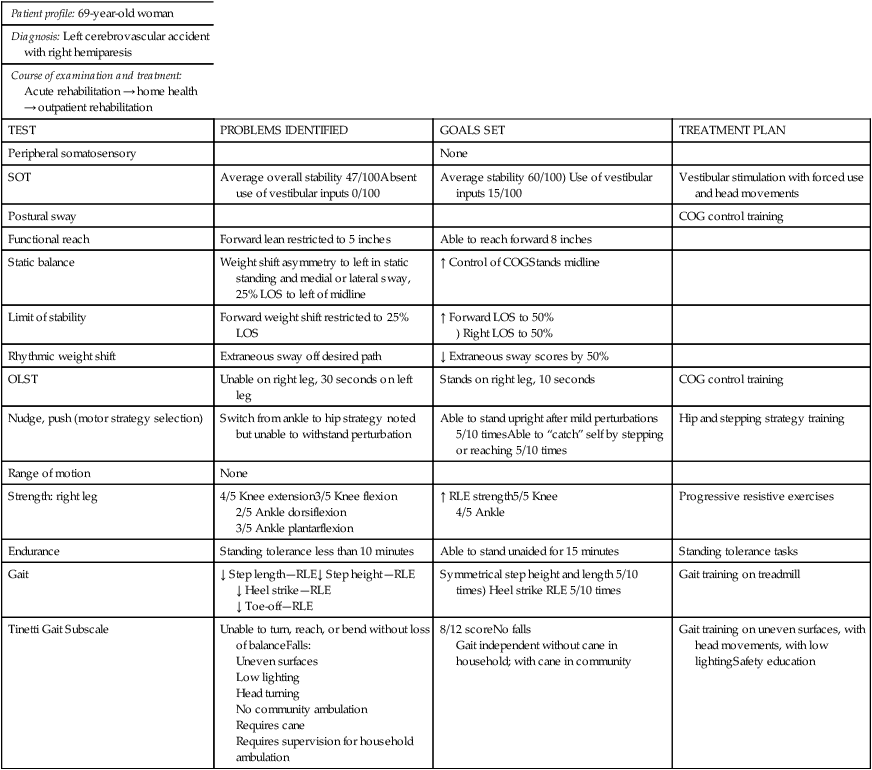
Reprinted with permission from NeuroCom International, Clackamas, Ore.