48 Asthma
• Asthma is a chronic inflammatory condition that can be controlled.
• Indications of inadequate control of asthma include frequent use of short-acting β-agonist agents, wheezing, coughing, and nighttime symptoms.
• Emergency department treatment of asthma exacerbation includes a targeted history and physical examination, aerosolized β-agonist agents, and systemic steroids with objective measures of response to therapy. Anticholinergic agents should be used in the emergency department for patients with a severe exacerbation.
• At discharge, controller medications should be prescribed in addition to rescue medications for patients with chronic persistent asthma. Patients should follow up with a primary care physician or asthma specialist within several weeks.
Perspective
Asthma is a chronic inflammatory disorder characterized by increased responsiveness of the airways to multiple stimuli. Many cells and cellular elements, such as mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells, play a role in development of the inflammatory response.1 The inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are associated with airflow obstruction that is reversible either spontaneously or with treatment. Although patients appear to clinically recover completely, evidence suggests that some asthmatic patients have chronic airflow limitation. The recognition that asthma is a chronic inflammatory disorder of the airways has significant implications for the diagnosis, management, and potential prevention of acute exacerbations.
Epidemiology
Asthma affects approximately 4% to 5% of the population in the United States.2 Although it is the most common chronic disease of childhood, with a prevalence of 5% to 10%, it also affects 7% to 10% of the elderly. Epidemiologic studies suggest that asthma is underdiagnosed and undertreated in all age groups. Part of the problem is that the transient nature of asthma allows many patients to tolerate intermittent respiratory symptoms before seeking medical care. Another important factor resulting in underdiagnosis of asthma is the sometimes nonspecific nature of the symptoms.
About half of cases of asthma develop before 10 years of age and another third before 40 years. The 2 : 1 male-to-female preponderance of asthma in childhood equalizes by 30 years of age.3 The average asthmatic patient has 15 days of restricted activity each year and spends 5.8 days in bed. Approximately 2 million emergency department (ED) visits, 484,000 hospitalizations, and more than 4000 deaths per year are attributed to asthma. In the United States alone, the estimated direct and indirect cost of asthma in all age groups was $56 billion in 2007.4
Pathophysiology
Allergic asthma occurs when inhaled allergens bind to immunoglobulin E molecules bound to mast cells in the lining of the tracheobronchial tree. During the early response, various mediators are released and cause greater vascular permeability, mucosal edema, and contraction of bronchial smooth muscle. A second wave of reaction, the late response, is seen hours to days later; it involves accumulation of inflammatory cells in the bronchial mucosa, thus perpetuating the reaction. The release of mediators and regulation of the inflammatory process in asthma are complex, redundant, and self-perpetuating.5
Although several theories attempt to explain the pathophysiologic changes that occur in nonallergic asthma, none adequately explain all clinically observed phenomena. Research suggests that even patients without atopy have pathophysiology similar to that in atopic patients.5 Respiratory infections, particularly viral infections, may precipitate bronchospasm. Viruses cause mucosal inflammation and lower the firing threshold of the subendothelial vagal receptors, which results in enhanced airway reactivity that may last up to 8 weeks, even in nonasthmatic persons. Pharmacologic agents, such as aspirin and nonsteroidal antiinflammatory compounds, coloring agents, and beta-blockers, also induce acute asthma. In addition, sulfating agents, which are used widely as food preservatives and antioxidants in pharmaceutical products, can exacerbate asthma.
Most patients with asthma seem to display an exaggerated bronchoconstrictive response to a variety of exogenous and endogenous stimuli, and inflammation plays a key role. The final common pathway is as follows1:
Presenting Signs and Symptoms
Diagnostic Testing
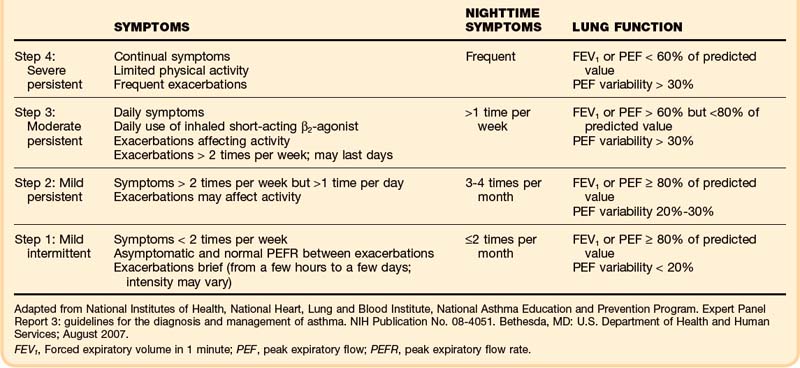
As for all patients who come to the ED for care, a directed history and physical examination should be performed. Key historical points should be elicited, such as the duration and onset of the current attack, identification of precipitating causes, type and amount of medications used before arrival at the ED, response to previous therapy, including current or previous use of corticosteroids, frequency of ED visits and hospitalizations, previous need for intubation or ventilation, history of concurrent medications and allergies, and history of concurrent medical problems. At some point during the patient’s ED stay, effort should be made to evaluate both the severity of the obstruction and the adequacy of ongoing asthma control (Table 48.1).
The physical examination should focus on observing respiratory effort and use of accessory muscles and listening for wheezing or other abnormal breath sounds and prolongation of the expiratory phase. Although wheezing results from movement of air through narrowed airways, the intensity of the wheeze may not correlate with the severity of airflow obstruction. Tachycardia and tachypnea are usually present in patients with acute asthma, but vital signs normalize very quickly as the airflow obstruction is relieved.10 Therefore, a normal heart rate and respiratory rate are not reliable indicators of the degree of relief from obstruction.
Bedside spirometry provides a rapid, objective assessment of patients and helps both indicate the effectiveness of and guide therapy. Sequential measurements assist emergency physicians in assessing the severity of the problem and determining the response to therapy. Although forced expiratory volume in 1 second (FEV1) and the peak expiratory flow (PEF) rate measure the extent of large airway obstruction, patient cooperation is essential for these tests to be reliable. When possible, management decisions should be guided by a patient’s personal best PEF rate or FEV1 value or, if unknown, a percentage of the predicted value in addition to other physiologic and historical factors.1
Pulse oximetry is a useful and convenient method for accessing oxygenation and monitoring oxygen saturation during treatment. Analysis of arterial blood gases is not indicated in the majority of patients with mild to moderate asthma exacerbation, but it is helpful if there is concern for hypoventilation with carbon dioxide retention and respiratory acidosis. Patients with the latter problems almost always have clinical evidence of severe attacks or spirometry demonstrating PEF or FEV1 less than 25% of the predicted value.11,12 Practitioners should be aware that a normal or slightly elevated PaCO2 (e.g., 42 mm Hg or higher) indicates extreme airway obstruction and fatigue and may herald the onset of acute ventilatory failure.11,12
Routine radiography is unnecessary but is indicated if the possibility of pneumothorax, pneumomediastinum, pneumonia, or other medical conditions is a concern. In up to one third of asthmatic patients requiring admission, an abnormality is demonstrated on chest radiographs.13
Use of exhaled nitric oxide measurements and other serum and urine markers for detection of the severity of the asthma exacerbation is currently under investigation.14–17
Treatment
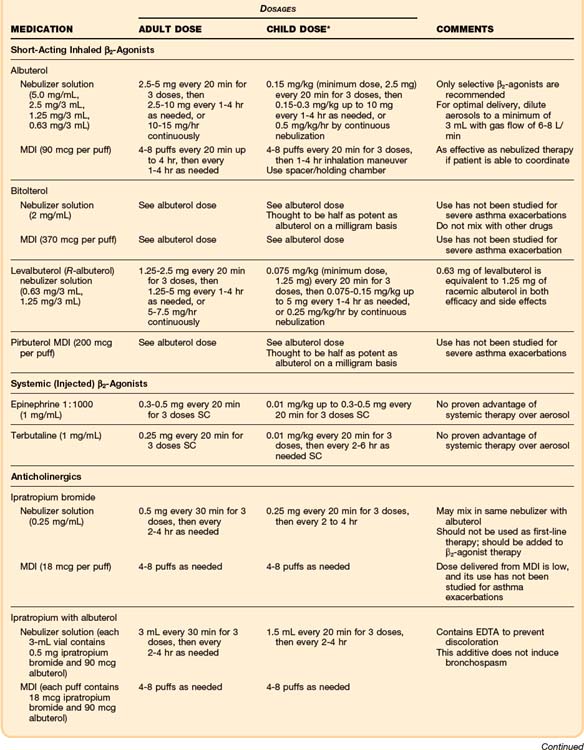
The goal of treatment of acute asthma in the ED is to rapidly reverse the airflow obstruction with repetitive or continuous administration of inhaled β2-agonists, ensure adequate oxygenation, and relieve inflammation. The National Asthma Education and Prevention Program Expert Panel has developed guidelines for emergency treatment of asthma (Fig. 48.1),1 as have other organizations around the world. Prehospital treatment with oxygen and β2-agonists is usually initiated. The following types of medications have been shown to be effective for the treatment of acute asthma: β2-agonists, anticholinergics, and glucocorticoids (Table 48.2).1 Magnesium should be considered in patients with severe obstruction. Current evidence does not support the use of heliox (helium-oxygen mixture) or ketamine, even when the aforementioned medications fail to relieve bronchospasm. Mast cell–stabilizing agents, methylxanthines, and leukotriene modifiers are currently reserved for maintenance therapy only.
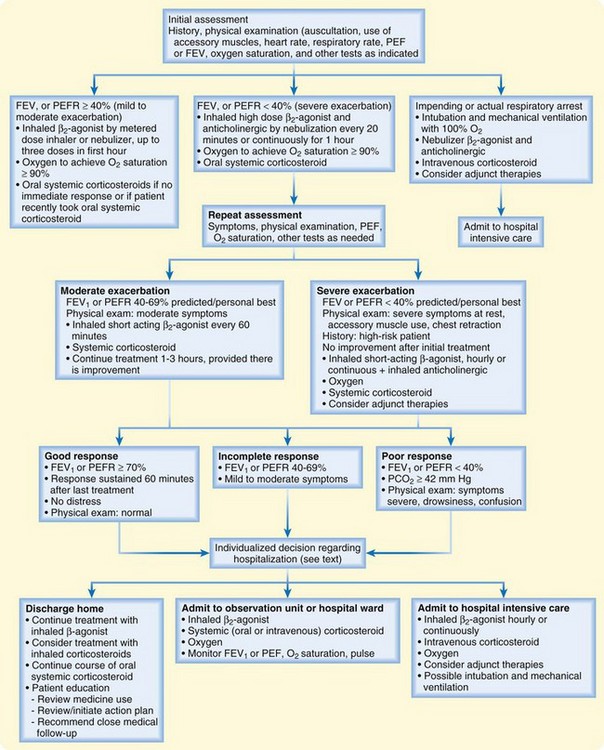
Fig. 48.1 Management of asthma exacerbations: emergency department– and hospital-based care.
(Adapted from National Institutes of Health, National Heart, Lung and Blood Institute, National Asthma Education and Prevention Program. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. NIH Publication No. 08-4051. Bethesda, MD: U.S. Department of Health and Human Services; August 2007.)
Pharmaceuticals
β2-Agonist Agents
β2-Agonists are the preferred initial rescue medications for acute bronchospasm. In addition to bronchodilation, these drugs inhibit the release of mediators and promote mucociliary clearance.1
Aerosol therapy with β2-agonist drugs produces excellent bronchodilation with minimal systemic absorption and few side effects. Aerosol delivery may be achieved with a metered dose inhaler (MDI) with a spacing device or a compressor-driven nebulizer.19 A spacing device attached to the inhaler can improve drug deposition when patient technique is inadequate. Even with optimal technique only a maximum of 15% of the dose of the drug is retained in the lungs, regardless of the aerosol method used. Since 2008, dry-powder delivery devices and MDIs using hydrofluoroalkane as propellant have replaced chlorinated fluorocarbon–driven devices. Aerosol treatments may be administered every 15 to 20 minutes or on a continuous basis.20 Subcutaneous administration of terbutaline or epinephrine may be used in patients unable to coordinate aerosolized or MDI treatments or to tolerate aerosolized medications.21
Intravenous β2-agonist infusions offer no advantage over aerosolized or MDI-delivered agents and carry potential risk.22
Salmeterol xinafoate is indicated only as maintenance therapy, should never be used more frequently than twice per day, and is to be avoided for the treatment of acute exacerbations.1
Corticosteroids
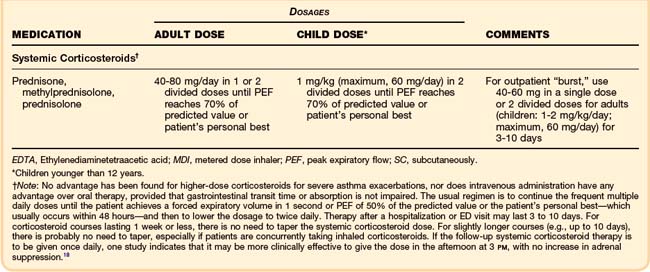
Corticosteroids, highly effective drugs for asthma exacerbation, are a cornerstone of treatment.23 They are thought to produce beneficial effects by restoring β2-agonist responsiveness and reducing inflammation. Onset of the antiinflammatory effects of corticosteroids is delayed at least 4 to 8 hours after intravenous or oral administration.
Data indicate that corticosteroids, administered within 1 hour of arrival in the ED, reduce the need for hospitalization of a patient with an asthma exacerbation.23 Although evidence for what constitutes the optimal dose for acute asthma is lacking, experts agree that an initial 40- to 60-mg dose of prednisone or an intravenous 60- to 125-mg bolus of methylprednisolone in patients unable to tolerate oral medications is usually adequate. No advantage has been demonstrated for higher doses.24 Additional doses should be given every 4 to 6 hours until significant subjective and objective improvement is achieved. Patients who are being discharged home after ED treatment should be prescribed a 3- to 10-day nontapering “burst” of oral steroids, such as prednisone, 40 to 60 mg/day, or its equivalent.
Current recommendations favor inhaled corticosteroids for maintenance of all patients with mild persistent asthma or more severe asthma.1 Therefore, consideration should be given to discharging any patient with mild persistent or more severe asthma with maintenance inhaled corticosteroid therapy in addition to the burst of oral steroids.25
Anticholinergics
Aerosolized ipratropium bromide, 0.5 mg, should be administered to patients with a severe exacerbation of asthma. Ipratropium is a synthetic quaternary derivative that is available as both a nebulized solution and in an MDI (18 mg per puff) and is well tolerated (see Table 48.2). Clinical trials indicate that adding ipratropium to β2-agonist agents offers mild additional improvement in bronchodilation and significantly decreases the need for hospitalization.26 Side effects include dry mouth, thirst, and difficulty swallowing. Less commonly, tachycardia, restlessness, irritability, confusion, difficulty in micturition, ileus, blurring of vision, and an increase in intraocular pressure are noted.
At discharge, addition of tiotropium to the patient’s current inhaled corticosteroid dose is comparable to the addition of salmeterol—both are more effective in achieving disease control than is doubling the inhaled corticosteroid dose.27
Magnesium
Intravenous magnesium sulfate is indicated for the management of acute, very severe asthma, such as a patient with an FEV1 less than 25% of predicted, but not in those with mild or moderate asthma exacerbation.28–30 The dose is 1 to 2 g intravenously delivered over a 30-minute period. Inhaled magnesium may also be a helpful adjunct in the treatment of a severe exacerbation.31,32 Magnesium is not a substitute for standard therapy regimens.
Heliox, Ketamine, and Halothane
Helium is not indicated for use in patients with mild or moderate asthma exacerbation, although several studies have demonstrated its effectiveness for very severe asthma.33 Several investigators have reported success with ketamine34,35 and halothane in patients in whom all other treatment modalities have failed. Controlled trials substantiating these claims are lacking.
Leukotriene Modifiers
Leukotriene modifiers improve lung function, diminish symptoms, and reduce the need for short-acting β2-agonists.1 They are recommended as an alternative to low-dose inhaled corticosteroid therapy in patients with mild persistent asthma and as steroid-sparing agents with inhaled corticosteroids in those with moderate persistent asthma. Several leukotriene modifiers—montelukast, zafirlukast, and zileuton—are currently available as oral tablets for the treatment of asthma. Although intravenous montelukast has been demonstrated to cause rapid bronchodilation when used as adjuvant therapy for acute asthma in a single trial, recommending its use for the treatment of acute bronchospasm in the ED would be premature.36 Montelukast, zafirlukast, and zileuton have been associated with neuropsychiatric side effects.
Theophylline
Although theophylline is no longer considered a first-line treatment of acute asthma,37 some patients who come to the ED for treatment may be using it at home. Some data suggest that this agent has an antiinflammatory mechanism of action. When used in combination with inhaled β2-agonists, theophylline appears to increase the toxicity—but not the efficacy—of treatment. The most common side effects of theophylline are nervousness, nausea, vomiting, anorexia, and headache. At plasma theophylline levels greater than 30 mcg/mL, there is a risk for seizures and cardiac arrhythmias.
Mechanical Ventilation
When it appears that a patient needs more than the aforementioned treatments, noninvasive positive pressure ventilation may be attempted. Data showing that bilevel positive airway pressure reduces the need for intubation and mechanical ventilation are lacking.38–40
The potential complications of mechanical ventilation in asthmatic patients are numerous: barotrauma, hemodynamic impairment, mucous plugging leading to increased airway resistance, atelectasis, and pulmonary infection. Air trapping and increased residual volume (intrinsic positive end-expiratory pressure) may be partially avoided with controlled mechanical hypoventilation or permissive hypoventilation.39,40 This form of mechanical ventilation is achieved by using a reduced respiratory rate and low inspiratory volume and pressure and allowing adequate time for the expiratory phase. One can achieve the goal of ventilatory support—maintenance of adequate arterial oxygen saturation (90% or greater)—without concern about “normalizing” the hypercapnic acidosis. All patients requiring mechanical ventilation should be admitted to an intensive care unit.
Disposition
• Does the patient feel that the wheezing and air exchange have improved?
• Does auscultation confirm improvement or lack thereof?
• Has a significant improvement in FEV1 or PEF been noted?
• What is the patient’s health care history?
• Is the patient usually compliant with care plans and medication regimens?
• Does the patient have access to prompt follow-up?
• Does the patient usually require hospitalization after an exacerbation?
Unfortunately, a formula for successful discharge without risk for early relapse does not yet exist, and up to 25% of patients treated in the ED for asthma return within 3 weeks.41–44
Addition of a short, nontapering course of oral steroids to the scheduled use of a β2-agonist bronchodilator reduces relapse rates in discharged patients. Patients with chronic asthma who are not using controller medications at home should be prescribed and educated about the daily use of either inhaled corticosteroids or leukotriene modifiers, in addition to their rescue medications.45 Data indicate that relying on the primary care physician to prescribe these controllers at follow-up is inadequate.25
Current guidelines suggest that patients with a good response to treatment, as demonstrated by complete resolution of symptoms and a PEF or FEV1 value greater than 70% of predicted, can be safely discharged home. Patients with a poor response to treatment, as defined by persistent symptoms, a PEF or FEV1 value less than 50% of predicted, and persistent wheezing and dyspnea at rest, should be admitted. Many patients with an incomplete response to treatment, as defined by some persistence of symptoms and a PEF or FEV1 value between 50% and 70% of predicted, may be discharged home safely, provided that they have no risk factors for death from asthma.1 Patients who do not show adequate improvement over several hours because they are in the late phase of the exacerbation and those with significant risk factors for death from asthma should be admitted to either an observation unit or the hospital. Most patients have an incomplete response to treatment and fall into this “gray zone” of disposition decisions.
Studies indicate that the majority of asthmatic patients admitted to an observation unit where strict care protocols are followed can be successfully treated and discharged.45
National Institutes of Health, National Heart, Lung and Blood Institute, National Asthma Education and Prevention Program. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. NIH Publication No. 08–4051. Bethesda, MD: U.S. Department of Health and Human Services; August 2007.
Rodrigo GJ, Castro-Rodriguez JA. Anticholinergics in the treatment of children and adults with acute asthma: a systematic review with meta-analysis. Thorax. 2005;60:740–746.
Rowe BH, Spooner C, Ducharme FM, et al. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 1, 2001. CD002178
Rowe BH, Spooner CH, Ducharme FM, et al. Corticosteroids for preventing relapse following acute exacerbations of asthma (Cochrane Review). In: The Cochrane Library. Oxford: Update Software; 2004.
1 National Institutes of Health, National Heart, Lung and Blood Institute, National Asthma Education and Prevention Program. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. NIH Publication No. 08–4051. Bethesda, MD: U.S. Department of Health and Human Services; August 2007.
2 National Center for Health Statistics. Health, United States. Hyattsville, MD: Public Health Service; 2000.
3 Moorman JE, Rudd RA, Johnson CA, et al. MMWR Surveillance Summaries. National Surveillance for Asthma—United States, 1980-2004. Centers for Disease Control and Prevention. Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5608.al.htm
4 Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011;127:145–152.
5 Bousquet J, Jeffery PK, Busse WW, et al. Asthma: from bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000;161:1720–1745.
6 Robin ED. Unexpected, unexplained sudden death in young asthmatic subjects. Chest. 1989;96:790–793.
7 Wasserfallen JB. Sudden asphyxic asthma: a distinct entity? Am Rev Respir Dis. 1990;142:108–111.
8 Brooks SM, Hammad Y, Richards I, et al. The spectrum of irritant-induced asthma: sudden and not-so-sudden onset and the role of allergy. Chest. 1998;113:42–49.
9 Barr RG, Woodruff PG, Clark S, et al. Sudden-onset asthma exacerbations: clinical features, response to therapy, and 2-week follow-up. Multicenter Airway Research Collaboration (MARC) investigators. Eur Respir J. 2000;15:266–273.
10 Carden DL, Nowak RM, Sarkar D, et al. Vital signs including pulsus paradoxus in the assessment of acute bronchial asthma. Ann Emerg Med. 1983;12:80–83.
11 Martin TG, Elenbaas RM, Pingleton SH. Use of peak expiratory flow rates to eliminate unnecessary arterial blood gases in acute asthma. Ann Emerg Med. 1982;11:70–73.
12 McFadden ER, Jr. Clinical physiologic correlates in asthma. J Allergy Clin Immunol. 1986;77:1–5.
13 White CS. Acute asthma: admission chest radiography in hospitalized adult patients. Chest. 1991;100:14–16.
14 Shome GP, Starnes JD, Shearer M, et al. Exhaled nitric oxide in asthma: variability, relation to asthma severity, and peripheral blood lymphocyte cytokine expression. J Asthma. 2006;43:95–99.
15 Redington AE. Modulation of nitric oxide pathways: therapeutic potential in asthma and chronic obstructive pulmonary disease. Eur J Pharmacol. 2006;533:263–276.
16 Taylor DR. Nitric oxide as a clinical guide for asthma management. J Allergy Clin Immunol. 2006;117:259–262.
17 Spergel JM, Fogg MI, Bokszczanin-Knosala A. Correlation of exhaled nitric oxide, spirometry and asthma symptoms. J Asthma. 2005;42:879–883.
18 Beam WR, Weiner DE, Martin RJ. Timing of prednisone and alterations of airways inflammation in nocturnal asthma. Am Rev Respir Dis. 1992;146:1524–1530.
19 Cates CJ, Rowe BH. Holding chambers versus nebulisers for beta-agonist treatment of acute asthma. Cochrane Database Syst Rev. 2, 2000. CD000052
20 Camargo C, Jr., Spooner C, Rowe B. Continuous versus intermittent beta-agonists in the treatment of acute asthma. Cochrane Database Syst Rev. 4, 2003. CD001115
21 Cydulka R, Davison R, Grammer L, et al. The use of epinephrine in the treatment of older adult asthmatics. Ann Emerg Med. 1988;17:322–326.
22 Travers A, Jones AP, Kelly K, et al. Intravenous beta2-agonists for acute asthma in the emergency department. Cochrane Database Syst Rev. 2, 2001. CD002988
23 Rowe BH, Spooner C, Ducharme FM, et al. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 1, 2001. CD002178
24 Emerman CL, Cydulka RK. A randomized comparison of 100-mg vs 500-mg dose of methylprednisolone in the treatment of acute asthma. Chest. 1995;107:1559–1563.
25 Cydulka RK, Tamayo-Sarver JH, Wolf C, et al. Inadequate follow-up controller medications among patients with asthma who visit the emergency department. Ann Emerg Med. 2005;46:316–322.
26 Rodrigo GJ, Castro-Rodriguez JA. Anticholinergics in the treatment of children and adults with acute asthma: a systematic review with meta-analysis. Thorax. 2005;60:740–746.
27 Peters SP, Kunselman SJ, Icitovic N, et al. for the National Heart, Lung, and Blood Institute Asthma Clinical Research Network. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med. 2010;363:1715–1726.
28 Rowe BH, Camargo CA, Jr. The use of magnesium sulfate in acute asthma: rapid uptake of evidence in North American emergency departments. J Allergy Clin Immunol. 2006;117:53–58.
29 Silverman RA, Osborn H, Runge J, et al. IV magnesium sulfate in the treatment of acute severe asthma: a multicenter randomized controlled trial. Chest. 2002;122:489–497.
30 Cheuk DK, Chau TC, Lee SL. A meta-analysis on intravenous magnesium sulphate for treating acute asthma. Arch Dis Child. 2005;90:74–77.
31 Kokturk N, Turktas H, Kara P, et al. A randomized clinical trial of magnesium sulphate as a vehicle for nebulized salbutamol in the treatment of moderate to severe asthma attacks. Pulm Pharmacol Ther. 2005;18:416–421.
32 Blitz M, Blitz S, Hughes R, et al. Aerosolized magnesium sulfate for acute asthma: a systematic review. Chest. 2005;128:337–344.
33 Rodrigo GJ, Rodrigo C, Pollack CV, et al. Use of helium-oxygen mixtures in the treatment of acute asthma: a systematic review. Chest. 2003;123:891–896.
34 Howton JC. Randomized, double-blind, placebo-controlled trial of intravenous ketamine in acute asthma. Ann Emerg Med. 1996;27:170–175.
35 Lau TT, Zed PJ. Does ketamine have a role in managing severe exacerbation of asthma in adults? Pharmacotherapy. 2001;21:1100–1106.
36 Camargo CA, Jr., Smithline HA, Malice MP, et al. A randomized controlled trial of intravenous montelukast in acute asthma. Am J Respir Crit Care Med. 2003;167:528–533.
37 Parameswaran K, Belda J, Rowe BH. Addition of intravenous aminophylline to beta2-agonists in adults with acute asthma. Cochrane Database Syst Rev. 4, 2000. CD002742
38 Soroksky A, Stav D, Shpirer I. A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest. 2003;123:1018–1025.
39 Oddo M, Feihl F, Schaller MD, et al. Management of mechanical ventilation in acute severe asthma: practical aspects. Intensive Care Med. 2006;32:501–510.
40 Austan F, Polise M. Management of respiratory failure with noninvasive positive pressure ventilation and heliox adjunct. Heart Lung. 2002;31:214–218.
41 Rowe BH, Spooner CH, Ducharme FM, et al. Corticosteroids for preventing relapse following acute exacerbations of asthma (Cochrane Review). In: The Cochrane Library. Oxford: Update Software; 2004.
42 Emerman CL, Cydulka RK, Crain EF, et al. Prospective multicenter study of relapse after treatment for acute asthma among children presenting to the emergency department. J Pediatr. 2001;138:318–324.
43 Emerman CL, Woodruff PG, Cydulka RK, et al. Prospective multicenter study of relapse following treatment for acute asthma among adults presenting to the emergency department. MARC investigators. Multicenter Asthma Research Collaboration. Chest. 1999;115:919–927.
44 Frey U. Predicting asthma control and exacerbations: chronic asthma as a complex dynamic model. Curr Opin Allergy Clin Immunol. 2007;7:223–230.
45 Rydman RJ, Isola ML, Roberts RR, et al. Emergency department observation unit versus hospital inpatient care for a chronic asthmatic population: a randomized trial of health status outcome and cost. Med Care. 1998;36:599–609.