Extremely aggressive and almost always unresectable
• Pancreatoblastoma

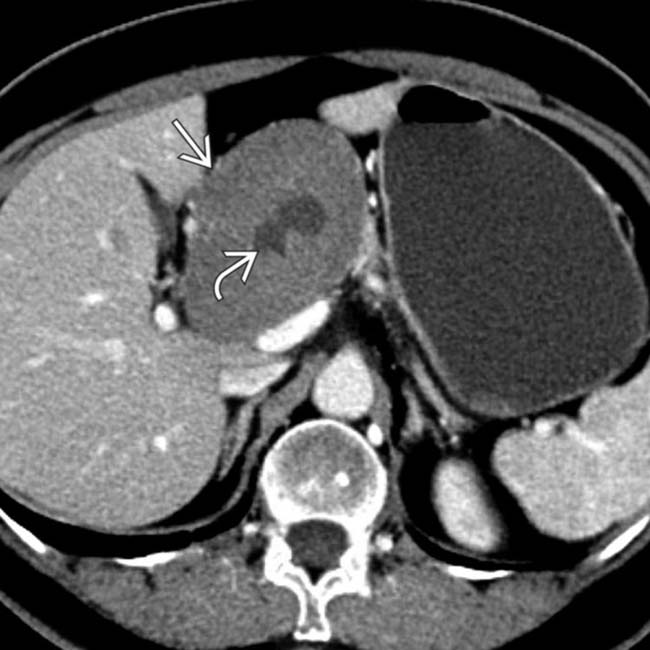
 in the pancreatic head with solid and cystic components. This was found to be an acinar cell carcinoma at surgery. As in this case, these tumors often mimic the appearance of neuroendocrine tumors, albeit with less hyperenhancement.
in the pancreatic head with solid and cystic components. This was found to be an acinar cell carcinoma at surgery. As in this case, these tumors often mimic the appearance of neuroendocrine tumors, albeit with less hyperenhancement.
 arising from the pancreatic tail. This mass was found to be an acinar cell carcinoma at surgery.
arising from the pancreatic tail. This mass was found to be an acinar cell carcinoma at surgery.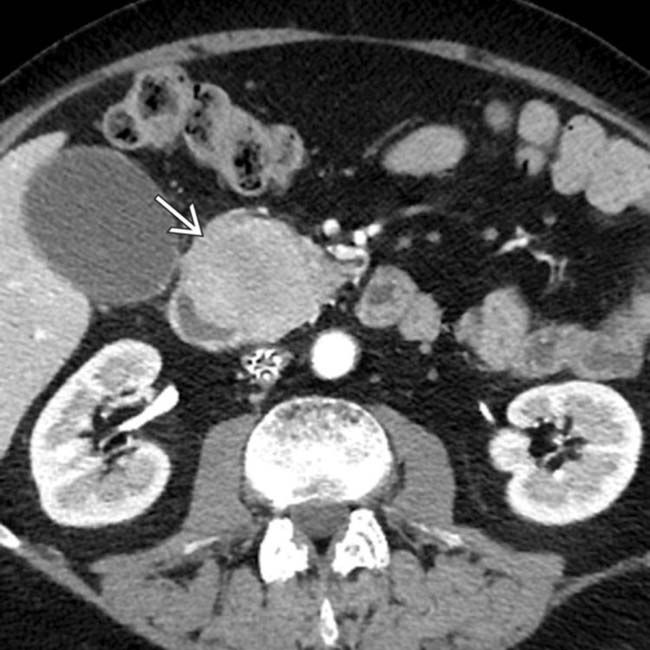
 in the pancreatic head.
in the pancreatic head.
IMAGING
General Features
• Giant cell carcinoma (pleomorphic or osteoclast)
• Acinar cell carcinoma
• Pancreatoblastoma
CLINICAL ISSUES
Presentation
Natural History & Prognosis
• Anaplastic carcinoma
• Small cell carcinoma
 with internal cystic foci
with internal cystic foci  that was found to be a benign pancreatic schwannoma at resection.
that was found to be a benign pancreatic schwannoma at resection.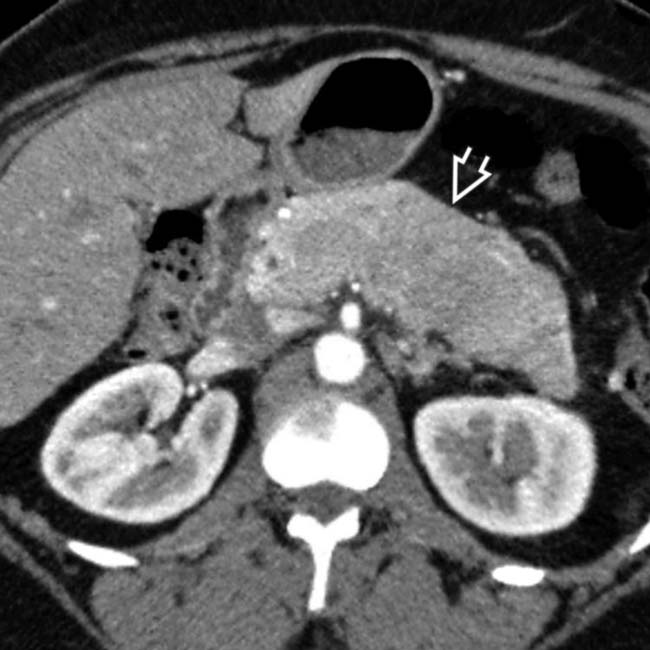
 in the pancreatic body and tail. While the appearance suggests adenocarcinoma, this is a rare pancreatoblastoma in an adult patient, a tumor much more common in children.
in the pancreatic body and tail. While the appearance suggests adenocarcinoma, this is a rare pancreatoblastoma in an adult patient, a tumor much more common in children.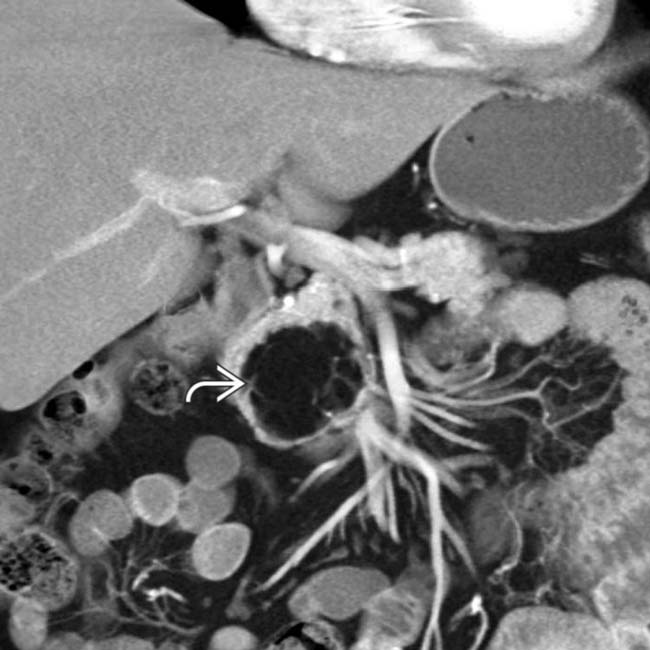
 within the pancreatic head. The mass is quite simple in appearance, with only a few linear strands interspersed in the midst of fat density.
within the pancreatic head. The mass is quite simple in appearance, with only a few linear strands interspersed in the midst of fat density.
 in the neck of the pancreas. Note that the mass is homogeneously enhancing and conforms to the contours of adjacent structures. There is no biliary obstruction. However, multiple liver metastases
in the neck of the pancreas. Note that the mass is homogeneously enhancing and conforms to the contours of adjacent structures. There is no biliary obstruction. However, multiple liver metastases  are noted.
are noted.
 involving the body of the pancreas with central necrosis
involving the body of the pancreas with central necrosis  . Note the obstruction of the common duct
. Note the obstruction of the common duct  , which contains a metallic stent.
, which contains a metallic stent.
 arising from the pancreatic tail with moderate vascularity and central necrosis
arising from the pancreatic tail with moderate vascularity and central necrosis  . Note the invasion of the left kidney
. Note the invasion of the left kidney  by the mass.
by the mass.
 arising from the tail of the pancreas. Note the focal calcification in one of the septations
arising from the tail of the pancreas. Note the focal calcification in one of the septations  .
.
 in the body of the pancreas that contains both solid
in the body of the pancreas that contains both solid  and cystic
and cystic  elements. At pathology, this lesion was proven to be a rare giant cell carcinoma.
elements. At pathology, this lesion was proven to be a rare giant cell carcinoma.
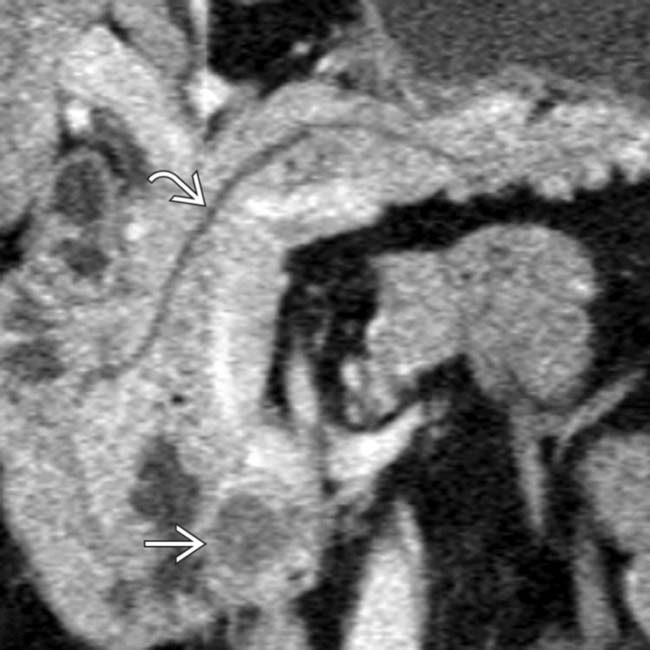
 arising from the pancreatic tail and invading the spleen. The appearance would be more typical for an aggressive neuroendocrine tumor, but the mass was found at biopsy to be an acinar cell carcinoma.
arising from the pancreatic tail and invading the spleen. The appearance would be more typical for an aggressive neuroendocrine tumor, but the mass was found at biopsy to be an acinar cell carcinoma.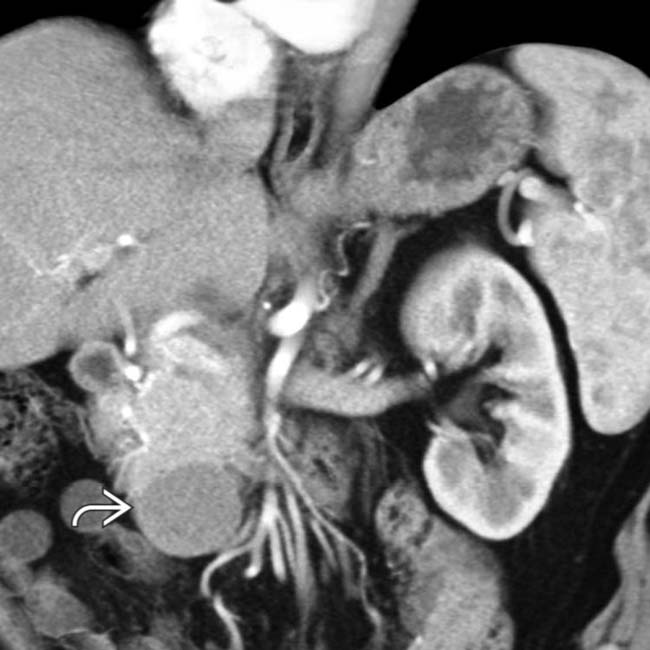
 arising exophytically from the pancreatic head, found to represent a rare acinar cell carcinoma.
arising exophytically from the pancreatic head, found to represent a rare acinar cell carcinoma.
 that follows the course of the splenic vein along the dorsal surface of the pancreas. There is no evidence of local invasion, metastases, or ductal obstruction. This was found to be a plexiform neurofibroma.
that follows the course of the splenic vein along the dorsal surface of the pancreas. There is no evidence of local invasion, metastases, or ductal obstruction. This was found to be a plexiform neurofibroma.














































































 in the head of the pancreas. The mass does not obstruct the pancreatic duct
in the head of the pancreas. The mass does not obstruct the pancreatic duct  and was found to be benign peripancreatic schwannoma.
and was found to be benign peripancreatic schwannoma.


