Assessment of Gait
Walking is the simple act of falling forward and catching oneself. One foot is always in contact with the ground, and within a cycle, there are two periods of single-leg support and two periods of double-leg support. With running, there is a period of time during which neither foot is in contact with the ground, a period called “double float.”
Winter1 felt walking gait performs five main functions. First, it helps to support of the head, arms, and trunk by maintaining a semirigid lower limb. Second, it helps to maintain upright posture and balance. Third, it controls the foot to allow it to clear obstacles and enables gentle heel or toe landing through eccentric muscle action. Fourth, it generates mechanical energy by concentric muscle contraction to initiate, maintain, and, if desired, increase forward velocity. Finally, through eccentric action of the muscles, it provides shock absorption and stability and decreases forward velocity of the body.
The locomotion pattern tends to be variable and irregular until about the age of 7 years.2 Several functional tasks are involved in gait, including forward progression, which is executed in a stepping movement in a wide range of rapid and comfortable walking speeds. Second, the body must be balanced alternately on one limb and then the other; this is accompanied by repeated adjustments of limb length. Finally, there is support of the upright body.
Gait assessment or analysis takes a great deal of time, practice, and technical skill combined with standardization for the clinician to develop the necessary skills.3–5 Most gait analysis today is performed with force platforms to measure ground reaction forces, electromyography to measure muscle activity, and high-speed video motion analysis systems to measure movement. Discussion of these techniques, however, is beyond the scope of this book. This chapter gives only a brief overview of a complex task, assessment of normal and pathological gait; detailed assessment of gait is left to other authors.6–15 The various terms commonly used to describe gait, the normal pattern of gait, the assessment of gait, and common abnormal gaits are reviewed.
Definitions5–10
Gait Cycle
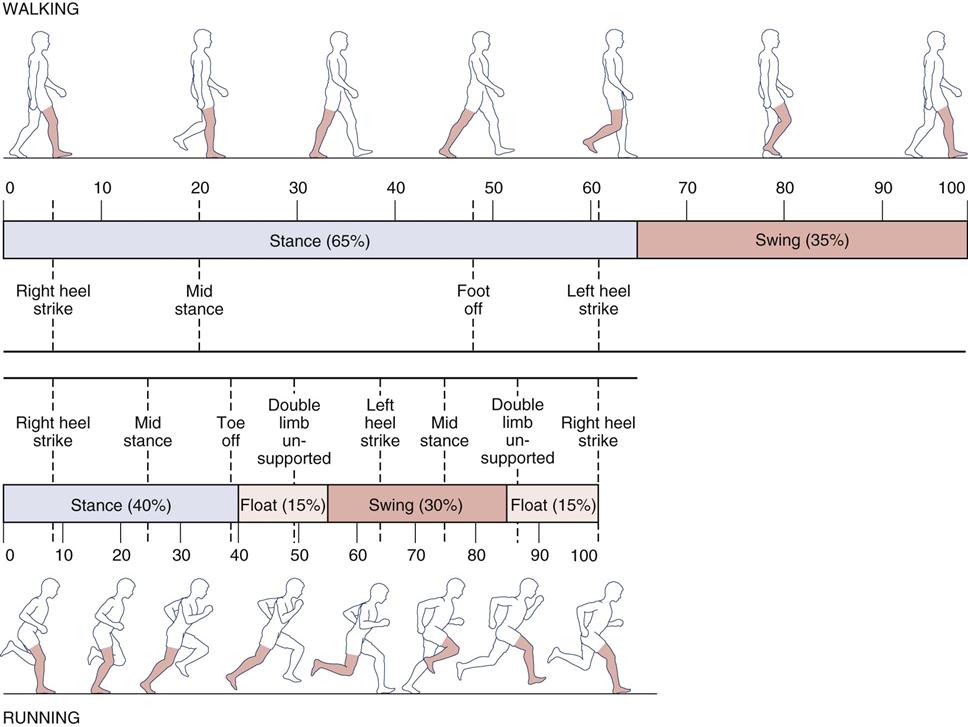
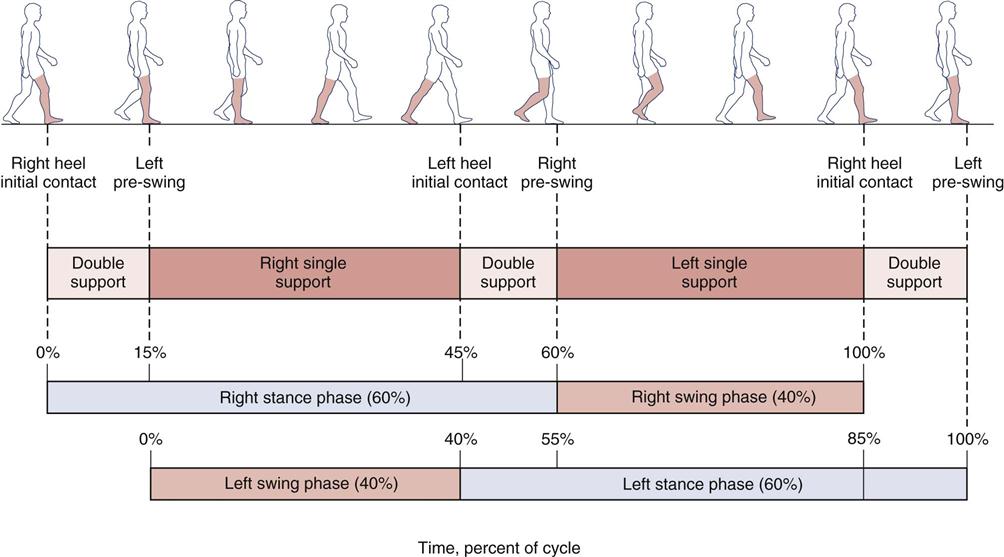
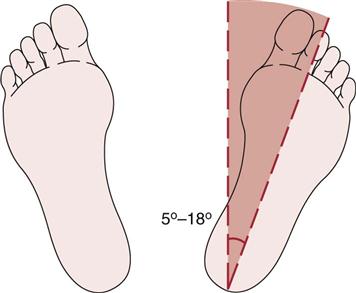
The gait cycle is the time interval or sequence of motions occurring between two consecutive initial contacts of the same foot (Figure 14-1). It is synonymous with the stride length. For example, if heel strike is the initial contact, the gait cycle for the right leg is from one heel strike to the next heel strike on the same foot. The gait cycle is a description of what happens in one leg. The same sequence of events is repeated with the other leg, but it is 180° out of phase.8 There are spatial descriptors of gait, such as stride length, step length and step width; time or temporal descriptors, such as cadence, stride time and step time; and, descriptors that involve time and space, such as walking speed.16 Another spatial descriptor that is sometimes discussed with gait is foot angle (Fick angle; see Figure 14-14). Each of these descriptors can and should be very similar for both limbs. For example, osteoarthritis in one hip can change many of the descriptors and the examiner should watch for these changes. Simoneau17 clearly described the terminology that applies to the gait cycle events (Figure 14-2). Table 14-1 demonstrates the periods or phases of the gait cycle, the function of each phase, and what is happening in the opposite limb.8 The gait cycle consists of two phases for each foot: stance phase, which makes up 60% to 65% of the walking cycle, and swing phase, which makes up 35% to 40% of the walking cycle. In addition, there are two periods of double support and one period of single-leg stance during the gait cycle.
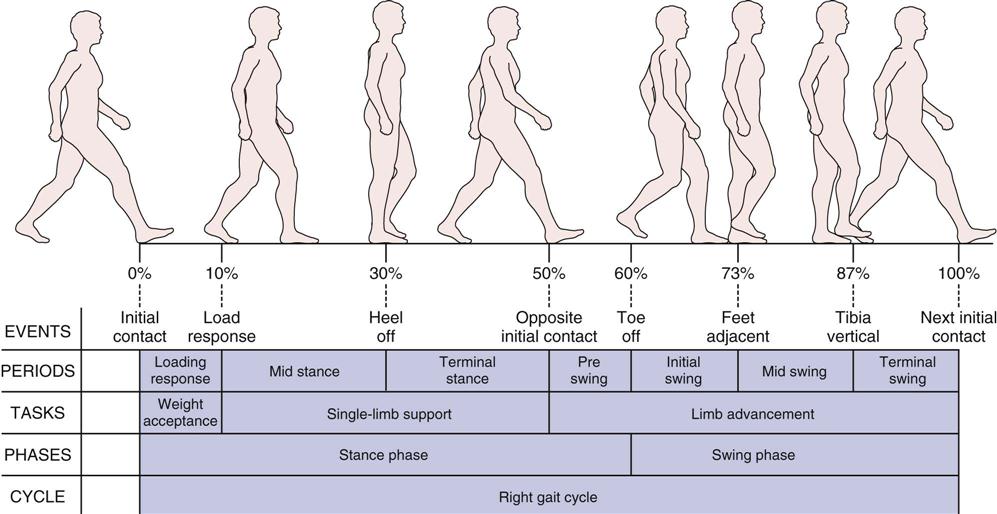
Initial contact corresponds to the beginning of stance when the foot first contacts the ground at 0% of gait cycle. Load response occurs when the contralateral foot leaves the ground at 10% of gait cycle. Heel off corresponds to the heel lifting from the ground and occurs at approximately 30% of gait cycle. Opposite initial contact corresponds to the foot contact of the opposite limb, typically at 50% of gait cycle. Toe off occurs when the foot leaves the ground at 60% of gait cycle. Feet adjacent takes place when the foot of the swing leg is next to the foot of the stance leg at 73% of gait cycle. Tibia vertical corresponds to the tibia of the swing leg being oriented in the vertical direction at 87% of gait cycle. The final event is, again, initial contact, which in fact is the start of the next gait cycle. These eight events divide the gait cycle into seven periods. Loading response, between initial contact and opposite toe off, corresponds to the time when the weight is accepted by the lower extremity, initiating contact with the ground. Midstance is from opposite toe off to heel rise (10% to 30% of gait cycle). Terminal stance begins when the heel rises and ends when the contralateral lower extremity touches the ground, from 30% to 50% of gait cycle. Preswing takes place from foot contact of the contralateral limb to toe off of the ipsilateral foot, which is the time corresponding to the second double-limb support period of the gait cycle (50% to 60% of gait cycle). Initial swing is from toe off to feet adjacent, when the foot of the swing leg is next to the foot of the stance leg (60% to 73% of gait cycle). Midswing is from feet adjacent to when the tibia of the swing leg is vertical (73% to 87% of gait cycle). Terminal swing is from a vertical position of the tibia to immediately before heel contact (87% to 100% of the gait cycle). The first 10% of the gait cycle corresponds to a task of weight acceptance—when body mass is transferred from one lower extremity to the other. Single-limb support, from 10% to 50% of the gait cycle, bears the weight of the body as the opposite limb swings forward. The last 10% of stance phase and the entire swing phase advance the limb forward to a new location. (Modified from Simoneau GG: Kinesiology of walking. In Neumann DA, editor: Kinesiology of the musculoskeletal system: foundations of physical rehabilitation, ed 2, St Louis, 2010, Mosby, p. 636.)
TABLE 14-1
Gait Cycle: Periods and Functions
| Period | Percentage of Cycle | Function | Contralateral Limb |
| Initial double limb support | 0 to 12 | Loading, weight transfer | Unloading and preparing for swing (preswing) |
| Single limb support | 12 to 50 | Support of entire body weight: center of mass moving forward | Swing |
| Second double limb support | 50 to 62 | Unloading and preparing for swing (preswing) | Loading, weight transfer |
| Initial swing | 62 to 75 | Foot clearance | Single limb support |
| Midswing | 75 to 85 | Limb advances in front of body | Single limb support |
| Terminal swing | 85 to 100 | Limb deceleration, preparation for weight transfer | Single limb support |
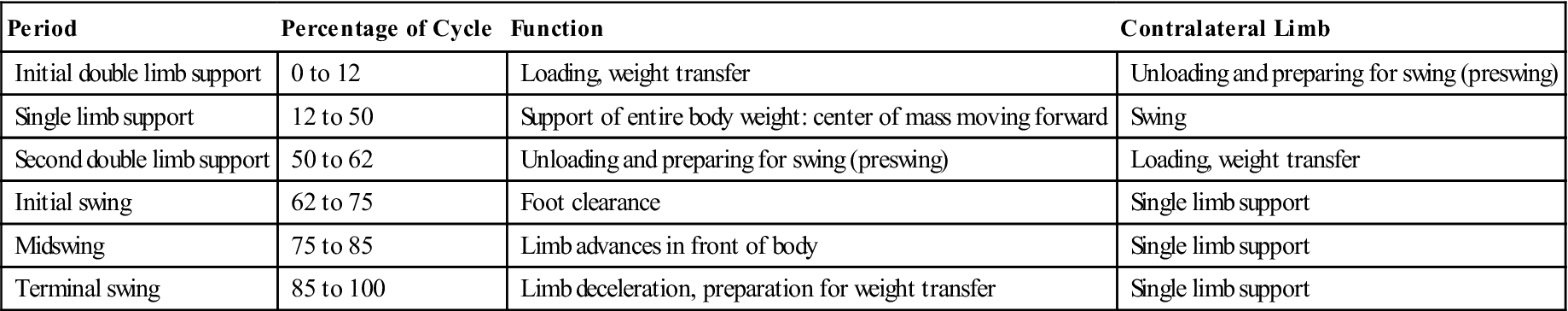
From Sutherland DH, et al: Kinematics of normal human walking. In Rose J, Gamble JG, editors: Human locomotion, Baltimore, 1994, Williams & Wilkins, p. 27.
As the velocity of the cycle increases, the cycle length or stride length decreases. For example, in jogging, the gait cycle is 70% of the walking cycle, and in running, the gait cycle is 60% that of walking.18 In addition, as the speed of movement increases, the function of the muscles changes somewhat, and their electromyographic activity may increase or decrease. Generally, gait velocity decreases with age.19 Montero-Odasso et al.20 found the gait velocity (less than 0.8 m/sec) could be used to determine mobility impairment in the elderly.
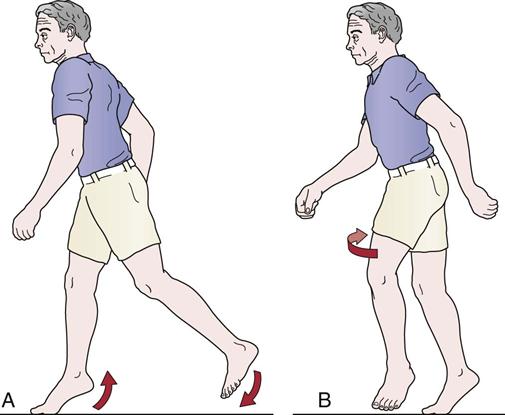
Stance Phase
The stance phase of gait occurs when the foot is on the ground and bearing weight (Figure 14-3). It allows the lower leg to support the weight of the body and, by so doing, acts as a shock absorber while allowing the body to advance over the supporting limb.18 Normally, this phase makes up 60% of the gait cycle and consists of five subphases, or instants.
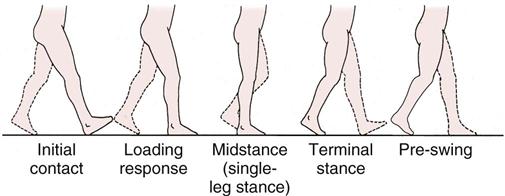
The initial contact instant is the weight-loading or weight acceptance period of the stance leg, which accounts for the first 10% of the gait cycle. During this period, one foot is coming off the floor while the other foot is accepting body weight and absorbing the shock of initial contact. Because both feet are in contact with the floor, it is a period of double support or double-leg stance.
The load response and midstance instants consist of the single support or single-leg stance, which accounts for the next 40% of the gait cycle. During this period, one leg alone carries the body weight while the other leg goes through its swing phase. The stance leg must be able to hold the weight of the body, and the body must be able to balance on the one leg. In addition, lateral hip stability must be exhibited to maintain balance, and the tibia of the stance leg must advance over the stationary foot.
The terminal stance and preswing instants make up the weight-unloading period, which accounts for the next 10% of the gait cycle. During this period, the stance leg is unloading the body weight to the contralateral limb and preparing the leg for the swing phase. As with the first two instants, both feet are in contact, and so double support occurs for the second time during the gait cycle.
Swing Phase
The swing phase of gait occurs when the foot is not bearing weight and is moving forward (Figure 14-4). The swing phase allows the toes of the swing leg to clear the floor and allows for leg length adjustments. In addition, it allows the swing leg to advance forward. It makes up approximately 40% of the gait cycle and consists of three subphases.
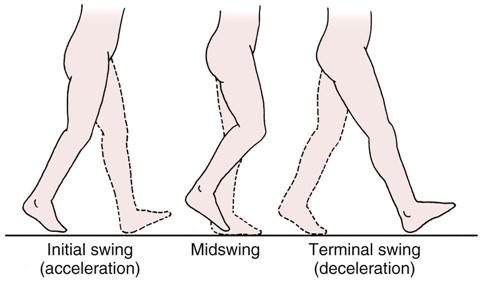
Acceleration occurs when the foot is lifted off the floor. During normal gait, rapid knee flexion and ankle dorsiflexion occur to allow the swing limb to accelerate forward. In some pathological conditions, loss or alteration of knee flexion and ankle dorsiflexion leads to alterations in gait.
The midswing instant occurs when the swing leg is adjacent to the weight-bearing leg, which is in midstance.
During the final instant (terminal swing or deceleration), the swinging leg slows down in preparation for initial contact with the floor. With normal gait, active quadriceps and hamstring muscle actions are required. The quadriceps muscles control knee extension, and the hamstrings control the amount of hip flexion.
During running or with increased velocity, the stance phase decreases and a float phase or double unsupported phase occurs while the double support phase disappears (Figure 14-5).18,21 Although the single-leg stance phase decreases, the load increases two or three times.22 The motion occurring at each of the joints (pelvis, hip, knee, ankle) is similar for walking and for running, but the required range of motion (ROM) increases with the speed of the activity. For example, hip flexion in walking is about 40° to 45°, whereas in running it is 60° to 75°.23
Double-Leg Stance
Double-leg stance is that phase of gait in which parts of both feet are on the ground. In normal gait, it occurs twice during the gait cycle and represents about 25% of the cycle. This percentage increases the more slowly one walks; it becomes shorter as walking speed increases (Figure 14-6) and disappears in running.
Single-Leg Stance
The single-leg stance phase of gait occurs when only one leg is on the ground; this occurs twice during the normal gait cycle and takes up approximately 30% of the cycle.
Normal Parameters of Gait7–11,24
The parameters that follow and their values are considered normal for a population between the ages of 8 and 45 years. It should be pointed out, however, that a relatively normal gait pattern is seen in persons as young as 3 years of age.2 There are, however, differences between individuals of the same sex and between men and women.25 For the majority of the population outside of these ages, there are alterations caused by neurological development, balance control, aging, changes in limb length, and maturation.2 For example, with maturity, walking velocity and step length increase, and cadence decreases.26 It is also important to evaluate gait on the basis of normal gait for someone the same age. This is especially true for children.
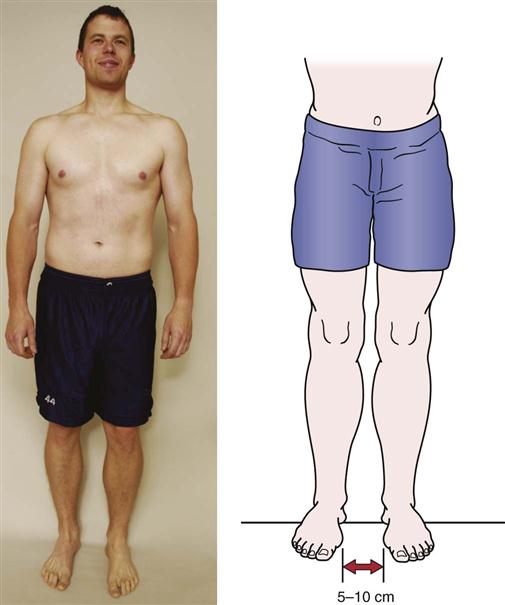
Base (Step) Width
The normal base width, which is the distance between the two feet, is 5 to 10 cm (2 to 4 inches; Figure 14-7). If the base is wider, the examiner may suspect some pathology (e.g., cerebellar or inner ear problems) that results in poor balance, a condition such as diabetes or peripheral neuropathy that may indicate a loss of sensation, or a musculoskeletal problem (e.g., tight hip abductors). In the first two cases, the patient tends to have a wider base to maintain balance. With increased speed, the base width normally decreases to zero, and in some cases, crossover occurs, in which one foot lands where the other should and vice versa. Such crossover can lead to gait alterations and other problems.27
Step Length
Step length, or gait length, is the distance between successive contact points on opposite feet (see Figure 14-1). Normally, this distance is about 72 cm (28 inches) being relatively constant for each individual (i.e., step length is commonly related to preferred walking speed)17,28 and should be equal for both legs. It varies with age and sex with children taking smaller steps than adults and females taking smaller steps than males.22 Height also has an effect: a taller person takes larger steps. Step length tends to decrease with age, fatigue, pain, and disease. If step length is normal for both legs, the rhythm of walking is smooth. If there is pain in one limb, the patient attempts to take weight off that limb as quickly as possible, altering the rhythm.
Stride Length
Stride length is the linear distance in the plane of progression between successive points of foot-to-floor contact of the same foot. The stride length is normally about 144 cm (56 inches) and in reality is one gait cycle.17 Stride length, like step length, decreases with age, pain, disease, and fatigue.19,29 The age changes are often the result of decreased walking pace or speed.29,30
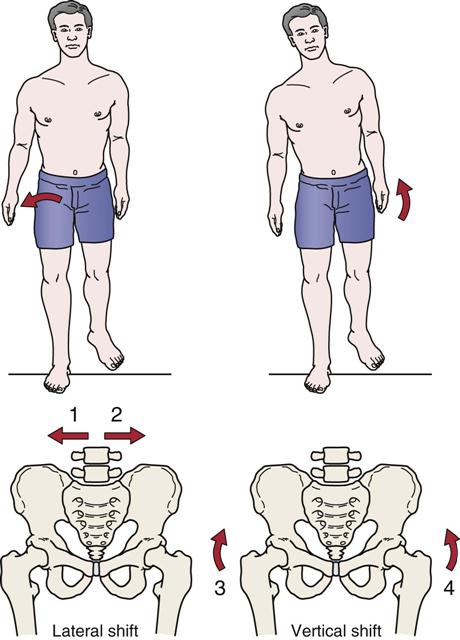
Lateral Pelvic Shift (Pelvic List)
Lateral pelvic shift, or pelvic list, is the side-to-side movement of the pelvis during walking. It is necessary to center the weight of the body over the stance leg for balance (Figure 14-8). The lateral pelvic shift is normally 2.5 to 5 cm (1 to 2 inches). It increases if the feet are farther apart. The pelvic list causes relative adduction of the weight-bearing limb, facilitating the action of the hip adductors. If the abductor muscles are weak, a Trendelenburg gait results (see Figure 14-21).
Vertical Pelvic Shift
Vertical pelvic shift keeps the center of gravity from moving up and down more than 5 cm (2 inches) during normal gait. By means of a vertical pelvic shift, the high point occurs during midstance and the low point during initial contact; the height of these points may increase during the swing phase if the knee is fused or does not bend because of protective spasm or swelling. The head is never higher during normal gait than it is when the person is standing on both feet. Therefore, if a person can stand in an opening, he or she should be able to move through the opening without hitting the head.7 On the swing phase, the hip is lower on the swing side, and the patient must flex the knee and dorsiflex the foot to clear the toe. This action shortens the extremity length at midstance and decreases the center of gravity rise.
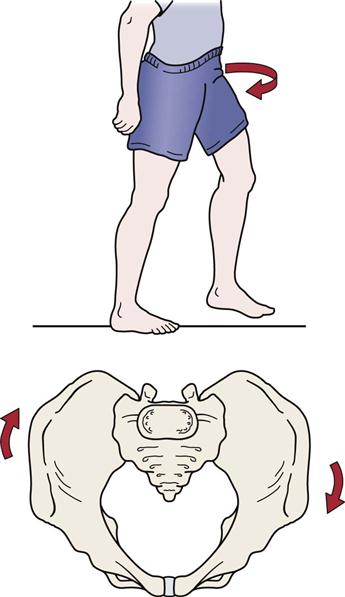
Pelvic Rotation
Pelvic rotation is necessary to lessen the angle of the femur with the floor, and, in so doing, it lengthens the femur (Figure 14-9). The rotation decreases the amplitude of displacement along the path traveled by the center of gravity and thereby decreases the center-of-gravity dip. There is a total of 8° pelvic rotation with 4° forward on the swing leg and 4° posteriorly on the stance leg. To maintain balance, the thorax rotates in the opposite direction. When the pelvis rotates clockwise, the thorax rotates counterclockwise, and vice versa. These concurrent rotations provide counter-rotation forces and help regulate the speed of walking.
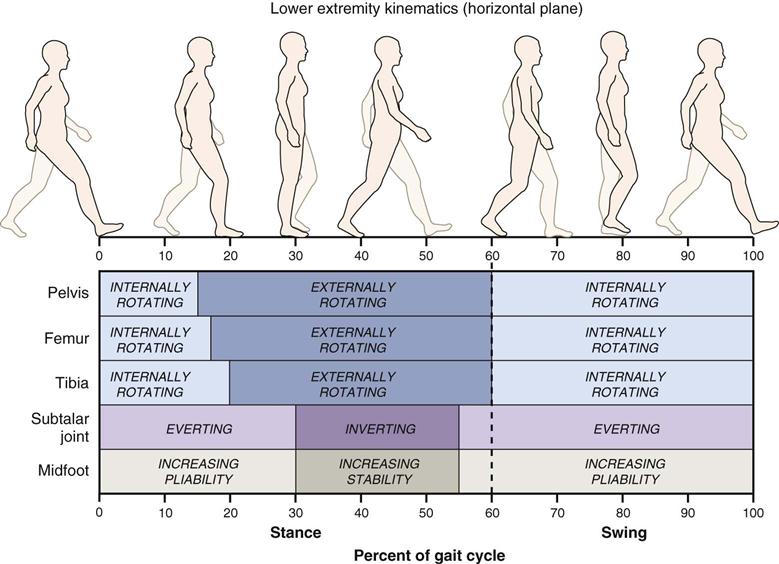
In the lower limb, rotation is evident at each joint (Figure 14-10). The farther the joint is from the trunk, the greater the amount of rotation. For example, rotation in the tibia is three times greater than rotation in the pelvis.7
Center of Gravity
Normally, in the standing position, the center of gravity is 5 cm (2 inches) anterior to the second sacral vertebra; it tends to be slightly higher in men than in women because men tend to have a greater body mass in the shoulder area. The vertical and horizontal displacements of the center of gravity describe a figure-eight, occupying a 5-cm (2-inch) square within the pelvis during walking. The vertical displacement, which describes a smooth sinusoidal curve during walking, can be observed from the side. The patient’s head descends during weight-loading and weight-unloading periods and rises during single-leg stance.
Normal Cadence
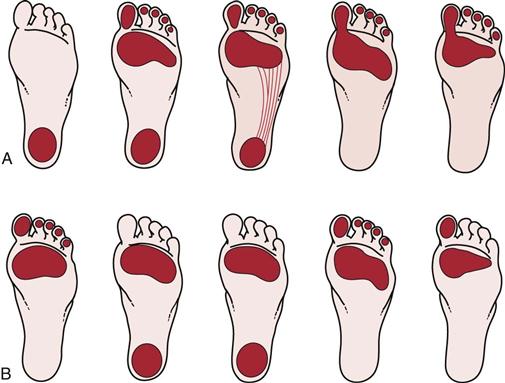
The normal cadence is between 90 and 120 steps per minute which varies, in part, because of the height of the individual.31–34 The cadence of women is usually six to nine steps per minute higher than that of men.33 With age, the cadence decreases. Figure 14-11, A, illustrates the cadence of normal gait from heel strike to toe off showing the changing weight distribution. With pathology or deformity (e.g., a cavus foot [Figure 14-11, B]), this weight-bearing pattern may be altered. As the pace of walking increases, the stride width increases, and the toeing-out angle decreases. Gait speed is about 1.4 m/sec (3 mph).17
Normal Pattern of Gait6–11,17,31,35,36
Stance Phase
As previously mentioned, there are five instants involved during the stance phase of gait. These are now described in order of occurrence. This phase is the closed kinetic chain phase of gait. The action occurring at the various joints causes a chain reaction because of the stresses put on the joints and supporting structures with weight-bearing. The foot becomes the fixed stable segment, and alterations occur from the foot up with the joints of the foot adapting first, followed by those of the ankle, knee, hip, pelvis, spine, and finally the upper limb, which acts as a counterbalance to movement in the lower limb.37 The relations between the joints are constantly changing. Table 14-2 summarizes the movement at the hip, knee, ankle, and foot during the stance phase.38
TABLE 14-2
| Hip | |||
| Kinematic Motion | KINETIC MOTION | ||
| Phase | Hip | External Forces | Internal Forces |
| Heel strike | 20° to 40° of hip flexion moving toward extension; slight adduction and lateral rotation | Reaction force in front of joint; flexion moment moving toward extension; forward pelvic rotation | Gluteus maximus and hamstrings working eccentrically to resist flexion moment; erector spinae working eccentrically to resist forward bend |
| Foot flat | Hip moving into extension, adduction, medial rotation | Flexion moment | Gluteus maximus and hamstrings contracting concentrically to bring hip into extension; erector spinae resisting trunk flexion |
| Midstance | Moving through neutral position; pelvis rotating posteriorly | Reaction force posterior to hip joint; extension moment | Iliopsoas working eccentrically to resist extension; gluteus medius contracting in reverse action to stabilize opposite pelvis; iliopsoas activity continuing |
| Heel off | 10° to 15° extension of hip abduction, lateral rotation | Extension moment decreasing after double-limb support begins | |
| Toe off | Moving toward 10° extension, abduction, lateral rotation | Decrease of extension moment | Adductor magnus working eccentrically to control or stabilize pelvis; iliopsoas activity continuing |
| Knee and Tibia | ||||
| KINEMATIC MOTION | KINETIC MOTION | |||
| Phase | Knee | Tibia | External Forces | Internal Forces |
| Heel strike | In full extension before heel contact; flexing as heel strikes floor | Slight lateral rotation | Rapidly increasing reaction forces behind knee joint causing flexion moment | Quadriceps femoris contracting eccentrically to control rapid knee flexion and to prevent buckling |
| Foot flat | In 20° flexion moving toward extension | Medial rotation | Flexion moment | After foot is flat, quadriceps femoris activity becoming concentric to bring femur over tibia |
| Midstance | In 15° flexion moving toward extension | Neutral | Maximum flexion moment | Quadriceps femoris activity decreasing; gastrocnemius working eccentrically to control excessive knee extension |
| Heel off | In 4° flexion moving toward extension | Lateral rotation | Reaction forces moving anterior to joint; extension moment | Gastrocnemius beginning to work concentrically to start knee flexion |
| Toe off | Moving from near full extension to 40° flexion | Lateral rotation | Reaction forces moving posterior to joint as knee flexes; flexion moment | Quadriceps femoris contracting eccentrically |
| Foot and Ankle | ||||
| KINEMATIC MOTION | KINETIC MOTION | |||
| Phase | Foot | Ankle | External Forces | Internal Forces |
| Heel strike | Supination (rigid) at heel contact | Moving into plantar flexion | Reaction forces behind joint axis; plantar flexion moment at heel strike | Dorsiflexors (tibialis anterior, extensor digitorum longus, and extensor hallucis longus) contracting eccentrically to slow plantar flexion |
| Foot flat | Pronation, adapting to support surface | Plantar flexion to dorsiflexion over a fixed foot | Maximum plantar flexion moment; reaction forces beginning to shift anterior, producing a dorsiflexion moment | Dorsiflexion activity decreasing; tibialis posterior, flexor hallucis longus, and flexor digitorum longus working eccentrically to control pronation |
| Midstance | Neutral | 3° of dorsiflexion | Slight dorsiflexion moment | Plantar flexor muscles (gastrocsoleus and peroneal muscles), activated to control dorsiflexion of the tibia and fibula over a fixed foot, contracting eccentrically |
| Heel off | Supination as foot becomes rigid for push-off | 15° dorsiflexion toward plantar flexion | Maximal dorsiflexion moment | Plantar flexor muscles beginning to contract concentrically to prepare for push-off |
| Toe off | Supination | 20° plantar flexion | Dorsiflexion moment | Plantar flexor muscles at peak activity but becoming inactive as foot leaves ground |
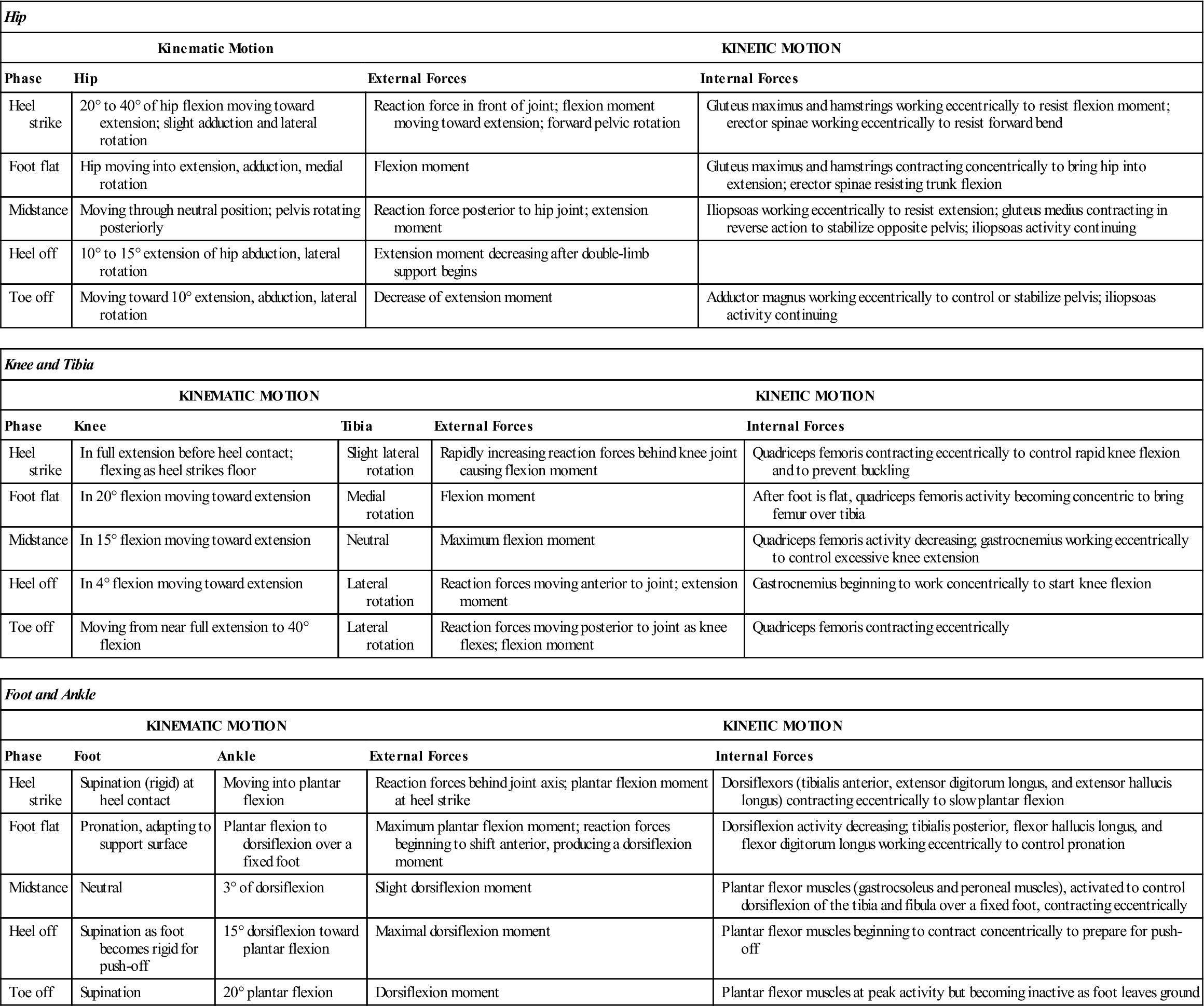
Modified from Giallonardo LM: Gait. In Myers RS, editor: Saunders manual of physical therapy practice, Philadelphia, 1995, WB Saunders, pp. 1108–1109.
Initial Contact (Heel Strike)
Initial contact occurs when the limb first strikes the ground. Normally, this occurs when the heel strikes and the limb is being prepared to take weight. During the initial contact, the pelvis is level and medially rotated on the side of initial contact, whereas the trunk is aligned between the two lower limbs. The hip is flexed 30° to 49° and is medially rotated; the knee is slightly flexed or extended; the tibia is laterally rotated; the ankle is at 90° with the foot supinated; and the hindfoot is everted. At this instant, there is little force going through the limb.
If pain occurs in the heel at this time, it may be caused by a heel spur, bone bruise, heel fat-pad bruise, or bursitis. This pain may cause increased flexion of the knee with early plantar flexion to relieve the stress or pressure on the painful tissues. If the knee is weak, the patient may extend the knee by using the hand or may hit the heel hard on the ground to whip the knee into extension. A patient may do this because of weakness of the muscles (e.g., reflex inhibition, poliomyelitis, an internal derangement of the knee, a nerve root lesion [L2, L3, or L4], femoral neuropathy). In the past, this instant was referred to as “heel strike;” however, with some pathological gaits, heel strike may not be the first instant. Instead, the toes, the forefoot, or the entire foot may initially contact the ground. If the dorsiflexor muscles are weak, the foot drops, slaps, or flops down. The weakness may be caused by a peroneal neuropathy or nerve root lesion (L4). A knee flexion contracture or spasticity may cause the same alteration.
Load Response (Weight Acceptance or Foot Flat)
Load response is a critical event in that the person subconsciously decides whether the limb is able to bear the weight of the body. The trunk is aligned with the stance leg. The pelvis drops slightly on the swing leg side and medially rotates on the same side. The flexed and laterally rotated hip moves into extension, and the knee flexes 15° to 25°. The tibia is medially rotated and begins to move forward over the fixed foot as the body swings over the foot. The ankle is plantar flexed, and the hindfoot is inverted. The foot moves into pronation, because this position unlocks the foot and enables it to adapt to different terrains and postures. The forefoot is pronated, unlocking the subtalar and metatarsal joints to enable them to absorb the shock more effectively, and the plantar aspect is in contact with the floor.
Abnormal responses include excessive or no knee motion as a result of weak quadriceps, plantar flexor contractures, or spasticity.9
Midstance (Single-Leg Support)
The midstance instant is a period of stationary foot support. Normally, the weight of the foot is evenly distributed over the entire foot. The trunk is aligned over the stance leg, and the pelvis shows a slight drop to the swing leg side.
During this stage, there is maximum extension of the hip (10° to 15°) with lateral rotation, and the greatest force is on the hip. Painful hip, knee, or ankle conditions cause this phase to be shortened as the patient hurries through the phase to decrease the pain. If the gluteus medius (L5 nerve root) is weak, Trendelenburg sign is present. The knee flexes, and the ankle is locked at 5° to 8° of dorsiflexion, rolling forward on the forefoot (roll-off). The foot is in contact with the floor; the forefoot is pronated, and the hindfoot is inverted. This instant is a critical event for the ankle. If pain is elicited during this period, the phase is shortened and the heel may lift off early. This pain is commonly caused by conditions such as arthritis, rigid pes planus, fallen metatarsal or longitudinal arches, plantar fasciitis, or Morton metatarsalgia. Therefore, pathology at the hip, ankle, or knee can modify the gait in this phase.
Terminal Stance (Heel Off)
In the final stages, the trunk is initially aligned over the lower limbs and moves toward the stance leg. The pelvis is initially level and posteriorly rotated and then dips to the swing leg side, remaining posteriorly rotated. The heel is in neutral and slight medial rotation; the knee is extended with the tibia laterally rotated. At the ankle, plantar flexion occurs as the critical event. This action helps to smooth the pathway of the center of gravity. The forefoot is initially in contact with the floor, and then the weight on the foot moves forward with plantar flexion so that only the big toe is in contact with the floor. At the same time, the forefoot moves from inversion to eversion.
Preswing (Toe Off)
The preswing phase is the acceleration phase as the toe pushes the leg forward. The trunk remains erect, the pelvis remains posteriorly rotated, and the hip is extended and slightly medially rotated. The knee flexes to 30° to 35° (critical event), and the ankle is plantar flexed. Because the center of gravity is anterior to the hip, the hip can be accelerated forward in initial swing.
If pain is elicited during this instant, it may be caused by a hallux rigidus, turf toe, or any other pathology involving the great toe (hallux), especially the metatarsophalangeal joint of the hallux. With injury to the joint, the patient is unable to push off on the medial aspect of the foot; instead, the patient pushes off on the lateral aspect of the foot to compensate for the painful metatarsophalangeal joint or, in some cases, a painful metatarsal arch resulting from increased pressure on the metatarsal heads. If the plantar flexors are weak (e.g., S1–S2 nerve root pathology), push-off may be absent. During this phase, the foot pronates so that there is a rigid base for better push-off.
During walking, a cane can be used to decrease the load on the limb. Lyu and associates39 have shown that using a cane in the contralateral upper limb, if the cane tip touches the ground at the same time as the heel, can reduce the force at heel strike by 34%, by 25% at midstance, and about 30% at toe off.
Swing Phase
The swing phase of gait involves the lower limb in an open kinetic chain; the foot is not fixed on the ground, and the stresses on the limb are therefore less and easier to dissipate. During this phase, alterations occur from the spine down through the pelvis, hip, ankle, and foot. The pelvis and hip provide the most stability in the lower limb during the non–weight-bearing phase. Table 14-3 summarizes the motions occurring in the lower limb during the swing phase.
TABLE 14-3
| ACCELERATION TO MIDSWING | MIDSWING TO DECELERATION | |||
| Joint | Kinematic Motion | Kinetic Motion | Kinematic Motion | Kinetic Motion |
| Hip | Slight flexion (0° to 15°) moving to 30° flexion and lateral rotation to neutral | Hip flexors working concentrically to bring limb through; contralateral gluteus medius concentrically contracting to maintain pelvis position | Continued flexion at about 30° to 40° | Gluteus maximus contracting eccentrically to slow hip flexion |
| Knee | 30° to 60° knee flexion and lateral rotation of tibia moving toward neutral | Hamstrings concentrically contracting | Moving to near full extension and slight lateral tibial rotation | Quadriceps femoris contracting concentrically and hamstrings contracting eccentrically |
| Ankle and foot | 20° dorsiflexion and slight pronation | Dorsiflexors contracting concentrically | Ankle in neutral; foot in slight supination | Dorsiflexors contracting isometrically |
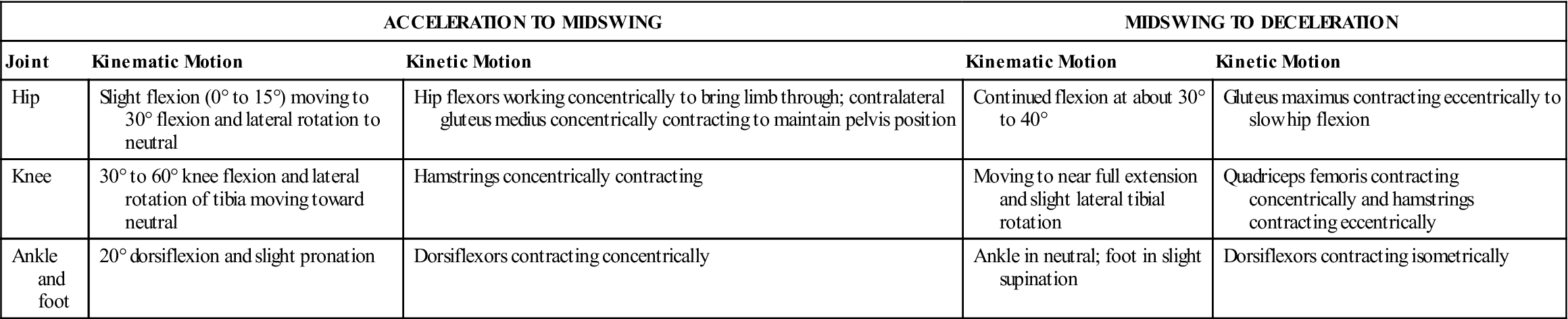
From Giallonardo LM: Gait. In Myers RS, editor: Saunders manual of physical therapy practice, Philadelphia, 1995, WB Saunders, p. 1110.
The three instants composing the swing phase of gait are now described in order of occurrence.
Initial Swing
During the first subphase of acceleration (Figure 14-12), flexion and medial rotation of the hip and flexion of the knee occur. The pelvis medially rotates and dips to the swing leg side. The trunk is aligned with the stance leg. In addition, the ankle continues to plantar flex. The foot is not in contact with the floor. The forefoot continues supinating, and the hindfoot continues everting. The dorsiflexor muscles of the ankle contract to allow the foot to clear the ground, and the knee exhibits its maximum flexion during gait of about 60°. If the quadriceps muscles are weak, the trunk muscles thrust the pelvis forward to provide forward momentum to the leg.
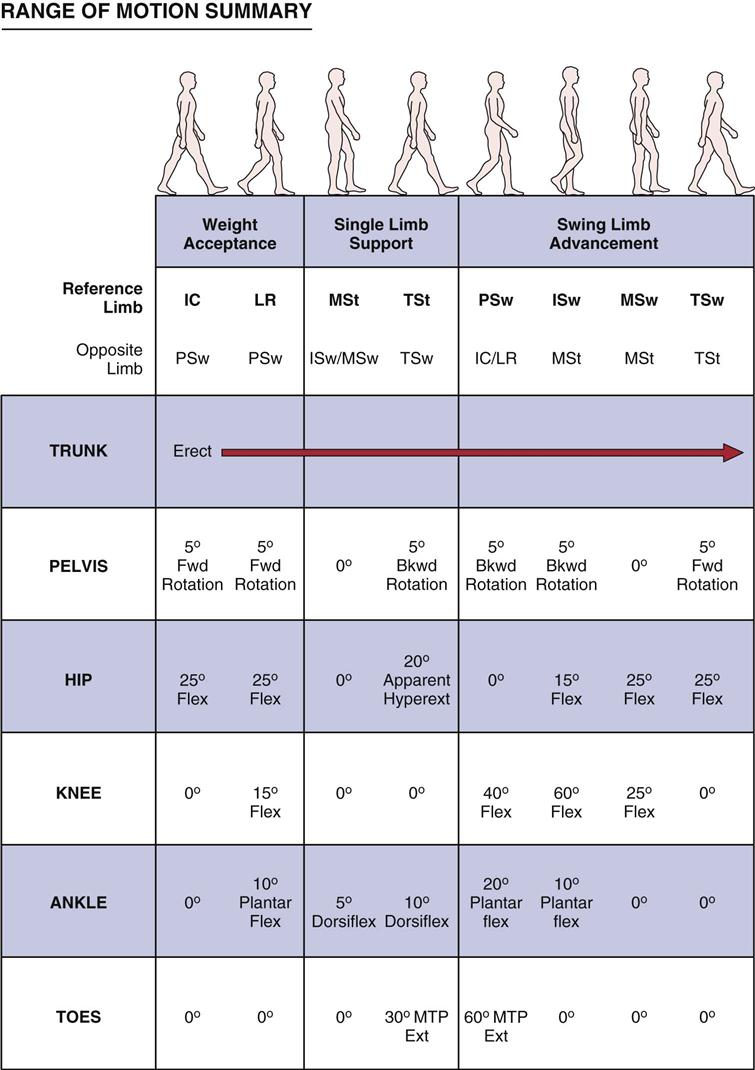
IC, Initial contact; ISw, initial swing; LR, load response; MSt, midstance; MSw, midswing; PSw, preswing; TSt, terminal stance; TSw, terminal swing. (Copyright 1991 LAREI, Rancho Los Amigos Medical Center, Downey, CA 90242; from The Pathokinesiology Service and The Physical Therapy Department, Rancho Los Amigos Medical Center: Observational Gait Analysis. Downey, CA, Los Amigos Research and Educational Institute, Inc., 1996, p. 30.)
Midswing
During the midswing instant, the hip continues to flex and medially rotate, and the knee continues to flex. The ankle is in the anatomical or plantigrade position (90°) for the first 25% of the stance phase to permit the foot and midtarsal joints to unlock so that the foot can adapt to uneven terrain when it begins weight-bearing. The forefoot is supinated, and the hindfoot is everted. The pelvis and trunk are in the same position as during the previous stage. If the ankle dorsiflexor muscles are weak (e.g., drop foot), the patient demonstrates a steppage gait (see Figure 14-27). In such a gait, the hip flexes excessively so that the toes can clear the ground.
Terminal Swing (Deceleration)
During the final subphase, the hip continues to flex and medially rotate, and the knee reaches its maximum extension. At the ankle, dorsiflexion has occurred. The forefoot is supinated, and the hindfoot is everted. The trunk and pelvis maintain the same position as before. The hamstring muscles contract during the terminal phase to slow the swing; if the hamstrings are weak (e.g., S1–S2 nerve root lesion), heel strike may be excessively harsh to lock the knee in extension.
Joint Motion During Normal Gait
Although there is a tendency to talk about gait as action around joints, the examiner must not forget that muscles play a significant role in what happens at the joints. Table 14-4 illustrates the actions of some of the muscles used during gait.40
TABLE 14-4
Muscle Actions During Gait Cycle
| Phase of Gait | Mechanical Goals | Active Muscle Groups | Examples |
| Stance Phase | |||
| Initial contact | Position foot, begin deceleration | Ankle dorsiflexors, hip extensors, knee flexors | Anterior tibialis, gluteus maximus, hamstrings |
| Loading response | Accept weight, stabilize pelvis, decelerate mass | Knee extensors, hip abductors, ankle plantar flexors | Vasti, gluteus medius, gastrocnemius, soleus |
| Midstance | Stabilize knee, preserve momentum | Ankle plantar flexors (isometric) | Gastrocnemius, soleus |
| Terminal stance | Accelerate mass | Ankle plantar flexors (concentric) | Gastrocnemius, soleus |
| Swing Phase | |||
| Preswing | Prepare for swing | Hip flexors | Iliopsoas, rectus femoris |
| Initial swing | Clear foot, vary cadence | Ankle dorsiflexors, hip flexors | Tibialis anterior, iliopsoas, rectus femoris |
| Midswing | Clear foot | Ankle dorsiflexors | Tibialis anterior |
| Terminal swing | Decelerate shank, decelerate leg, position foot, prepare for contact | Knee flexors, hip extensors, ankle dorsiflexors, knee extensors | Hamstrings, gluteus maximus, tibialis anterior, vasti |
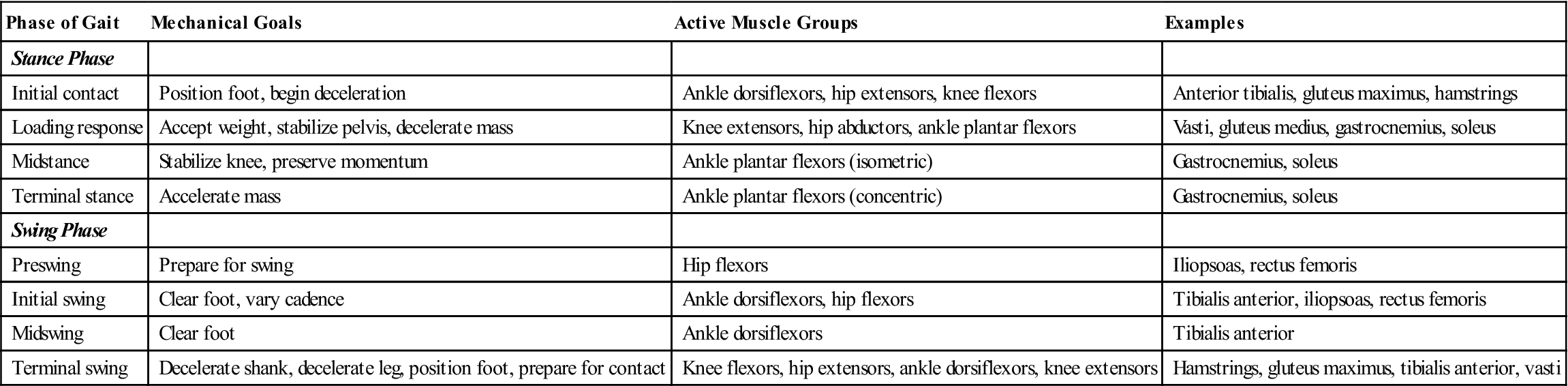
From Rab GT: Muscle. In Rose J, Gamble JG, editors: Human locomotion, Baltimore, 1994, Williams & Wilkins, p. 113.
Hip.
The function of the hip is to extend the leg during the stance phase and flex the leg during the swing phase. The ligaments of the hip help to stabilize it in extension. The hip extensors help to initiate movement, as do the hip flexors; both groups of muscles work phasically.41 The hip flexors (primarily the iliopsoas muscle) contract to slow extension; the hip extensors (primarily the hamstring muscles) contract to slow flexion. In this way, they work eccentrically. The abductor muscles provide stability during single-leg support, a critical event for the hip.41
If there is loss of movement of the hip, the compensatory mechanisms are increased mobility of the knee on the same side and increased mobility of the contralateral hip. In addition, the lumbar spine shows increased mobility.
Knee.
When the knee is in flexion during the first three instants of the stance phase of gait, it acts as a shock absorber. Painful knees are not able to do this. One of the critical events of the knee is extension. The functions of the knee during gait are to bear weight, absorb shock, extend the stride length, and allow the foot to move through its swing. The quadriceps muscles use only 4% to 5% of their maximum voluntary contraction to extend the knee, but in so doing, they help to control weight acceptance. The hamstring muscles flex the knee and slow the leg in the swing phase, working eccentrically.
If the knee has a flexion deformity, the hip is flexed and, therefore, loses its extension power, which is a critical event for the hip. Pathological conditions, such as patellofemoral syndrome, also cause deviations from normal gait. For example, patients with patellofemoral syndrome show less knee flexion during the single-leg stance phase, combined with lateral femoral rotation during the swing phase.42 On heel strike to foot flat, the femur then medially rotates, and if this compensating medial rotation is too great, it causes excessive pronation, which then stresses the medial aspect of the patellofemoral joint.
Gastrocnemius and Soleus.
The gastrocnemius and soleus muscles are important in gait. They use 85% of their maximum voluntary contraction during normal walking. These muscles help to restrain the body’s forward momentum during forward movement. They also contribute to knee and ankle stability, restrain forward rotation of the tibia on the talus during the stance phase, and minimize the vertical pelvic shift, thereby conserving energy.43 To accomplish these functions during gait, the triceps surae work eccentrically and concentrically.
Foot and Ankle.
The foot and ankle play major roles in gait in that the various joints allow the foot to accommodate to the ground. The joints of the foot and ankle work interdependently during normal gait. When the heel contacts the ground, the lower limb becomes a closed kinetic chain, and movements and stresses must be absorbed by the structures of the lower limb.
When looking at the ankle, the examiner should observe immediate plantar flexion at initial contact. Loss of this plantar flexion (e.g., tibial nerve neuropathy) results in an inability to transfer weight to the anterior foot, increased ankle dorsiflexion, and increased knee flexion. In addition, the duration of single-leg stance on the affected side decreases, and the step length on the opposite side decreases. Furthermore, quadriceps action at the knee increases because of the lack of knee stability caused by the loss of the triceps surae with the end result being that walking velocity decreases.43 The foot then dorsiflexes through midstance or single-leg stance, with maximum dorsiflexion being reached just before heel off. The examiner should note whether there is sufficient plantar flexion during push-off.
Overview and Patient History
The assessment of a patient’s gait should be included in any assessment of the lower limb. The examiner must keep in mind that the posture of the head, neck, thorax, and lumbar spine can affect gait even if no pathology is evident in the lower limb. The examiner must be able to identify the action of each body segment and note any deviation from normal during the individual phases of gait. For this reason, it is important to understand the normal parameters of gait and the mechanism of gait as it occurs. With this knowledge, the ways in which the gait is altered under pathological conditions can be better understood.
Musculoskeletal pathology tends to modify gait because of muscle weakness, pain, or altered ROM, so the examiner should watch closely for these factors when observing gait. Many patients can adapt automatically to these changes, provided they have normal sensation and can develop selective control.9 Patients with upper motor neuron lesions have greater alterations and cannot easily adapt because, in addition to the musculoskeletal problems, they also present with spasticity, control problems, and sensory disturbances.9 It is important that the examiner read the patient’s chart and take a history from the patient regarding any disease or injury, past or present, that may be causing gait problems.
Observation
The examiner should first perform a general overview of the patient’s posture, looking for any asymmetry, and then observe the patient’s gait, looking at stride length, step frequency, time of swing, speed of walking, and duration of the complete walking cycle. This is normally done with the patient in shorts, wearing no shoes or socks. If gait is observed wearing shoes, the same shoes should be used for each test.44 A steady gait pattern is usually established within three steps; it is initiated by the body’s becoming unbalanced so that the patient can lift one foot off the ground to take the first step.45 After this overview is completed, the examiner can look at specific parts of the gait in terms of phases and what happens at each joint during these phases.
Because gait constantly changes as one stops and starts, hurries, dawdles, and walks with others, it is important to remember whether the movements the patient is capable of are normal and whether the speeds, phases, strides, and durations of the cycles occur in normal combinations. In addition to observing walking at a normal speed, the patient’s slow and fast gait speeds should be examined to see whether these changes affect the gait. The examiner must watch the upper limbs and trunk, as well as the lumbar spine, pelvis, hips, knees, feet, and ankles during these changes. Female patients should be in a bra and briefs, and male patients should be in shorts. The patient should walk barefoot. In this way, the motions of the toes, feet, legs, pelvis, trunk, and upper limbs can properly be observed.
The examiner should ask the patient to walk in the usual manner, using any aids necessary (e.g., parallel bars, crutches, walker, canes). While the patient is walking, the examiner makes an initial general observation of any obvious limp or deformity.
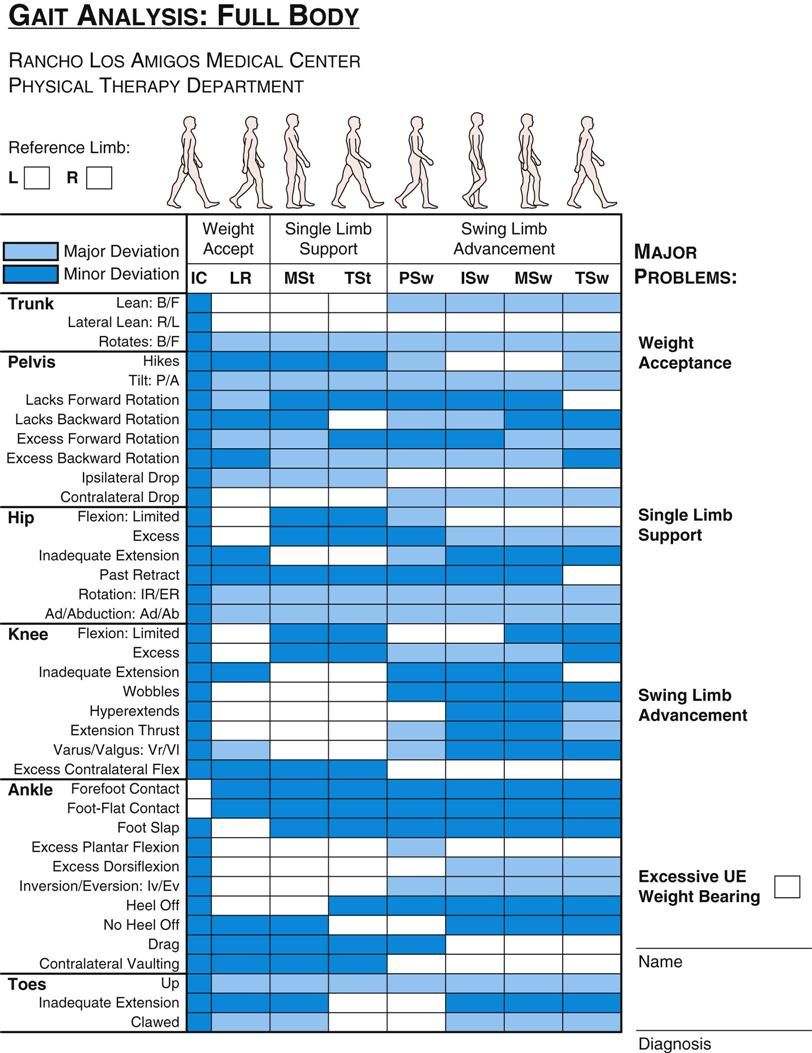
The examiner should observe the gait from the front, from behind, and from the side, in each instance observing from proximal to distal and watching the pelvis and lumbar spine down to the ankle and foot as well as from the foot up. For example, in the swing phase (open kinetic chain) movement starts proximally and moves distally. In the stance phase (closed kinetic chain), movement is reversed, starting in the foot and moving proximally. The examiner should observe the movements in the trunk and upper limbs, which normally are in the opposite direction to those of the lower limbs. This method provides a sequential, thorough manner of assessment. Rancho Los Amigos Medical Center has developed a useful gait analysis chart (Figure 14-13). By using the chart during observation, the examiner can determine deviations and their effect on gait in an easily used and easily retained method of recording. The dark gray boxes indicate what normally should occur; the lighter gray and white boxes indicate minor and major deviations from the normal, respectively. Minor deviations imply that the functional task of walking is not affected. Major deviations imply that the mechanics of walking are affected adversely.46
Anterior View
When observing from the front as the patient walks, the examiner should note whether any lateral tilt of the pelvis occurs, whether there is any sideways swaying of the trunk, whether the pelvis rotates on a horizontal plane, whether the trunk and upper extremity rotate in the opposite direction to the pelvis, and whether reciprocal arm swing is present. Usually, the trunk and upper extremity rotation is approximately 180° out of phase with the pelvis—that is, as the pelvis and lower limb rotate one way, the trunk and upper limb rotate in the opposite direction. This action helps provide a balancing effect and smoothes the forward progression of the body. The examiner may also note movements at the hip (rotation and abduction-adduction), knee (rotation and abduction-adduction), and ankle and foot (amount of toe-out and toe-in, dorsiflexion-plantar flexion, supination-pronation). The examiner should note any bowing of the femur or the tibia, any medial or lateral rotation of the hips, femur, or tibia, and the position of the feet as the patient goes through the gait cycle (Figure 14-14). This view is best used to examine the weight-loading period of the gait cycle. The examiner should also note whether there is any abduction or circumduction of the swing leg, whether there is atrophy of the musculature of the anterior thigh and leg, and whether the base width is normal.
Lateral View
From the side, the examiner should observe rotation of the shoulder and thorax during the gait cycle, as well as reciprocal arm swing. Spinal posture (e.g., lordosis), pelvic rotation, and movements in the joints of the lower limbs should be noted. These movements include flexion-extension at the hip, flexion-extension at the knee, and dorsiflexion-plantar flexion at the ankle. From the lateral aspect, the examiner may also observe step length, stride length, cadence, and the other time dimensions of gait (see Figure 14-6).36 This view allows observation of the interactions between the walking surface and the various body parts.
The examiner must remember that there may be some compensation by the lumbar spine for limitation of movement in the hip. The patient should be observed to determine whether there is sufficient knee extension at initial contact, followed almost immediately by slight flexion until the foot makes contact with the floor; whether there is control of the slightly flexed knee during load response and midstance; and whether there is sufficient flexion during preswing and initial swing. Also, any hyperextension of the knee during the gait cycle should be noted. Finally, the examiner should note whether there is coordination of movement among the hip, knee, and ankle; even or uneven gait length; and even or uneven duration of steps.
As the patient moves from initial contact to loading response, the foot flexes immediately, and the knee flexes until the foot is flat on the floor. During this period, the hip is also flexed. During midstance, the ankle dorsiflexes as the body pivots in an arc over the stationary foot. At the same time, the hip and knee extend, lengthening the leg. As the patient moves from terminal stance to preswing, the ankle plantar flexes to raise the heel, and the hip and knee flex as the weight is transferred to the opposite leg.
During the initial swing, the ankle is plantar flexed, and the hip and knee are maximally flexed. As the leg progresses to midswing, the ankle dorsiflexes, and the hip and knee begin to extend. As the patient moves from midswing to terminal swing, the ankle remains in the neutral position while the hip and knee continue extending. As the leg moves from terminal swing to initial contact, the knee reaches maximum extension; the ankle remains in neutral, and no further hip extension occurs at this stage.
Posterior View
When observing the gait cycle from behind, the examiner should notice the same structures that were viewed from the front. Rotation of the shoulders and thorax, reciprocal arm swing, and pelvic list and rotation may be noted posteriorly, as well as hip, knee, ankle, and subtalar joint movement. Heel rise and base of support (base width) are easier to view posteriorly. Any abnormal abduction or adduction movements or lateral displacement of the body segments should be noted. This view is best to examine the weight-unloading period of the gait cycle. The examiner can note whether heel rise is equal for both feet and whether the heels turn in or out. The observation should also include lateral movement of the spine and the musculature of the back, buttocks, posterior thigh, and calf.
Footwear
The patient should be asked to walk in normal footwear as well as in bare feet. The examiner should take time to observe the patient’s footwear and observe any wearing down of the heels or socks, the condition of the shoe uppers, creases, and so on. The feet should also be examined for callus formations, blisters, corns, and bunions. Different shoes can modify a patient’s gait and the amount of energy necessary to perform gait. For example, high-heeled shoes alter movement, especially at the knee and ankle, which in turn increases the vertical loading.47
Examination
Most gait assessment involves observation. However, the examiner should take time, especially if he or she notices altered gait, to measure muscle strength (active and resisted movement) and range of movement (active and passive movement) at each joint involved in the gait cycle.
The parameters of gait (see normal parameters of gait) may also be measured to see if there are differences between the left and right gait cycles.48,49 Leg length discrepancies (see Chapter 11 for leg length measurement) may also affect gait. Children tend to have better compensation mechanisms for leg length discrepancies than do adults.50 Table 9-7 gives functional causes of leg length differences. Tables 11-10, 12-2, and 13-3 outline malalignments that may also affect gait.
Locomotion Scores
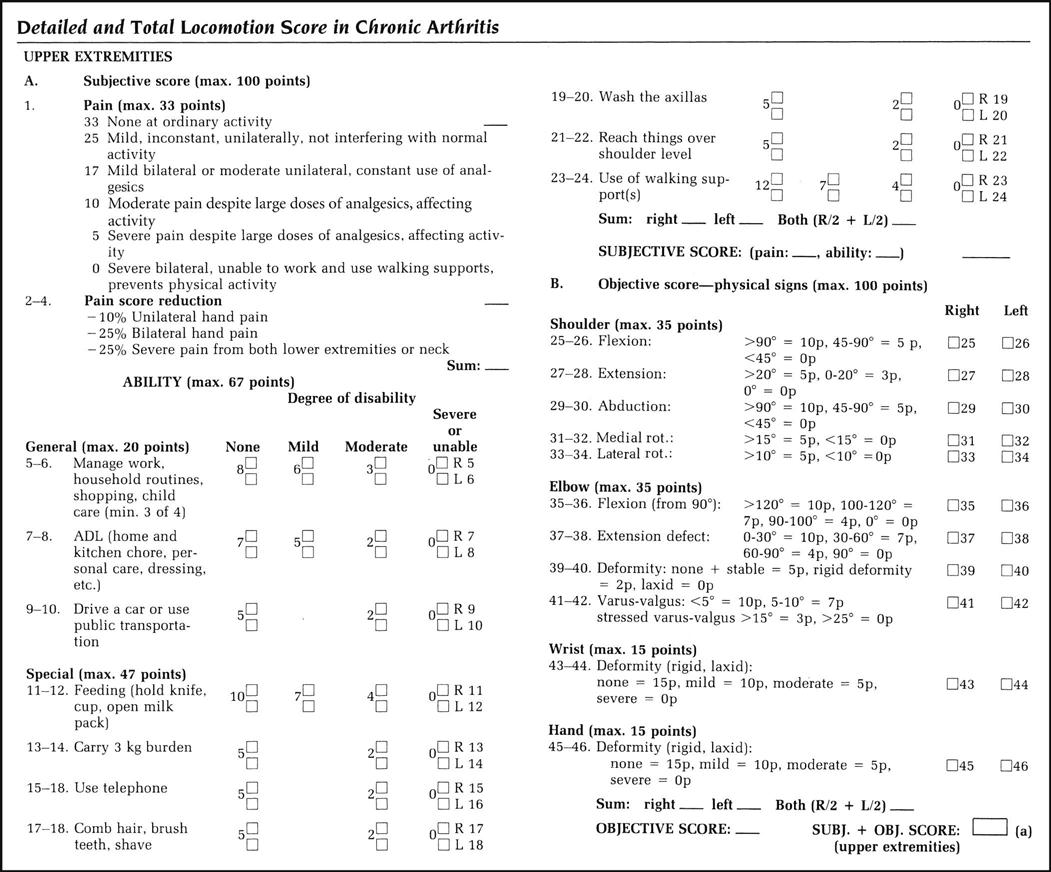
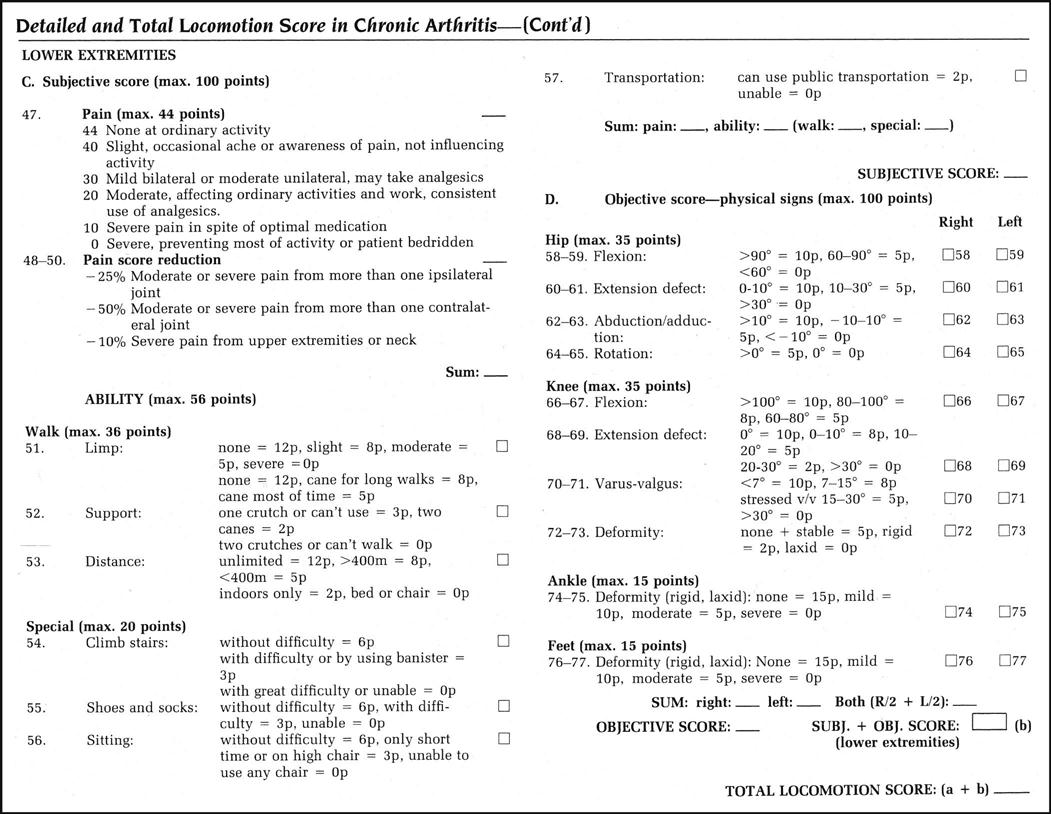
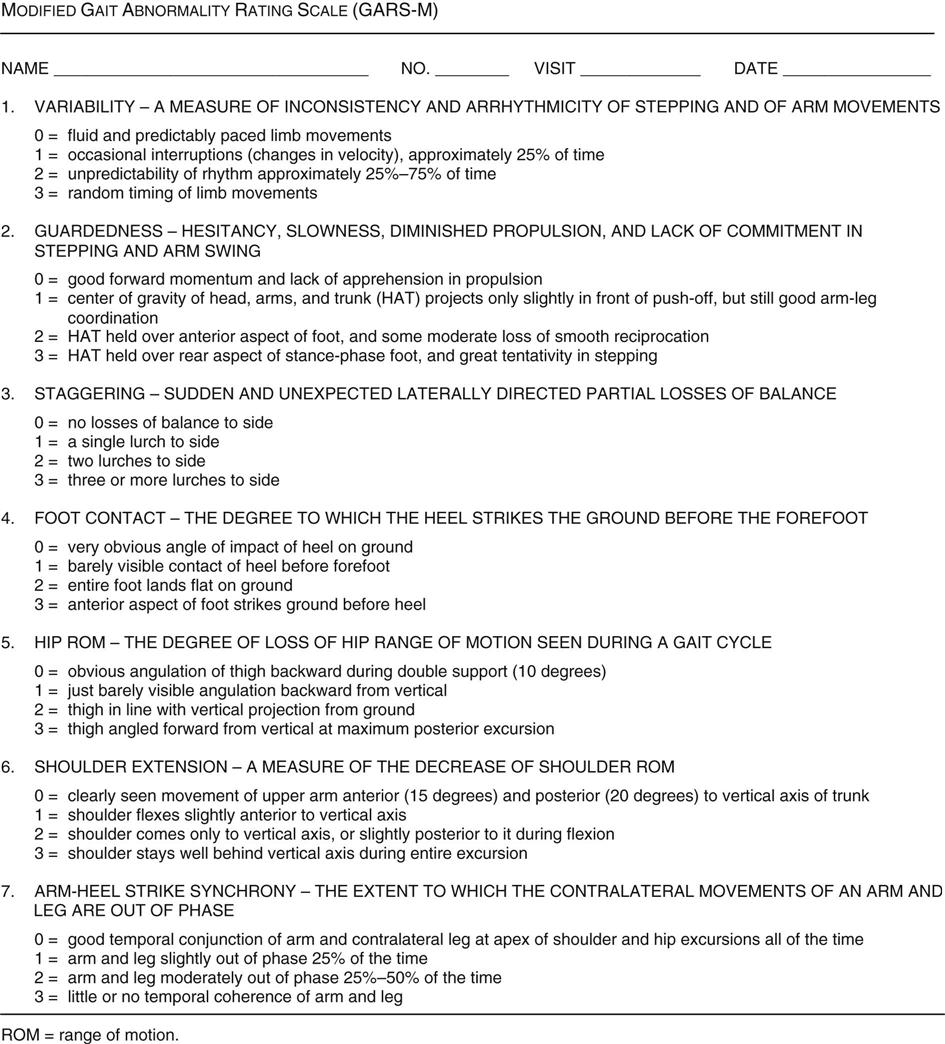
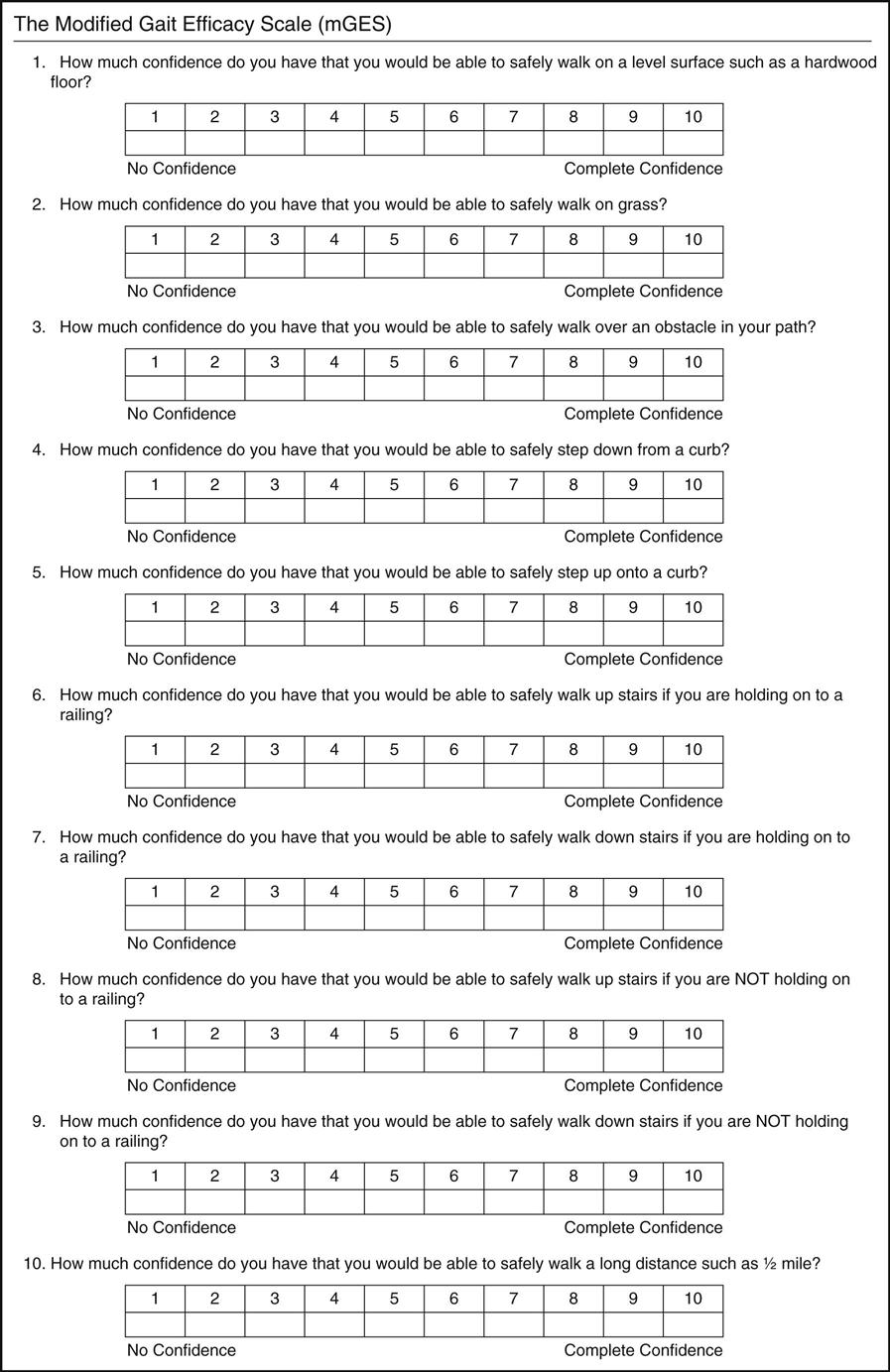
In addition to the detailed assessment of gait, locomotion scales or grading systems have been developed that include subjective and objective scores, which are combined for a total score. Figure 14-15 is a locomotion scoring scale that was developed for rheumatoid arthritis.51 Figure 14-16 shows the modified Gait Abnormality Scale (GARS-M) for elderly people who may be at high risk to falling.52–54 In addition to including all aspects of locomotion, it gives an overall estimation of functional disability for patients with rheumatoid arthritis. Wolf and associates reported on the Emory Functional Ambulation Profile and established its reliability and validity.55,56 The profile measures different tasks and surfaces for stroke patients and can differentiate between those suffering from a stroke and normals. The profile does time trials and measures such things as a 5-meter (16.4 feet) walk on bare floor and carpeted floor, an “up and go” task, negotiating an obstacle course, and stair climbing. The Walking Safety Scale (Grille d’évaluation de la securité à la marche [GEM]) is a scale developed to measure walking ability and safety.16,57 It is a functional scale divided into basic level (walking short distances in different directions), advanced level (walking and doing other activities or walking on different surfaces), and outdoor activities, and can test patients with walking aids. It is a scale that has patient input (perception and safety) and examiner (rater) input. Table 14-5 shows the walking items for each subscale. The modified Gait Efficacy Scale (mGES) (Figure 14-17) was designed to measure walking confidence in older adults during everyday activities.58 Other functional tests include the Get Up and Go Test,59 the Functional Ambulatory Classification Scale,60,61 Figure-of-8 Walk Test,62 Functional Gait Assessment,63 and the Performance Oriented Balance and Mobility Assessment (POMA).64
TABLE 14-5
Walking Items for Each Sub-Scale of the Walking Safety Scale
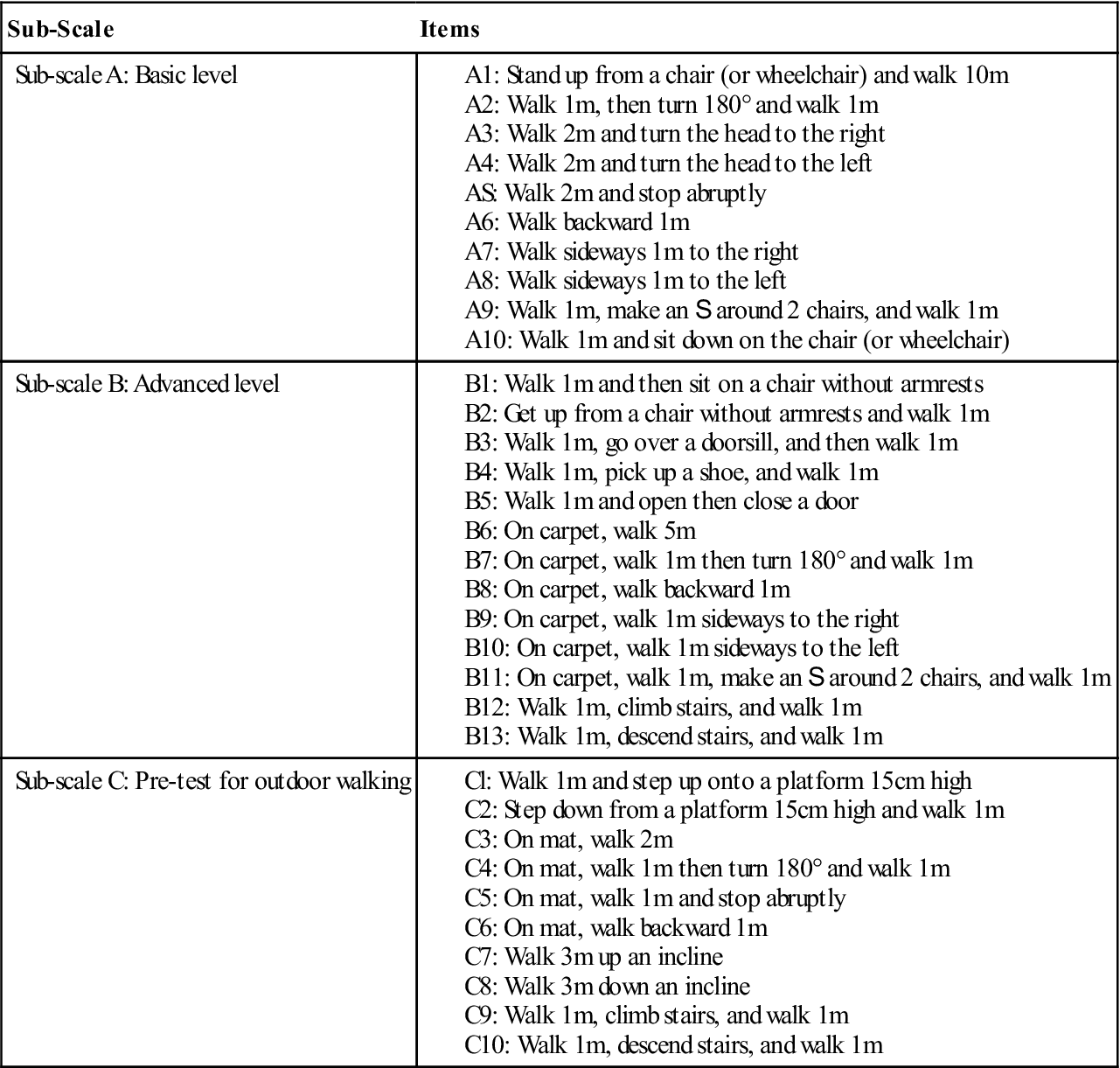
From Kaegi C, et al: Development of a walking safety scale for older adults. Part 1: content validity of the GEM scale. Physiother Can 60:264–273, 2008.
Compensatory Mechanisms
The examiner must try to determine the primary cause of gait faults and the compensatory factors used to maintain an energy-saving gait. The patient tries to use the most energy-saving gait possible.65 Speed of walking can also modify many of the normal parameters of gait.66 Therefore, not only the gait pattern but also the speed of the activity and its effects must be noted. This type of assessment allows the examiner to set appropriate goals and plan a logical approach to treatment.
Abnormal Gait
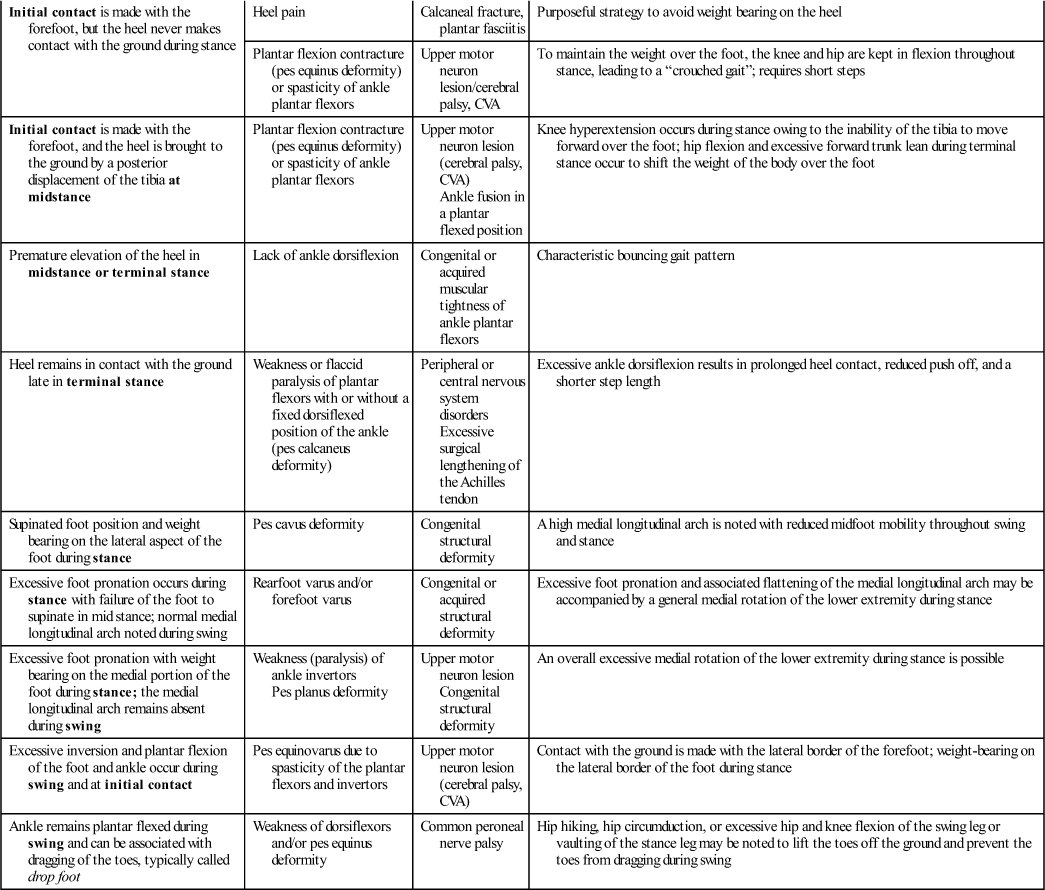
Gait deviations can occur for three reasons. First, they may occur because of pathology or injury in the specific joint (Table 14-6). Second, they may occur as compensations for injury or pathology in other joints on the same or ipsilateral side. Finally, they may occur as compensations for injury or pathology on the opposite or contralateral limb (Table 14-7).17 Some of the more common gait abnormalities are discussed next, but this list is by no means inclusive.
TABLE 14-6
Gait Deviations Secondary to Specific Impairments*†
| Gait Deviations at the Hip/Pelvis/Trunk Secondary to Specific Hip/Pelvis/Trunk Impairments | |||
| Observed Gait Deviation at the Hip/Pelvis/Trunk | Likely Impairment | Selected Pathologic Precursors | Mechanical Rationale and/or Associated Compensations |
| Backward trunk lean during loading response | Weak hip extensors | Paralysis of poliomyelitis | This action moves the line of gravity of the trunk behind the hip and reduces the need for hip extension torque |
| Lateral trunk lean toward the stance leg; since this movement compensates for a weakness, it is often called “compensated” Trendelenburg gait and is referred to as a waddling gait if bilateral | Marked weakness of the hip abductors | Guillain-Barré or poliomyelitis | Shifting the trunk over the supporting limb reduces the demand on the hip abductors |
| Hip pain | Arthritis | Shifting the trunk over the supporting lower extremity reduces compressive joint forces associated with the action of hip abductors | |
| Excessive downward drop of the contralateral pelvis during stance (referred to as positive Trendelenburg sign if present during single-limb standing) | Mild weakness of the gluteus medius of the stance leg | Guillain-Barré or poliomyelitis | Although the Trendelenburg sign may be seen in single-limb standing, a compensated Trendelenburg gait is often seen in severe weakness of the hip abductors |
| Forward bending of the trunk during mid and terminal stance, as the hip is moved over the foot | Hip flexion contracture | Hip osteoarthritis | Forward trunk lean is used to compensate for lack of hip extension; an alternate adaptation could be excessive lumbar lordosis |
| Hip pain | Hip osteoarthritis | Keeping the hip at 30° of flexion minimizes intraarticular pressure | |
| Excessive lumbar lordosis in terminal stance | Hip flexion contracture | Arthritis | Lack of hip extension in terminal stance is compensated for by increased lordosis |
| Trunk lurches backward and toward the unaffected stance leg from heel off to mid swing | Hip flexor weakness | L2–L3 nerve compression | Hip flexion is passively generated by a backward movement of the trunk |
| Posterior tilt of the pelvis during initial swing | Hip flexor weakness | L2–L3 nerve compression | Abdominals are used during initial swing to advance the swing leg |
| Hip circumduction: semicircle movement of the hip during swing—combining hip flexion, hip abduction and forward rotation of the pelvis | Hip flexor weakness | L2–L3 nerve compression | Semicircular movement combining hip flexion, hip abduction, and forward rotation of the pelvis |
| Gait Deviations at the Knee Secondary to Specific Knee Impairments | |||
| Observed Gait Deviation at the Knee | Likely Impairment | Selected Pathologic Precursors | Mechanical Rationale and/or Associated Compensations |
| Rapid extension of the knee (knee extensor thrust) immediately after initial contact | Spasticity of the quadriceps | Upper motor neuron lesion | Depending on the status of the posterior structures of the knee, may occur with or without knee hyperextension |
| Knee remains extended during the loading response, but there is no extensor thrust | Weak quadriceps | Femoral nerve palsy, L3–L4 compression neuropathy | Knee remains fully extended throughout stance; an associated anterior trunk lean in the early part of stance moves the line of gravity of the trunk, slightly anterior to the axis of rotation of the knee; this keeps the knee extended without action of the knee extensors; this gait deviation may lead to an excessive stretching of the posterior capsule of the knee and eventual knee hyperextension (genu recurvatum) during stance |
| Knee pain | Arthritis | Knee is kept in extension to reduce the need for quadriceps activity and associated compressive forces; it may be accompanied by an antalgic gait pattern characterized by a reduced stance time and shorter step length | |
| Genu recurvatum (hyperextension) during stance | Knee extensor weakness (see the two previously described gait deviations above) | Poliomyelitis | Secondary to progressive stretching of the posterior capsule of the knee |
| Varus thrust during stance | Laxity of the posterior and lateral ligamentous joint structures of the knee | Traumatic injury or progressive laxity | Rapid varus deviation of the knee during midstance, typically accompanied by knee hyperextension |
| Flexed position of the knee during stance and lack of knee extension in terminal swing | Knee flexion contracture > 10° (genu flexum) Hamstring overactivity (spasticity) |
Upper motor neuron lesion | Associated increase in hip flexion and ankle dorsiflexion during stance |
| Knee pain and joint effusion | Trauma or arthritis | Knee is kept in flexion since this is the position of lowest intraarticular pressure | |
| Reduced or absent knee flexion during swing | Spasticity of knee extensors Knee extension contracture |
Upper motor neuron lesion Immobilization (cast, brace) or surgical fusion |
Compensatory hip hiking and/or hip circumduction could be noted |
| Gait Deviations at the Ankle/Foot Secondary to Specific Ankle/Foot Impairments | |||
| Observed Gait Deviation at the Ankle/Foot | Likely Impairment | Selected Pathologic Precursors | Mechanical Rationale and/or Associated Compensations |
| “Foot slap”: rapid ankle plantar flexion occurs following heel contact; the name foot slap is derived from the characteristic noise made by the forefoot hitting the ground | Mild weakness of ankle dorsiflexors | Common peroneal nerve palsy and distal peripheral neuropathy | Ankle dorsiflexors have sufficient strength to dorsiflex the ankle during swing but not enough to control ankle plantar flexion after heel contact; no other gait deviations |
| “Foot flat”: Entire plantar aspect of the foot touches the ground at initial contact,‡ followed by normal, passive ankle dorsiflexion during the rest of stance | Marked weakness of ankle dorsiflexors | Common peroneal nerve palsy and distal peripheral neuropathy | Sufficient strength of the dorsiflexors to partially, but not completely, dorsiflex the ankle during swing; normal dorsiflexion occurs during stance as long as the ankle has normal ROM; no other gait deviations |
| Initial contact with the ground is made by the forefoot followed by the heel region; normal passive ankle dorsiflexion occurs during stance | Severe weakness of ankle dorsiflexors | Common peroneal nerve palsy and distal peripheral neuropathy | No active ankle dorsiflexion is possible during swing; normal dorsiflexion occurs during stance as long as the ankle has normal ROM; likely requires excessive knee and hip flexion during swing to avoid catching toes on the ground |
| Initial contact is made with the forefoot, but the heel never makes contact with the ground during stance | Heel pain | Calcaneal fracture, plantar fasciitis | Purposeful strategy to avoid weight bearing on the heel |
| Plantar flexion contracture (pes equinus deformity) or spasticity of ankle plantar flexors | Upper motor neuron lesion/cerebral palsy, CVA | To maintain the weight over the foot, the knee and hip are kept in flexion throughout stance, leading to a “crouched gait”; requires short steps | |
| Initial contact is made with the forefoot, and the heel is brought to the ground by a posterior displacement of the tibia at midstance | Plantar flexion contracture (pes equinus deformity) or spasticity of ankle plantar flexors | Upper motor neuron lesion (cerebral palsy, CVA) Ankle fusion in a plantar flexed position |
Knee hyperextension occurs during stance owing to the inability of the tibia to move forward over the foot; hip flexion and excessive forward trunk lean during terminal stance occur to shift the weight of the body over the foot |
| Premature elevation of the heel in midstance or terminal stance | Lack of ankle dorsiflexion | Congenital or acquired muscular tightness of ankle plantar flexors | Characteristic bouncing gait pattern |
| Heel remains in contact with the ground late in terminal stance | Weakness or flaccid paralysis of plantar flexors with or without a fixed dorsiflexed position of the ankle (pes calcaneus deformity) | Peripheral or central nervous system disorders Excessive surgical lengthening of the Achilles tendon |
Excessive ankle dorsiflexion results in prolonged heel contact, reduced push off, and a shorter step length |
| Supinated foot position and weight bearing on the lateral aspect of the foot during stance | Pes cavus deformity | Congenital structural deformity | A high medial longitudinal arch is noted with reduced midfoot mobility throughout swing and stance |
| Excessive foot pronation occurs during stance with failure of the foot to supinate in mid stance; normal medial longitudinal arch noted during swing | Rearfoot varus and/or forefoot varus | Congenital or acquired structural deformity | Excessive foot pronation and associated flattening of the medial longitudinal arch may be accompanied by a general medial rotation of the lower extremity during stance |
| Excessive foot pronation with weight bearing on the medial portion of the foot during stance; the medial longitudinal arch remains absent during swing | Weakness (paralysis) of ankle invertors Pes planus deformity |
Upper motor neuron lesion Congenital structural deformity |
An overall excessive medial rotation of the lower extremity during stance is possible |
| Excessive inversion and plantar flexion of the foot and ankle occur during swing and at initial contact | Pes equinovarus due to spasticity of the plantar flexors and invertors | Upper motor neuron lesion (cerebral palsy, CVA) | Contact with the ground is made with the lateral border of the forefoot; weight-bearing on the lateral border of the foot during stance |
| Ankle remains plantar flexed during swing and can be associated with dragging of the toes, typically called drop foot | Weakness of dorsiflexors and/or pes equinus deformity | Common peroneal nerve palsy | Hip hiking, hip circumduction, or excessive hip and knee flexion of the swing leg or vaulting of the stance leg may be noted to lift the toes off the ground and prevent the toes from dragging during swing |
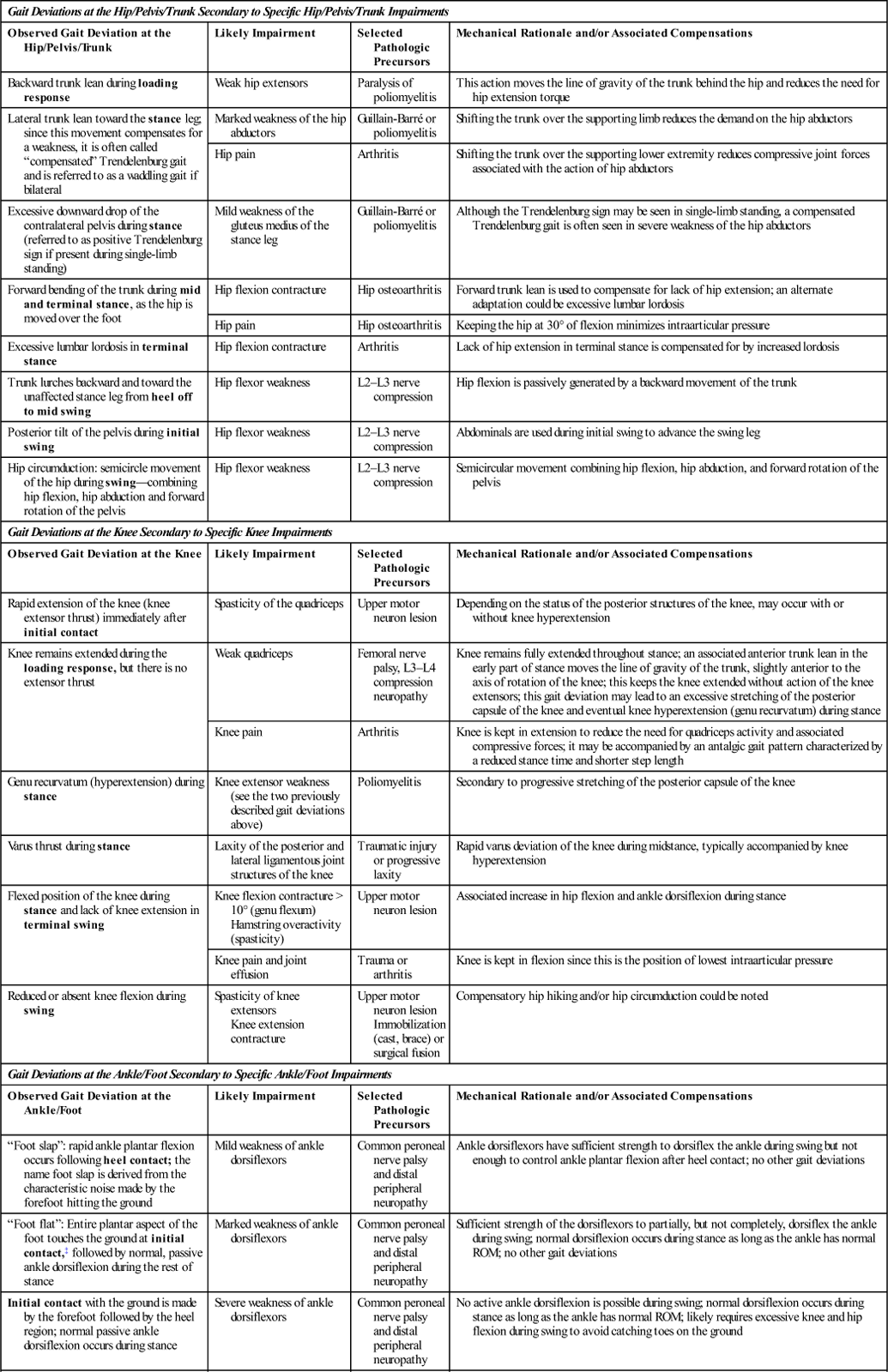
CVA, Cerebrovascular accident; ROM, range of motion.
*An impairment is a loss or an abnormality in physiologic, psychologic, or anatomic structure or function.
†Note: Terms in boldface indicate when in the gait cycle the gait deviation is expressed.
‡Initial contact is often used instead of heel contact to reflect the fact that with many gait deviations the heel is not the section of the foot that makes initial contact with the ground.
From Simoneau GG: Kinesiology of walking. In Neumann DA, editor: Kinesiology of the musculoskeletal system—foundations of physical rehabilitation, ed 2, St Louis, 2010, Mosby, pp. 665, 666, 668.
TABLE 14-7
Gait Deviations as a Compensation for a Lower Extremity Impairment*
| Gait Deviations Seen at the Hip/Pelvis/Trunk as a Compensation for an Impairment of the Ipsilateral Ankle, Ipsilateral Knee, or Contralateral Lower Extremity | ||
| Observed Gait Deviation at the Hip/Pelvis/Trunk | Likely Impairment | Mechanical Rationale |
| Forward bending of the trunk during the loading response | Weak quadriceps | Trunk is brought forward to move the line of gravity anterior to the axis of rotation of the knee, thereby reducing the need for knee extensors |
| Forward bending of the trunk during mid and terminal stance | Pes equinus deformity | Lack of ankle dorsiflexion during stance results in knee hyperextension and forward trunk lean to move the weight of the body over the stance foot |
| Excessive hip and knee flexion during swing | Often due to lack of ankle dorsiflexion of the swing leg; may also be due to a functionally or anatomically short contralateral stance leg | Used to clear the toes of the swing leg |
| Hip circumduction during swing | Lack of shortening of the swing leg secondary to reduced hip flexion, reduced knee flexion, and/or lack of ankle dorsiflexion | Used to lift the foot of the swing leg off the ground and provide toe clearance |
| Hip hiking (elevation of the ipsilateral pelvis during swing) | Lack of shortening of the swing leg secondary to reduced hip flexion, reduced knee flexion, and/or lack of ankle dorsiflexion Functionally or anatomically short stance leg |
Used to lift the foot of the swing leg off the ground and provide toe clearance |
| Excessive backward horizontal rotation of the pelvis on the side of the stance leg in terminal stance | Ankle plantar flexor weakness | Ankle plantar flexor weakness leads to prolonged heel contact and lack of push off; an increased pelvic horizontal rotation is used to lengthen the limb and maintain adequate step length |
| Gait Deviations Seen at the Knee as a Compensation for an Impairment of the Ipsilateral Ankle, Ipsilateral Hip, or Contralateral Lower Extremity | ||
| Observed Gait Deviation at the Knee | Likely Impairment | Mechanical Rationale |
| Knee is kept in flexion during stance despite the knee having normal ROM on examination | Impairments at the ankle or the hip, including a pes calcaneus deformity, plantar flexor weakness, and hip flexion contracture | Exaggerated ankle dorsiflexion or hip flexion during stance forces the knee in a flexed position; the contralateral (healthy) swing leg shows exaggerated hip and knee flexion to clear the toes owing to the functionally shorter stance leg |
| Hyperextension of the knee (genu recurvatum) from initial contact to pre swing | Ankle plantar flexion contracture (pes equinus deformity) or spasticity of ankle plantar flexors | Knee must hyperextend to compensate for the lack of forward displacement of the tibia during midstance |
| Antalgic gait | Painful stance leg | This is characterized by a shorter step length and stance time on the side of the painful lower extremity; it may be accompanied by ipsilateral trunk lean, if hip pain, contralateral trunk lean occurs with knee and foot pain |
| Excessive knee flexion in swing | Lack of ankle dorsiflexion of the swing leg or a short stance leg | Strategy to increase toe clearance of the swing leg and is typically accompanied by increased hip flexion |
| Gait Deviations Seen at the Ankle and Foot as a Compensation for an Impairment of the Ipsilateral Ankle, Ipsilateral Hip, or Contralateral Lower Extremity | ||
| Observed Gait Deviation at the Ankle/Foot | Likely Impairment | Mechanical Rationale |
| Vaulting: compensatory mechanism demonstrated by exaggerated ankle plantar flexion during midstance; leads to excessive vertical movement of the body | Any impairment of the contralateral lower extremity that reduces hip flexion, knee flexion, or ankle dorsiflexion during swing | Strategy used to allow the foot of a functionally long, contralateral lower extremity to clear the ground during swing |
| Excessive foot angle during stance that is called toeing-out | Retroversion of the neck of the femur or tight hip lateral rotators | Foot is in excessive toeing-out due to excessive lateral rotation of the lower extremity |
| Reduction of the normal foot ankle during stance that is called toeing-in | Excessive femoral anteversion or spasticity of the hip adductors and/or hip medial rotators | General medial rotation of the lower extremity |
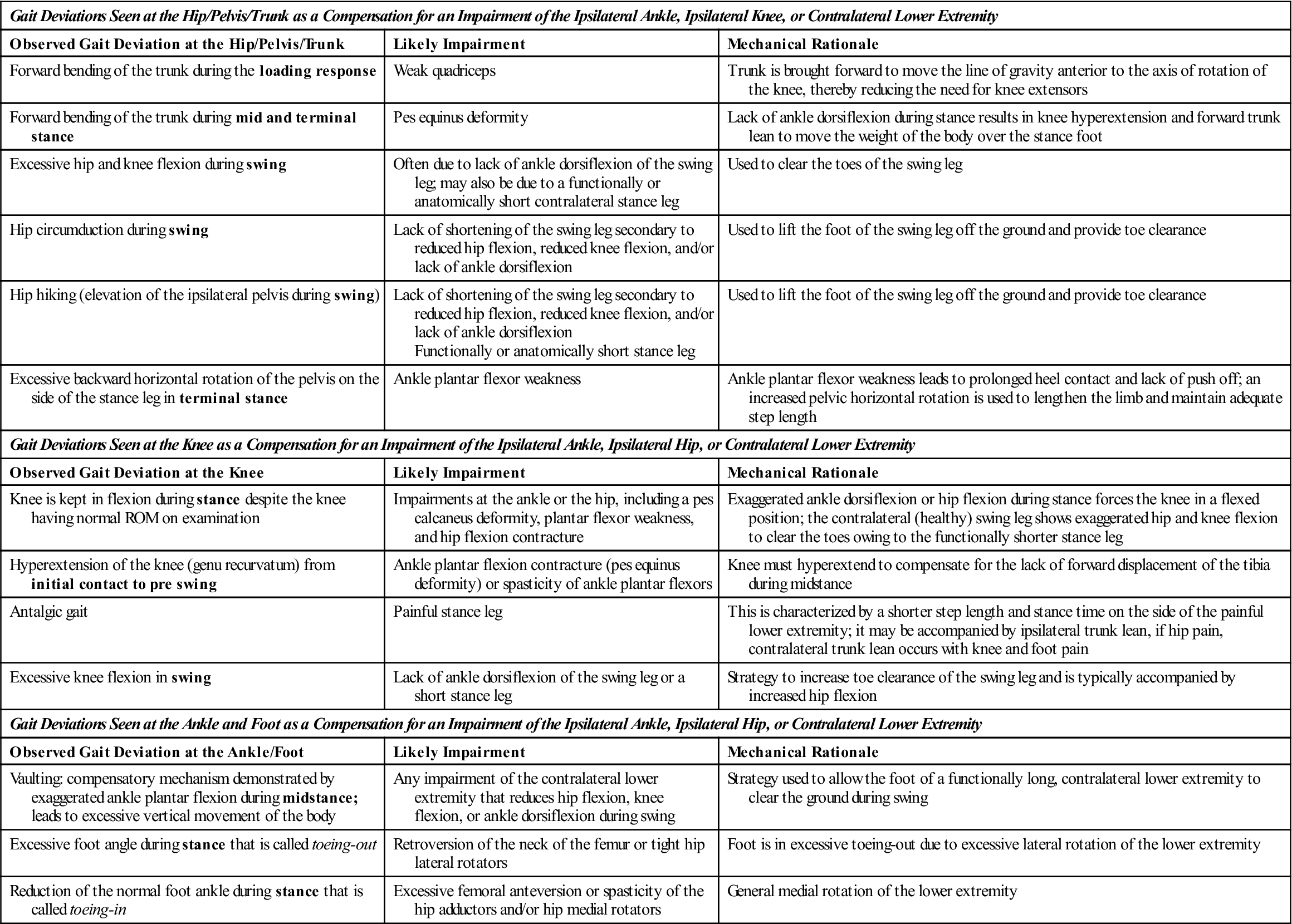
*Note: Terms in boldface indicate when in the gait cycle the gait deviation is expressed.
From Simoneau GG: Kinesiology of walking. In Neumann DA: Kinesiology of the musculoskeletal system—foundations of physical rehabilitation, ed 2, St Louis, 2010, Mosby, pp. 665–670.
Antalgic (Painful) Gait
The antalgic or painful gait is self-protective and is the result of injury to the pelvis, hip, knee, ankle, or foot. The stance phase on the affected leg is shorter than that on the nonaffected leg, because the patient attempts to remove weight from the affected leg as quickly as possible; therefore, the amount of time on each leg should be noted. The swing phase of the uninvolved leg is decreased. The result is a shorter step length on the uninvolved side, decreased walking velocity, and decreased cadence.36 In addition, the painful region is often supported by one hand, if it is within reach, and the other arm, acting as a counterbalance, is outstretched. If a painful hip is causing the problem, the patient also shifts the body weight over the painful hip. This shift decreases the pull of the abductor muscles, which decreases the pressure on the femoral head from more than two times the body weight to approximately body weight, owing to vertical instead of angular placement of the load over the hip. Flynn and Widmann have outlined some of the causes of a painful limp in children67 (Table 14-8).
TABLE 14-8
Differential Diagnosis of Antalgic Gait
| Less than 4 Years | 4 to 10 Years | More than 10 Years |
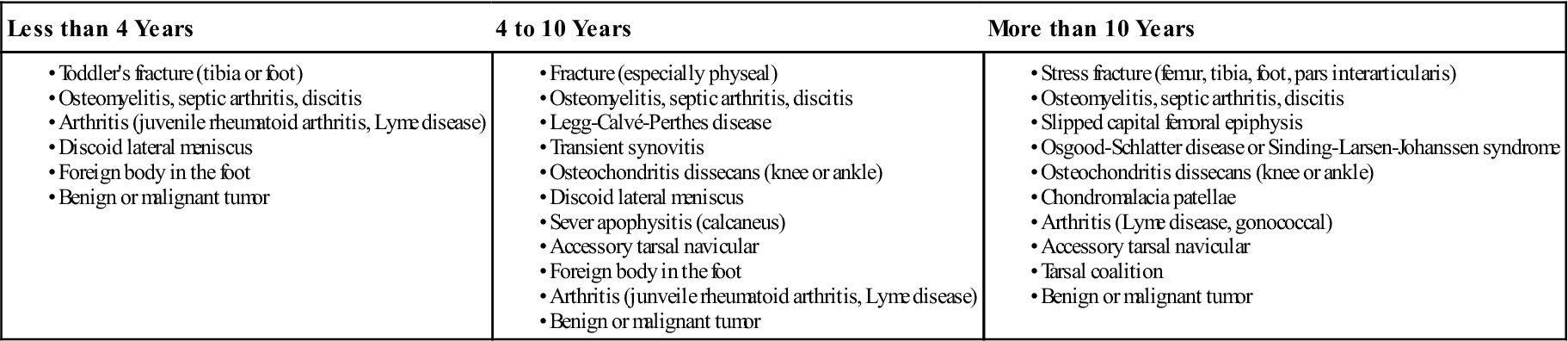
© 2001 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, vol 9(2), pp. 89–98.
Arthrogenic (Stiff Hip or Knee) Gait
The arthrogenic gait results from stiffness, laxity, or deformity, and it may be painful or pain free. If the knee or hip is fused or the knee has recently been removed from a cylinder cast, the pelvis must be elevated by exaggerated plantar flexion of the opposite ankle and circumduction of the stiff leg (circumducted gait) to provide toe clearance. The patient with this gait lifts the entire leg higher than normal to clear the ground because of a stiff hip or knee (Figure 14-18). The arc of movement helps to decrease the elevation needed to clear the affected leg. Because of the loss of flexibility in the hip, knee, or both, the gait lengths are different for the two legs. When the stiff limb is bearing weight, the gait length is usually smaller.
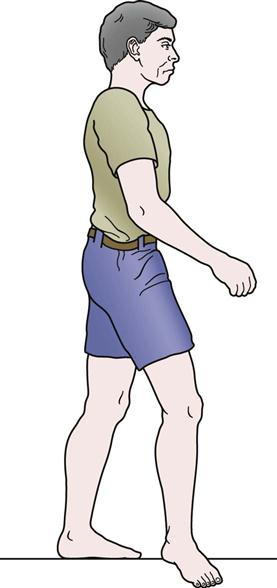
Ataxic Gait
If the patient has poor sensation or lacks muscle coordination, there is a tendency toward poor balance and a broad base (Figure 14-19). The gait of a person with cerebellar ataxia includes a lurch or stagger, and all movements are exaggerated. The feet of an individual with sensory ataxia slap the ground, because they cannot be felt. The patient also watches the feet while walking. The resulting gait is irregular, jerky, and weaving.
Contracture Gaits
Joints of the lower limb may exhibit contracture if immobilization has been prolonged or pathology to the joint has not been properly cared for. Hip flexion contracture often results in increased lumbar lordosis and extension of the trunk combined with knee flexion to get the foot on the ground. With a knee flexion contracture, the patient demonstrates excessive ankle dorsiflexion from late swing phase to early stance phase on the uninvolved leg and early heel rise on the involved side in terminal stance. Plantar flexion contracture at the ankle results in knee hyperextension (midstance of affected leg) and forward bending of the trunk with hip flexion (midstance to terminal stance of affected leg). Heel rise on the affected leg also occurs earlier.36
Equinus Gait (Toe Walking)
This childhood gait is seen with talipes equinovarus (club foot) (Table 14-9). Weight-bearing is primarily on the dorsolateral or lateral edge of the foot, depending on the degree of deformity. The weight-bearing phase on the affected limb is decreased, and a limp is present. The pelvis and femur are laterally rotated to partially compensate for tibial and foot medial rotation.2
TABLE 14-9
Differential Diagnosis of a Nonantalgic Limp
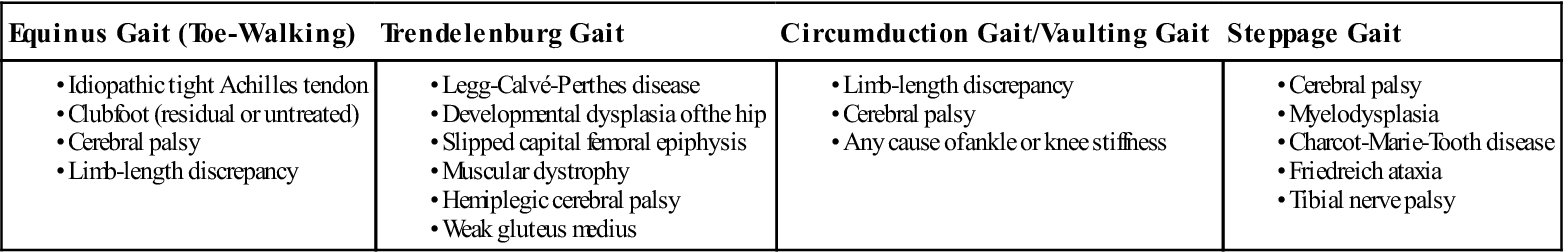
© 2001 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, vol 9(2), pp. 89–98.
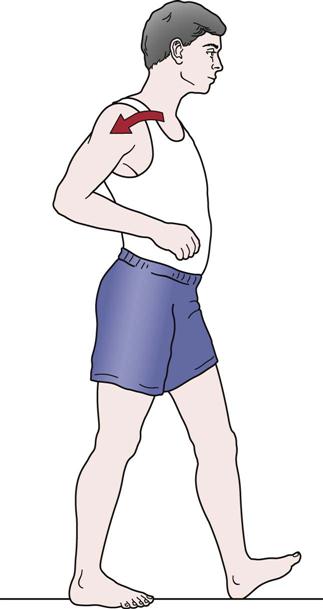
Gluteus Maximus Gait
If the gluteus maximus muscle, which is a primary hip extensor, is weak, the patient thrusts the thorax posteriorly at initial contact (heel strike) to maintain hip extension of the stance leg. The resulting gait involves a characteristic backward lurch of the trunk (Figure 14-20).
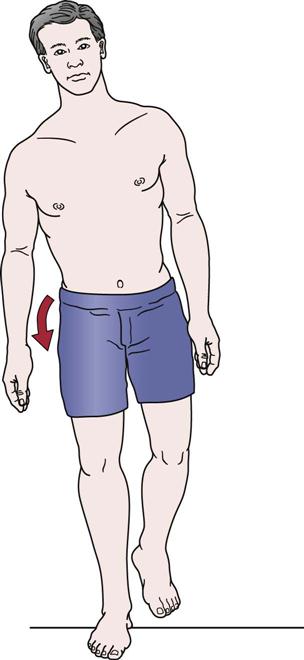
Gluteus Medius (Trendelenburg) Gait
If the hip abductor muscles (gluteus medius and minimus) are weak, the stabilizing effect of these muscles during stance phase is lost, and the patient exhibits an excessive lateral list in which the thorax is thrust laterally to keep the center of gravity over the stance leg (Figure 14-21). A positive Trendelenburg sign is also exhibited (i.e., the contralateral side droops because the ipsilateral hip abductors do not stabilize or prevent the droop). If there is bilateral weakness of the gluteus medius muscles, the gait shows accentuated side-to-side movement, resulting in a wobbling gait or “chorus girl swing.” This gait may also be seen in patients with congenital dislocation of the hip and coxa vara (see Table 14-9).

Hemiplegic or Hemiparetic Gait
The patient with hemiplegic or hemiparetic gait swings the paraplegic leg outward and ahead in a circle (circumduction) or pushes it ahead (Figure 14-22). In addition, the affected upper limb is carried across the trunk for balance. This is sometimes referred to as a neurogenic or flaccid gait.
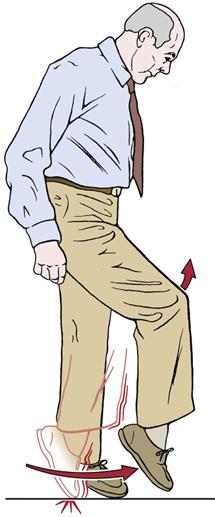
Parkinsonian Gait
The neck, trunk, and knees of a patient with parkinsonian gait are flexed. The gait is characterized by shuffling or short rapid steps (marche à petits pas) at times. The arms are held stiffly and do not have their normal associative movement (Figure 14-23). During the gait, the patient may lean forward and walk progressively faster as though unable to stop (festination).68
Plantar Flexor Gait
If the plantar flexor muscles are unable to perform their function, ankle and knee stability are greatly affected. Loss of the plantar flexors results in decrease or absence of push-off. The stance phase is less, and there is a shorter step length on the unaffected side.36
Psoatic Limp
The psoatic limp is seen in patients with conditions affecting the hip, such as Legg-Calvé-Perthes disease. The patient demonstrates a difficulty in swing-through, and the limp may be accompanied by exaggerated trunk and pelvic movement.36 The limp may be caused by weakness or reflex inhibition of the psoas major muscle. Classic manifestations of this limp are lateral rotation, flexion, and adduction of the hip (Figure 14-24). The patient exaggerates movement of the pelvis and trunk to help move the thigh into flexion.
Quadriceps Avoidance Gait
If the quadriceps muscles have been injured (e.g., femoral nerve neuropathy, reflex inhibition, trauma—3°strain), the patient compensates in the trunk and lower leg. Forward flexion of the trunk combined with strong ankle plantar flexion causes the knee to extend (hyperextend). The knee may be held extended by using the iliotibial band. If the trunk, hip flexors, and ankle muscles cannot perform this movement, the patient may use a hand to extend the knee.36
Scissors Gait
This gait is the result of spastic paralysis of the hip adductor muscles, which causes the knees to be drawn together so that the legs can be swung forward only with great effort (Figure 14-25). This is seen in spastic paraplegics and may be referred to as a neurogenic or spastic gait.
Short Leg Gait
If one leg is shorter than the other or there is a deformity in one of the bones of the leg, the patient may demonstrate a lateral shift to the affected side, and the pelvis tilts down on the affected side, creating a limp (Figure 14-26). The patient may also supinate the foot on the affected side to try to “lengthen” the limb. The joints of the unaffected limb may demonstrate exaggerated flexion, or hip hiking may occur during the swing phase to allow the foot to clear the ground.36 The weight-bearing period may be the same for the two legs. How a patient adapts for leg length difference has wide variability.69,70 With proper footwear, the gait may appear normal. This gait may also be termed painless osteogenic gait.
Steppage or Drop Foot Gait
The patient with a steppage gait has weak or paralyzed dorsiflexor muscles, resulting in a drop foot. To compensate and avoid dragging the toes against the ground, the patient lifts the knee higher than normal (Figure 14-27). At initial contact, the foot slaps on the ground because of loss of control of the dorsiflexor muscles resulting from injury to the muscles, their peripheral nerve supply, or the nerve roots supplying the muscles (see Table 14-9).71
Table 14-10 lists common gait pathologies that can modify gait and the phase in which the deviation occurs.38
TABLE 14-10
| Deviation | Phase | Cause |
| Excessive foot pronation | Midstance through toe off | Compensated forefoot or rearfoot varus deformity; uncompensated forefoot valgus deformity; pes planus; decreased ankle dorsiflexion; increased tibial varum; long limb; uncompensated medial rotation of tibia or femur; weak tibialis posterior |
| Excessive foot supination | Heel strike through midstance | Compensated forefoot valgus deformity; pes cavus; short limb, uncompensated lateral rotation of tibia or femur; limited calcaneal eversion; plantar flexed first ray; upper motor neuron muscle balance |
| Excessive calcaneal eversion | Initial contact through midstance | Excessive tibia vara; forefoot varus; tibialis posterior weakness; excessive lower extremity medial rotation (due to muscle imbalances, femoral anteversion) |
| Excessive varus | Heel strike to toe off | Contracture; overactivity of muscles on medial aspect of foot |
| Excessive valgus | Heel strike to toe off | Weak invertors; foot hypermobility |
| Bouncing or exaggerated plantar flexion | Midstance through toe off | Heel cord contracture; increased tone of gastrocnemius and soleus |
| Excessive dorsiflexion | Heel strike to toe off | Compensation for knee flexion contracture; inadequate plantar flexor strength; adaptive shortening of dorsiflexors; increased muscle tone of dorsiflexors; pes calcaneus deformity |
| Insufficient push-off | Midstance through toe off | Gastrocnemius and soleus weakness; Achilles tendon rupture; metatarsalgia; hallux rigidus |
| Foot slap | Heel strike to foot flat | Dorsiflexor weakness; lack of lower limb sensation |
| Steppage gait (exaggerated hip and knee flexion to clear foot) | Acceleration through deceleration | Dorsiflexor weakness or paralysis; functional leg length discrepancy |
| Excessive knee flexion | Heel strike through toe off | Hamstring contracture; decreased ROM in ankle dorsiflexion; plantar flexor muscle weakness; lengthened limb; hip flexion contracture |
| Excessive knee extension/inadequate knee flexion | Heel strike to foot flat, and swing | Pain; anterior trunk deviation/bending; weakness of quadriceps, hyperextension is a compensation and places body weight vector anterior to knee; spasticity of the quadriceps, noted more during the loading response and during initial swing intervals; joint deformity |
| Genu recurvatum (knee hyperextension) | Heel strike through midstance | Quadriceps femoris weak or short; compensated hamstring weakness; Achilles tendon contracture; habit |
| Abnormal internal hip rotation (“toe-in” gait) | Adaptive shortening of iliotibial band; weakness of hip lateral rotators; femoral anteversion; adaptive shortening of hip medial rotators | |
| Abnormal external hip rotation (“toe-out” gait) | Adaptive shortening of hip lateral rotators; femoral retroversion; weakness of hip medial rotators | |
| Increased hip adduction (scissors gait) | Heel strike to toe off | Spasticity or contracture of ipsilateral hip adductors; ipsilateral hip adductor weakness; coxa vara |
| Decreased hip swing through (psoatic limp) | Legg-Calvé-Perthes disease; weakness or reflex inhibition of psoas major muscle; pain | |
| Excessive medial or lateral femur rotation (femoral torsion) | Heel strike through toe off | Medial or lateral hamstrings tight, respectively; opposite muscle group weakness; anteversion or retroversion, respectively |
| Increased base of support (> 4 inches/10 cm) | Heel strike through toe off | Abductor muscle contracture; instability; genu valgum; leg length discrepancy; fear of losing balance |
| Decreased base of support (< 2 inches/5 cm) | Heel strike through toe off | Adductor muscle contracture; genu varum |
| Circumduction | Acceleration through deceleration | Increased limb length; abductor muscle shortening or overuse; stiff hip or knee |
| Hip hiking | Acceleration through deceleration | Increased limb length; hamstring weakness; inadequate hip or knee flexion or ankle dorsiflexion; quadratus lumborum shortening |
| Vaulting (ground clearance of swinging leg is increased if subject goes up on toes of stance period leg) | Foot flat to toe off | Functional leg-length discrepancy; vaulting occurs on shorter limb side |
| Inadequate hip flexion | Acceleration through heel strike | Hip flexor muscle weakness; hip extensor muscle shortening; increased limb length; hip joint arthrosis |
| Inadequate hip extension (causes trunk forward bending, increased lordosis) | Midstance through toe off | Hip flexion contracture; hip extensor muscle weakness; iliotibial band contracture; hip flexor spasticity; pain |
| Increased lumbar lordosis | Foot flat to toe off | Inability to extend hip; hip flexion contracture or hip ankylosis |
| Excessive trunk back bending (gluteus maximus gait) | Heel strike through midstance | Hip extensor or flexor muscle weakness; hip pain; decreased ROM of knee |
| Excessive trunk forward bending | Deceleration through midstance | Quadriceps femoris and gluteus maximus weakness; decreased ankle dorsiflexion; hip flexion contracture |
| Excessive trunk lateral flexion (compensated Trendelenburg gait) | Foot flat through heel off | Gluteus medius weakness; hip pain; unequal leg length; hip pathology; wide base |
| Pelvic drop | Foot flat through heel off | Contralateral gluteus medius weakness; adaptive shortening of quadratus lumborum; contralateral hip adductor spasticity |
| Excessive pelvic rotation | Heel strike to toe off | Adaptively shortened/spasticity of hip flexors on same side; limited hip joint flexion |
| Slower cadence than expected for person’s age | Generalized weakness; pain; joint motion restrictions; poor voluntary motor control | |
| Shorter stance phase on involved side and decreased swing phase on uninvolved side (shorter stride length on uninvolved side, decrease lateral sway over involved stance limb, decrease in cadence, decrease in velocity, use of assistive device) | Antalgic gait resulting from painful injury to lower limb and pelvic region | |
| Stance phase longer on one side | Pain; lack of trunk and pelvic rotation; weakness of lower limb muscles; restrictions in lower limb joints; poor muscle control; increased muscle tone |
Adapted from Giallonardo LM: Gait. In Myers RS, editor: Saunders manual of physical therapy practice, Philadelphia, 1995, WB Saunders, p. 1112; and Dutton M: Orthopedic examination, evaluation and intervention, New York, 2004, McGraw-Hill.